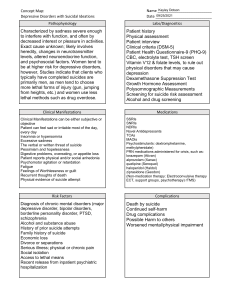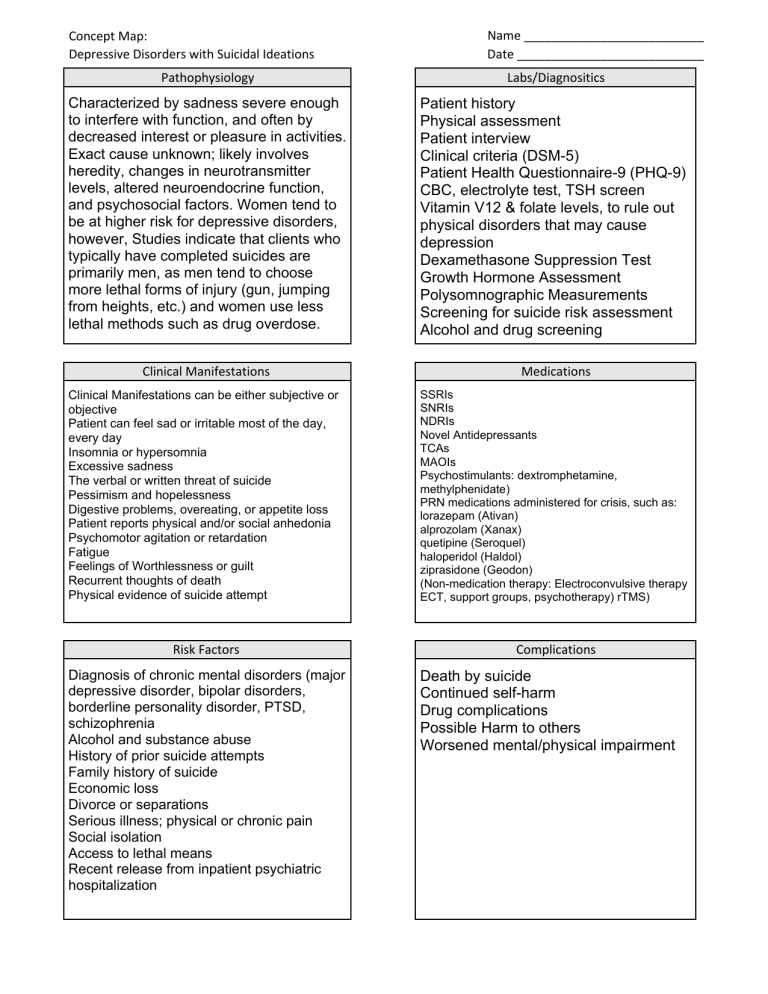
Concept Map: Depressive Disorders with Suicidal Ideations Name __________________________ Date ___________________________ Pathophysiology Labs/Diagnositics Characterized by sadness severe enough to interfere with function, and often by decreased interest or pleasure in activities. Exact cause unknown; likely involves heredity, changes in neurotransmitter levels, altered neuroendocrine function, and psychosocial factors. Women tend to be at higher risk for depressive disorders, however, Studies indicate that clients who typically have completed suicides are primarily men, as men tend to choose more lethal forms of injury (gun, jumping from heights, etc.) and women use less lethal methods such as drug overdose. Patient history Physical assessment Patient interview Clinical criteria (DSM-5) Patient Health Questionnaire-9 (PHQ-9) CBC, electrolyte test, TSH screen Vitamin V12 & folate levels, to rule out physical disorders that may cause depression Dexamethasone Suppression Test Growth Hormone Assessment Polysomnographic Measurements Screening for suicide risk assessment Alcohol and drug screening Clinical Manifestations Medications Clinical Manifestations can be either subjective or objective Patient can feel sad or irritable most of the day, every day Insomnia or hypersomnia Excessive sadness The verbal or written threat of suicide Pessimism and hopelessness Digestive problems, overeating, or appetite loss Patient reports physical and/or social anhedonia Psychomotor agitation or retardation Fatigue Feelings of Worthlessness or guilt Recurrent thoughts of death Physical evidence of suicide attempt SSRIs SNRIs NDRIs Novel Antidepressants TCAs MAOIs Psychostimulants: dextromphetamine, methylphenidate) PRN medications administered for crisis, such as: lorazepam (Ativan) alprozolam (Xanax) quetipine (Seroquel) haloperidol (Haldol) ziprasidone (Geodon) (Non-medication therapy: Electroconvulsive therapy ECT, support groups, psychotherapy) rTMS) Risk Factors Complications Diagnosis of chronic mental disorders (major depressive disorder, bipolar disorders, borderline personality disorder, PTSD, schizophrenia Alcohol and substance abuse History of prior suicide attempts Family history of suicide Economic loss Divorce or separations Serious illness; physical or chronic pain Social isolation Access to lethal means Recent release from inpatient psychiatric hospitalization Death by suicide Continued self-harm Drug complications Possible Harm to others Worsened mental/physical impairment Concept Map: Depressive Disorders with Suicidal Ideations Nursing Assessment Past health history, current medications Past surgical history Perform neurological assessment Patient Health Questionnaire-9 Perform screening for suicide risk assessment Obtain history from client and family members Kayley Dotson Name __________________________ 09/25/2021 Date ___________________________ Nursing Concepts Interpersonal violence Mood and loss Stress and coping Fatigue Psychosis Self-concept Self-management Adherence Anxiety Patient education Nursing Outcomes Nursing Interventions Patient will remain free from self-harm during hospitalization Patient will seek help when experiencing self-destructive impulses Patient will verbalize 3 techniques on developing coping skills to help handle stressful situations Patient will explore suicidal thoughts with staff Patient will contract for safety with nurse every night shift Patient will connect suicidal thoughts to current stressors Patient will demonstrate compliance with any medication or treatment plan within the next two weeks Initiate one-on-one monitoring at arm’s length per facility protocol. Avoid leaving client unattended for any reason Educate and listen to the patient about reasons why they want to self-harm Create a safe environment by removing potential weapons or objects that may inflict harm (weapons, utensils, sharp objects, belts, ties, etc.) Encourage the client to discuss feelings, emotions, fears and anxieties and alternative ways to cope with those feelings Assess for signs that the client has a plan to commit suicide Educate the patient on 3 techniques on developing coping skills to help the patient handle stressful situations Create a verbal or written contract, stating that patient will not act on impulse to do self-harm Identify situations or triggers and ineffective coping behaviors that may result in suicidal thoughts or actions Administer medications carefully and appropriately Provide resource information for support groups, hotlines, and counselors that are available 24/7 Evaluation Maintained safe environment by removing potential harmful objects from patients room Patient discussed feelings, emotions, and anxieties and verbalized different ways to cope with stressors Patient signed written contract, stating patient will not act on impulse to do self-harm Patient verbalized importance of appropriately taking prescribed medications Provided resource information for local support groups and 24/7 hotlines in time of crisis