Anemia Drugs: Hematopoiesis & Iron Deficiency Presentation
advertisement

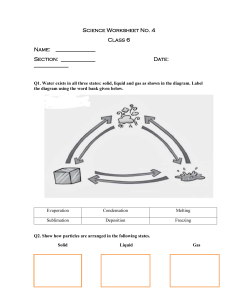
Chapter 54 ANEMIA DRUGS Hematopoiesis Formation of new blood cells Red blood cells (RBCs) Erythropoiesis White blood cells (WBCs) Platelets 2 Hematopoiesis (Cont.) RBCs Manufactured Immature Lifespan in bone marrow RBCs are reticulocytes. is 120 days. More than one third of an RBC is made of hemoglobin. Heme: red pigment, contains iron Globin: protein chain 3 Anemias 4 Maturation defects Cytoplasmic Nuclear Excessive destruction of RBCs (hemolytic anemias) Intrinsic RBC abnormalities Extrinsic mechanisms Underlying causes of anemia are red blood cell (RBC) maturation defects and factors secondary to excessive RBC destruction. Iron 5 Essential mineral in the body Oxygen carrier in hemoglobin and myoglobin Stored in the liver, spleen, and bone marrow Iron deficiency results in anemia. Dietary sources: meats, certain vegetables, and grains Dietary iron must be converted by gastric juices before it can be absorbed. Iron (Cont.) Some foods enhance iron absorption: Orange juice Veal Fish Ascorbic acid Some foods impair iron absorption: Eggs* Corn Beans* Cereal products containing phytates * Also common dietary sources of iron. 6 Iron: Indications 7 Prevention and treatment of iron-deficiency syndromes Administration of iron alleviates the symptoms of irondeficiency anemia, but the underlying cause of the anemia should be corrected. Causes nausea, vomiting, diarrhea, constipation, and stomach cramps and pain Causes black, tarry stools Liquid oral preparations may stain teeth. Injectable forms cause pain upon injection. Iron Toxicity 8 Symptomatic and supportive measures Suction and maintenance of the airway; correction of acidosis; control of shock and dehydration with IV fluids or blood, oxygen, and vasopressors In patients with severe symptoms of iron intoxication, such as coma, shock, or seizures, chelation therapy with deferoxamine is initiated. Iron Preparations PROTOTYPE MEDICATIONS Oral: Ferrous sulfate Parenteral: Iron dextran OTHER MEDICATIONS Oral: Ferrous gluconate, ferrous fumarate Parenteral: (SFGC) Ferumoxytol, iron sucrose, sodium-ferric gluconate complex Iron Therapeutics Ferumoxytol For patients with chronic kidney disease Ferumoxytol requires only two doses over 3 to 8 days compared with SFGC and iron sucrose, which require 3 to 10 doses over several weeks. SFGC For patients undergoing long-term hemodialysis 3-10 doses given over several weeks Parenteral Iron 11 Iron dextran (INFeD, Dexferrum) May cause anaphylactic reactions, including major orthostatic hypotension and fatal anaphylaxis A test dose of 25 mg of iron dextran is administered before injection of the full dose, and then the remainder of dose is given after 1 hour. Used less frequently now; replaced by newer products ferric gluconate and iron sucrose Iron Therapeutics (Cont’d) Iron sucrose Patients who have chronic kidney disease, are receiving erythropoietin, and are hemodialysis- or peritoneal dialysis-dependent Patients who have chronic kidney disease, are not receiving erythropoietin, and are not dialysis-dependent 3-10 doses given over several weeks Injectable Iron: Iron Sucrose Venofer Indicated for anemic patients with chronic renal failure Less risk for precipitating anaphylaxis than with iron dextran No test dose required Adverse effects: hypotension (related to infusion rates) Infuse over 2.5 to 3.5 hours Erythropoiesis-Stimulating Agents 14 Epoetin alfa (Epogen) Biosynthetic form of the natural hormone erythropoietin Used for treatment of anemia associated with end-stage renal disease, chemotherapy-induced anemia, and anemia associated with zidovudine therapy Medication is ineffective without adequate body iron stores and bone marrow function. Most patients receiving epoetin alfa need to also receive an oral or intravenous (IV) iron preparation. Erythropoiesis-Stimulating Agents 15 Epoetin alfa (Epogen) Longer acting form of epoetin called darbepoetin (Aranesp) Contraindications: drug allergy, uncontrolled hypertension, hemoglobin levels are above 10 g/dL for cancer patients and 11 g/dL for renal patients, head and neck cancers, risk of thrombosis. Most frequent adverse effects: hypertension, fever, headache, pruritus, rash, nausea, vomiting, arthralgia, and injection site reaction Complications GI distress (nausea, constipation, heartburn) Teeth staining (liquid form) Staining of skin and other tissues (IM injections) Anaphylaxis Hypotension Folic Acid (Folate) Water-soluble, B-complex vitamin Essential for erythropoiesis Primary uses Folic acid deficiency During 17 pregnancy to prevent neural tube defects Malabsorption syndromes are the most common causes of deficiency. Folic Acid (Cont.) 18 Should not be used until actual cause of anemia is determined May mask symptoms of pernicious anemia, which requires treatment other than folic acid Untreated pernicious anemia progresses to neurologic damage. Mechanism of Action 19 Folic acid is converted in the body to tetrahydrofolic acid which is used for erythropoiesis and for synthesis of nucleic acids. Not active in the ingested form and must be converted for reactions to occur Contraindications/Precau tions Patients with previous hypersensitivity to iron Anemias other than iron-deficiency anemia Oral Use with caution in clients who have peptic ulcer disease, regional enteritis, ulcerative colitis, and severe liver disease Antacids or tetracyclines Caffeine and dairy products Food Iron Nursing Care Take on an empty stomach Take with food if GI adverse effects occur Space doses Teach patient to anticipate a harmless dark green or black color of stool Proper PO administration of liquid iron preparation Increase water and fiber intake (unless contraindicated) Maintain an exercise program Therapy can last 1 to 2 months Dietary considerations Nursing Evaluation of Iron Increased reticulocyte count Hemoglobin Fatigue and pallor subside Increased energy level