Benito et al., 2015
advertisement

J Appl Physiol 118: 1006–1013, 2015.
First published February 26, 2015; doi:10.1152/japplphysiol.00928.2014.
Change in weight and body composition in obese subjects following a
hypocaloric diet plus different training programs or physical activity
recommendations
Pedro J. Benito,1* Laura M. Bermejo,2* Ana B. Peinado,1 Bricia López-Plaza,2 Rocío Cupeiro,1,3
Barbara Szendrei,1 Francisco J. Calderón,1 Eliane A. Castro,1 and Carmen Gómez-Candela,2 on behalf of
the PRONAF Study Group
1
Laboratorio de Fisiología del Esfuerzo Research Group, Department of Health and Human Performance, Faculty of
Physical Activity and Sport Sciences, Technical University of Madrid, Madrid, Spain; 2Department of Nutrition, Hospital La
Paz Health Research Institute, La Paz University Hospital, Madrid, Spain; and 3Faculty of Law and Social Sciences,
Universidad Francisco de Vitoria, Pozuelo de Alarcón, Spain
Submitted 15 October 2014; accepted in final form 13 February 2015
Benito PJ, Bermejo LM, Peinado AB, López-Plaza B, Cupeiro
R, Szendrei B, Calderón FJ, Castro EA, Gómez-Candela C on
behalf of the PRONAF Study Group Change in weight and body
composition in obese subjects following a hypocaloric diet plus
different training programs or physical activity recommendations. J
Appl Physiol 118: 1006 –1013, 2015. First published February 26,
2015; doi:10.1152/japplphysiol.00928.2014.—The aim of the present
study was to compare the effects of different physical activity programs, in combination with a hypocaloric diet, on anthropometric
variables and body composition in obese subjects. Ninety-six obese
(men: n ⫽ 48; women: n ⫽ 48; age range: 18-50 yr) participated in a
supervised 22-wk program. They were randomized into four groups:
strength training (S; n ⫽ 24), endurance training (E; n ⫽ 26),
combined strength ⫹ endurance training (SE; n ⫽ 24), and physical
activity recommendations (C; n ⫽ 22). In addition, all groups followed the same hypocaloric diet. At baseline and at the end of the
intervention, dietetic and physical activity variables were assessed
using validated questionnaires. Anthropometric variables were recorded along with body composition variables measured using dualenergy X-ray absorptiometry techniques. At the end of the intervention, significant improvements were seen within groups in terms of
body weight (S: ⫺9.21 ⫾ 0.83 kg; E: ⫺10.55 ⫾ 0.80 kg; SE: ⫺9.88
⫾ 0.85 kg; C: ⫺8.69 ⫾ 0.89 kg), and total fat mass (S: ⫺5.24 ⫾
0.55%; E: ⫺5.35 ⫾ 0.55%; SE: ⫺4.85 ⫾ 0.56%; C: ⫺4.89 ⫾ 0.59%).
No differences were seen between groups at this time in terms of any
other anthropometric or body composition variables examined. All
groups increased their total physical activity in metabolic equivalents
(MET) per week during the intervention, but with no difference
between groups (S: 976 ⫾ 367 MET-min/wk; E: 954 ⫾ 355 METmin/wk; SE: 1 329 ⫾ 345 MET-min/wk; C: 763 ⫾ 410 MET-min/
wk). This study shows that, when combined with a hypocaloric diet,
exercise training and adherence to physical activity recommendations
are equally effective at reducing body weight and modifying body
composition
in the treatment of obesity (Clinical Trials Gov. number:
NCT01116856).
physical activity; aerobic exercise; strength training; dietary modification; body composition
studies indicate excess body
weight during midlife to be associated with an increased risk of
THE MAJORITY OF EPIDEMIOLOGICAL
* P. J. Benito and L. M. Bermejo contributed equally to this work.
Address for reprint requests and other correspondence: P. J. B. Peinado, Dept.
of Health and Human Performance, Technical Univ. of Madrid, C/Martín Fierro 7,
28040 Madrid, Spain (e-mail: pedroj.benito@upm.es).
1006
all-cause mortality (1, 9, 33). For example, people with a body
mass index (BMI) of 25–28.9 have a relative risk of developing
cardiovascular disease twice that of people with a BMI of ⬍21
kg/m2, while those with a BMI of ⱖ29 kg/m2 are at almost
three times the risk (36). Further, the results of the Framingham
Heart Study show that being overweight at age 40 reduces life
expectancy by 3 yr (24). In Spain, the prevalence of obesity
in 2011 was 22.9% (24.4% in men and 21.4% in women)
and about 36% of adults had abdominal obesity (32% of
men and 39% of women) (11). Finding efficient treatments
for midlife obesity should, therefore, be seen as a public
health priority (4).
The treatment of obesity includes low-calorie, low-fat diets,
increased physical activity, and lifestyle modification strategies
(12, 18). Current evidence indicates that the best diet for
prevention of weight gain, obesity, Type 2 diabetes, and
cardiovascular disease is one low in fat and sugary beverages
and high in carbohydrates, fiber, grains, and protein (3).
Physical activity is also widely recognized as a means of
achieving the primary prevention of chronic diseases (10).
Increasing physical activity, in addition to following a balanced diet, however, is crucial in any program designed to
combat obesity (34). Despite the benefits of regular physical
activity, the percentage of physically inactive adults in the
world is high. The World Health Report of the World Health
Organization (WHO) (2003) states that, worldwide, more than
60% of adults can be classified as inactive (10).
A combination of energy restriction and increased energy
output by means of exercise has been proven as a means of
treating obesity in the hospital setting (7). Indeed, the results
have been quite conclusive with respect to the undertaking of
aerobic exercise and the following of a very restrictive energy
intake (i.e., ⬍50% of that normally recommended) (15, 25).
However, data are still scarce regarding the effect on weight
loss of combining strength and aerobic training with a much
less restrictive hypocaloric diet (15). Those trials that have
been performed have varied in terms of intensity, delivery
methods, target groups, and study components; the comparisons that can be made among them are, therefore, necessarily
limited. It has now become essential that effective, physical
activity interventions be developed on the basis of good scientific evidence (19, 21).
Within the framework of the Global Strategy on Diet,
Physical Activity and Health, the WHO has stated that health
8750-7587/15 Copyright © 2015 the American Physiological Society
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
http://www.jappl.org
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
should be protected and promoted by guiding the development
of an enabling environment for sustainable actions at the
individual, community, national, and global level, such that,
when followed together, these might lead to reduced disease
and death rates related to unhealthy diet and physical inactivity
(35). Accordingly, the project “Nutrition and Physical Activity
Programs for Obesity Treatment” (the PRONAF study according to its Spanish initials) was designed. Its main aim is to
discover, via the undertaking of two randomized clinical trials,
which physical activity protocol, in combination with a hypocaloric diet, is the most effective for the treatment of overweight and obesity. As part of this project, the present work
compares the effects of different physical activity programs, in
combination with a hypocaloric diet, on body weight and body
composition in obese subjects.
MATERIALS AND METHODS
Participants
Detailed information on the materials and methods used in the
wider PRONAF study can be obtained from a previous paper (39). In
the present work, participants were sought via advertisements posted
in newspapers and announced on the radio, the Internet, and TV. The
eligible sample population consisted of 120 obese subjects (59 women
and 61 men; age range: 18 –50 years; BMI: ⱖ30 to ⬍34.9 kg/m2)
living in the region of Madrid, Spain. All subjects were healthy adults
with no history of important concomitant illness (heart, lung, or liver
disease, or neoplasms). All were normoglycemic, nonsmokers, and
took no medications or drugs, but all led sedentary lifestyles. All
female subjects had regular menstrual cycles. The exclusion criteria
covered all physical and psychological diseases that may have precluded the performance of the requested strength or endurance training, along with the taking of any medication known to influence
physical performance or that might interfere with the interpretation of
the results. Subjects with a background of systematic strength or
endurance training (moderate to high-intensity training more than
once a week) in the year before the study started were also excluded.
In agreement with the guidelines of the Declaration of Helsinki
regarding research on human subjects, all participants signed an
institutionally approved document of informed consent. All subjects
were carefully informed about the possible risks and benefits of the
study, which was approved by the Human Research Review Committee of the La Paz University Hospital (PI-643). This trial was registered at clinical trials.gov as NCT01116856. http://clinicaltrials.gov/.
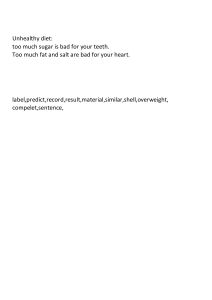
Figure 1 shows the participant flowchart in the study.
Study Design
Subjects who fulfilled the inclusion criteria and passed a baseline
physical examination were stratified by age and sex and assigned
(using a randomization table) to a strength training group (S; n ⫽ 30),
an endurance training group (E; n ⫽ 30), a combined strength ⫹
endurance training group (SE; n ⫽ 30), or a physical activity recommendations group (control group, C; n ⫽ 30).
Hypocaloric diets were prescribed individually for all participants.
This study design was that of an intervention trial of 22 wk duration.
Baseline measurements for all subjects were made before starting the
intervention period. The final measurements were taken once the
intervention period was over (within 48 –72 h of the last training
session for the exercise groups).
Exercise Programs
The different exercise training groups (E, S, SE) followed their
corresponding training programs, which in all cases involved training
•
Benito PJ et al.
1007
3 times/wk for 22 wk. All training sessions were carefully supervised
by certified personal trainers.
The S group followed a circuit involving eight exercises: the
shoulder press, squats, the barbell row, the lateral split, bench press,
front split and biceps curl, and the French press for triceps. Running,
cycling, or elliptical (self-selected) exercises were the main components of the session for group E, while group SE followed a combination of cycle ergometry, treadmill, or elliptical exercises intercalated with squats, rowing machine, bench presses, and front split
exercises (15 lifts per set or 45 s for the SE endurance phase). The C
subjects followed the hospital’s habitual clinical practice for achieving weight loss: dietary intervention—the same as followed by the
exercise training groups—plus being made aware of the general
recommendations of the American College of Sports Medicine regarding physical activity. Thus, the C subjects were advised to
undertake at least 200 –300 min of moderate-intensity physical activity per week (30 – 60 min on most, if not all, days of the week) (8). The
C subjects were also advised to reduce their sedentary behavior (e.g.,
watching television or using the computer) and increase daily activities, such as brisk walking or cycling instead of using a car, or
climbing stairs instead of using the elevator (32).
The exercise-training programs were designed to take into account
each subject’s muscular strength (MS) and heart rate reserve (HRR as
the difference between resting HR and maximal HR). MS was
measured in the strength program subjects (S, SE) using the 15repetition maximum (15 RM) testing method every other day during
the week before the intervention period. The HRR was calculated to
set the exercise intensity [(maximum heart rate-resting heart rate)
50 – 60%] for the E and SE subjects. The volume and intensity of the
three training programs were equal and increased progressively during
the study. In weeks 2–5, exercise was at an intensity of 50% of the 15
RM and HRR and lasted an overall 51 min and 15 s. In weeks 6 –14,
exercise was performed at an intensity of 60% of 15 RM and HRR,
again with a duration of 51 min and 15 s. Finally, in weeks 15–22,
exercise was performed at an intensity of 60% of 15 RM and HRR,
with a duration of 60 min. Each training session for the S, E, and SE
subjects commenced with a 5-min aerobic warm-up, followed by the
main session exercises, and concluded with 5 min of cooling down
and stretching exercises. In all sessions, the exercise rhythm was
controlled by instructions recorded on a compact disk.
Hypocaloric Diet Program
Hypocaloric diets (between 5,028 and 12,570 kJ) were prescribed
individually for all participants by expert dieticians at the Department
of Nutrition, La Paz University Hospital, Madrid. The diet was
designed to provide 30% less energy than the baseline total daily
energy expenditure (DEE), as measured using a SenseWear Pro
Armband accelerometer (BodyMedia, Pittsburgh, PA). Some 29 –34%
of energy came from fat, and 50 –55% from carbohydrates, according
to the recommendations of the Spanish Society of Community Nutrition [SENC, according to its Spanish initials, (29)], and 20% from
protein (beyond that outlined in the above recommendations) to
achieve the body composition benefits observed in different studies
and examined in a recent meta-analysis (38).
The hypocaloric diet program was followed during the 22-wk
intervention period. Dietary counseling was given at baseline and at
12 wk to resolve questions and to motivate participants sufficiently to
comply with dietary advice. All subjects were instructed on how to
record their dietary intake using a daily log and given recommended
portion sizes and information on possible food swaps. In addition,
nutrition education sessions were given by the dieticians. The goal
was to equip the participants with the knowledge and skills necessary
to achieve gradual but permanent behavior changes.
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
1008
•
Benito PJ et al.
Responded to the advertisement
n=751
Contacted and completed
the second questionnaire
n=432
Not interested after
preliminary information
n=319
Not eligible
n=312
Individual eligible
for orientation visit
n=120
Excluded for pathologies
Out of specified range of age
Inadequate body mass index
No sedentary behavior
Smoker
Metabolic syndrome
Binge eating disorder
Injuries and other reasons
n=49
n=12
n=118
n=58
n=12
n=34
n=18
n=11
Randomized
n=120
Assigned to S
Men (n=16)
Women (n=14)
Withdrew:
3 Lost interest
2 Job change
1 Personal reasons
Completers n=24
Assigned to E
Men (n=15)
Women (n=15)
Withdrew:
3 Lost interest
1 Diet adherence
Completers n=26
Assigned to SE
Men (n=15)
Women (n=15)
Withdrew:
1 Personal reasons
1 Job change
2 Lost interest
1 Diet adherence
1 Diet and exercise adherence
Completers n=24
Assigned to C
Men (n=15)
Women (n=15)
Withdrew:
8 Lost interest
Completers n=22
Fig. 1. Participant flow diagram.
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
Analytical Methods, Measurement of Dietetic, Physical Activity,
and Anthropometric and Body Composition Variables
The following analyses and measurements were made at baseline
and at the end of the intervention period.
Dietetic study. All food and beverages consumed by the participants were recorded using a food frequency questionnaire and a
“3-day food and drink record”, validated for the Spanish population
(23) at the beginning and end of the intervention. Participants were
instructed to record the weights of food consumed whenever possible
and to use household measurements (tablespoons, cups, etc.) when
not. The energy and nutritional content of the foods consumed were
then calculated using DIAL software (2004; Alce Ingeniería, Madrid,
Spain). The Healthy Eating Index (HEI) was calculated according to
Kennedy et al. (17), taking into account the number of servings
recommended for the Spanish population (29). Compliance with
recommended intakes was assessed for the different food groups
(cereals, vegetables/greens, fruits, dairy products, meat/fish/eggs, expressed in servings per day), and also from the point of view of
meeting nutritional objectives (intake of lipids, saturated fatty acid,
cholesterol, sodium, and dietary variety). Each of these 10 factors was
awarded a maximum of 10 points when the intake was the same as
that recommended and a minimum of 0 points when the difference
was very great. Intermediate values were awarded proportionally. Diet
quality was deemed “good” when more than 80 total points were
scored, as “needing improvement” when the score was 51– 80, and
“poor” when 50 or below (17).
Physical activity variables. Physical activity was assessed using six
items in the International Physical Activity Questionnaire-Short Form
(IPAQ-SF), which asked about the frequency and duration of vigorous
intensity activity, moderate intensity activity, and walking activity.
The questionnaire was scored using established methods posted on the
IPAQ website (www.ipaq.ki.se). The questionnaire took ⬃8 min to
complete; a trained researcher assisted participants with answering.
These data were summarized to classify the subjects into high-,
moderate-, and low-physical activity groups. Time spent in vigorous,
moderate, and walking activity was weighted by the energy expended
for these categories of activity, to produce the total metabolic equivalents per minute (MET-min) of physical activity per week. In
addition, the IPAQ-SF contained an additional indicator item of time
spent in sedentary activity: “During the last 7 days, how much time
did you usually spend sitting on a weekday?” Sitting time/week was
estimated taking into account the answers supplied.
Cardiovascular fitness was evaluated with a maximal stress test
using the modified Bruce protocol, broadly used in overweight and
obese population, on a computerized treadmill (H/P/COSMOS 3PW
4.0, H/P/Cosmos Sports & Medical, Nussdorf-Traunstein, Germany).
Peak oxygen consumption (V̇O2peak) was measured with the gas
analyzer Jaeger Oxycon Pro (Erich Jaeger; Viasys Healthcare, Höchberg, Germany). The stress test was maintained until exhaustion, and
the mean of the three highest measurements was used as V̇O2peak.
Dinamometry (maximum handgrip strength testing) was assessed
using the Tecsymp Tkk5002 hand dynamometer (Tecsymp, Barcelona, Spain) (range: 5–100 kg; precision: 0.1 kg). This test was
performed twice with the dominant hand, and the maximum score was
recorded in kilograms.
Weight and body composition variables. Height was measured
using a SECA stadiometer (range: 80 –200 cm). Body weight was
measured using a TANITA BC-420MA balance (Bio Lógica Tecnología Médica S.L, Barcelona, Spain). The BMI was calculated as
{[body weight (kg)]/[height (m)2]}. Waist circumference (WC) was
measured using a Seca 201 steel tape (Quirumed, Valencia, Spain).
Dual-energy X-ray absorptiometry (DXA) was used to measure the
total fat mass [TFM (%)], android fat [AF (%)], the android/gynoid fat
ratio (AF/GF), and the lean mass [LM (%)], employing a GE Lunar
Prodigy apparatus (GE Healthcare, Madison, WI). All DXA scans
were performed making use of GE Encore 2002 software v. 6.10.029.
•
Benito PJ et al.
1009
Adherence to Diet and Exercise
Adherence to diet was calculated as the estimated kilocalorie intake
divided by the real kilocalorie intake [(estimated kilocalories of
diet/real kilocalorie intake)·100]. Complete adherence ⫽ 100%.
Higher values reflect greater dietary restriction, while lower values
reflect lesser restriction. Those participants who failed to meet 80%
adherence to the diet were excluded from further analysis.
Adherence to exercise was calculated as the number of sessions
completed with respect to the theoretical maximum [(sessions performed/total sessions)·100]. An adherence of 90% was demanded.
Statistical Analysis
The Kolmogorov-Smirnov test was used to determine whether or
not the data were normally distributed: all variables reported in this
article met this condition. Means and SDs were calculated for continuous variables. MANOVA or two-way ANOVA for repeated measures were used to determine differences among the four interventions
groups and between baseline and post-training values. Multiple
ANOVA comparisons were made employing the Bonferroni post hoc
test. The Chi-square test was used to examine the relationship between
quantitative variables.
The sample size of the present study was calculated to detect any
effect of training and diet on TFM% (with 80% statistical power, and
with significance set at P ⬍ 0.05, assuming a correlation of 0.80
between repeated measures and assuming an estimated drop out of
20%). All analyses were performed using SPSS v. 17.0 software
(SPSS, Chicago, IL). Significance was set at ␣ ⫽ 0.05.
RESULTS
Baseline Characteristics
The baseline characteristics of the present subjects were
reported in a previous article (39). The results provided here
are for the 96 participants (48 women and 48 men; mean age:
39.27 ⫾ 7.80 yr), who completed the study (S: n ⫽ 24; E: n ⫽
26; SE: n ⫽ 24; C: n ⫽ 22). No significant differences in
baseline characteristics were seen between groups.
Diet
Adherence to diet was adequate (S: 103 ⫾ 31%; E: 103 ⫾
34%; SE: 100 ⫾ 26%; C: 98 ⫾ 21%), and acceptable compliance was achieved over the 22-wk diet intervention period
(Table 1). All groups significantly reduced their energy intake
compared with baseline (P ⬍ 0.001), with no significant
differences between groups. According to their energy profiles,
all subjects approached the recommendations of the dietary
intervention, increasing significantly the percentage of energy
provided by carbohydrate (P ⬍ 0.01) and protein (P ⬍ 0.05),
and decreasing significantly the percentage of energy provided
by fat (P ⬍ 0.01). The cholesterol intake decreased significantly by the end of the intervention period in all groups (P ⬍
0.01). At baseline, all subjects had a diet “needing improvement”, but by the end all had significantly improved their HEI
index and their dietary quality was “good”(S: 60.7 ⫾ 14.6 to
78.0 ⫾ 10.5, P ⬍ 0.001; E: 55.1 ⫾ 13.2 to 82.6 ⫾ 8.9, P ⬍
0.01; SE: 58.1 ⫾ 12.6 to 76.3 ⫾ 16.1, P ⬍ 0.001; and C:
58.5 ⫾ 10.1 to 73.5 ⫾ 19.2, P ⬍ 0.001).
Physical Activity
Table 2 shows the subjects’ physical activity variables.
Adherence to the training programs was adequate (S: 90.0 ⫾
7.0%; E: 90.0 ⫾ 8.0%; SE: 90.0 ⫾ 5.0%). The time spent
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
1010
•
Benito PJ et al.
Table 1. Dietetic variables at baseline and after 22 wk of intervention
Group/Characteristics
S n ⫽ 24
Energy intake, kcal/day
Baseline
Final
Change
2 918 ⫾ 909
1 971 ⫾ 634***
⫺946 ⫾ 183
Proteins, %EI
Baseline
Final
Change
Carbohydrates, %EI
Baseline
Final
Change
Lipids, %EI
Baseline
Final
Change
Alcohol, %EI
Baseline
Final
Change
Fiber, g/day
Baseline
Final
Change
Cholesterol, mg/day
Baseline
Final
Change
HEI
Baseline
Final
Change
E n ⫽ 26
3 007 ⫾ 1.257
1 787 ⫾ 696***
⫺1 221 ⫾ 180
Energy Profile
SE n ⫽ 24
C n ⫽ 22
P
2 555 ⫾ 873
1 734 ⫾ 471***
⫺820 ⫾ 191
2 691 ⫾ 740
1 752 ⫾ 340***
⫺939 ⫾ 206
NS
17.78 ⫾ 2.84
20.29 ⫾ 3.03**
2.52 ⫾ 0.71
16.29 ⫾ 2.79
19.87 ⫾ 2.02***
3.58 ⫾ 0.69
17.87 ⫾ 3.14
20.12 ⫾ 2.53**
2.25 ⫾ 0.74
16.37 ⫾ 2.49
20.34 ⫾ 2.90***
3.96 ⫾ 0.79
NS
38.38 ⫾ 6.05
40.58 ⫾ 4.97*
2.20 ⫾ 1.50
37.27 ⫾ 6.40
43.14 ⫾ 4.39***
5.87 ⫾ 1.47
36.52 ⫾ 4.96
43.10 ⫾ 6.73***
6.58 ⫾ 1.57
37.67 ⫾ 7.87
40.85 ⫾ 7.35*
3.18 ⫾ 1.69
NS
39.45 ⫾ 6.44
35.41 ⫾ 5.20**
⫺4.05 ⫾ 1.53
42.20 ⫾ 6.44
33.62 ⫾ 5.04***
⫺8.59 ⫾ 1.50
42.14 ⫾ 5.66
33.72 ⫾ 6.02***
⫺8.42 ⫾ 1.60
42.00 ⫾ 6.32
35.62 ⫾ 6.83***
⫺6.38 ⫾ 1.72
NS
2.56 ⫾ 3.07
1.31 ⫾ 2.57*
⫺1.25 ⫾ 0.77
2.65 ⫾ 5.18
0.66 ⫾ 1.24**
⫺1.99 ⫾ 0.75
1.72 ⫾ 1.91
0.60 ⫾ 1.37*
⫺1.12 ⫾ 0.80
2.32 ⫾ 3.57
0.65 ⫾ 1.67*
⫺1.67 ⫾ 0.86
NS
25.01 ⫾ 10.95
23.57 ⫾ 8.15
⫺1.44 ⫾ 1.80
23.79 ⫾ 8.01
23.22 ⫾ 7.43
⫺0.58 ⫾ 1.77
21.20 ⫾ 6.25
19.87 ⫾ 4.92
⫺1.32 ⫾ 1.88
21.93 ⫾ 6.05
22.12 ⫾ 6.94
0.20 ⫾ 2.03
NS
369.5 ⫾ 118.2
291.1 ⫾ 109.8**
⫺78.3 ⫾ 31.1
60.7 ⫾ 14.6
78.0 ⫾ 10.5***
17.3 ⫾ 3.5
444.6 ⫾ 201.0
262.8 ⫾ 97.8***
⫺181.8 ⫾ 30.5
449.7 ⫾ 192.3
278.7 ⫾ 104.0***
⫺171.0 ⫾ 32.5
55.1 ⫾ 13.2
82.6 ⫾ 8.9***
27.5 ⫾ 3.5
415.3 ⫾ 134.4
273.9 ⫾ 102.8***
⫺141.3 ⫾ 35.0
58.1 ⫾ 12.6
76.3 ⫾ 16.1***
18.2 ⫾ 3.6
58.5 ⫾ 10.1
73.5 ⫾ 19.2***
15.0 ⫾ 3.8
NS
NS
Values are expressed as means ⫾ SD. S, strength group; E, endurance group; SE, combined strength ⫹ endurance group; C, control group; EI, energy intake;
HEI, healthy eating index. *P ⬍ 0.05, significantly different compared to baseline. **P ⬍ 0.01, significantly different compared to baseline. ***P ⬍ 0.001),
significantly different compared to baseline. P denotes significant difference for the comparison of mean change after the intervention between treatments, with
baseline values as covariates. NS, not significant.
sitting per week decreased significantly after the intervention in
all groups (S: ⫺142.0 ⫾ 32.9; E: ⫺100.0 ⫾ 34.0; SE: ⫺98.8 ⫾
31.9; C: ⫺100.0 ⫾ 38.4 min/wk; no significant differences
between groups). In addition, all groups increased significantly
their total physical activity per week during the intervention (S:
1,314 ⫾ 708 to 2,290 ⫾ 982 MET-min/wk, P ⬍ 0.01; E:
1,428 ⫾ 727 to 2,884 ⫾ 1,707 MET-min/wk, P ⬍ 0.001; SE:
1,637 ⫾ 862 to 2,966 ⫾ 1,556 MET-min/wk, P ⬍ 0.001;
C: 1,366 ⫾ 861 to 2,128 ⫾ 1,083 MET-min/wk, P ⬍ 0.05),
with no differences between groups.
The change in the percentage of “high physical activity”
subjects increased in all groups after the intervention, more so
in the exercise training groups (S: 73.3%; E: 56.3%: SE:
70.6%; C: 25.0%).
Peak oxygen consumption improved only in SE (3,103 ⫾
692 to 3,405 ⫾ 907, P ⫽ 0.001). Strength measured by
dynamometry showed no differences in any groups.
Weight and Body Composition
A significant reduction in body weight, BMI, WC, TFM,
AF, and AF/GF, and a significant increase in LM, was detected
in all groups after the intervention, with no significant differences between groups (Table 3).
DISCUSSION
To our knowledge, this is the first clinical trial designed to
examine the effect of different physical activity interventions,
in combination with a hypocaloric diet, on body weight and
composition variables in obese Spanish people. Maintaining a
hypocaloric diet and regular physical activity, independent of
the type followed, improved the anthropometric and body
composition variables by the end of the 22-wk intervention
period.
Our knowledge of the efficacy of physical activity as part of
obesity prevention is based on a very small number of studies
(19, 21). Some of these report a positive impact on BMI and
body weight, but the heterogeneity in terms of study design,
theoretical underpinning, and target population, make it difficult to draw any firm conclusions regarding which interventions are most effective. The PRONAF study, of which the
present work is part, was designed as a clinical trial to clarify
the importance of physical activity in the treatment of obesity.
The information currently available suggests that the best
type of diet for treating obesity is one low in fat and sugary
beverages, and high in carbohydrates, fiber, grains, fruits and
vegetables, and proteins (3). According to the recommendations of the SENC (29), a balanced diet should provide 30 –
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
•
1011
Benito PJ et al.
Table 2. Physical activity variables (mean ⫾ SD) at baseline before and after 22 wk of intervention
S n ⫽ 24
E n ⫽ 26
SE n ⫽ 24
C n ⫽ 22
P
486.0 ⫾ 204.2
344.0 ⫾ 176.3***
⫺142.0 ⫾ 32.9
434.3 ⫾ 168.9
334.3 ⫾ 240.5**
⫺100.0 ⫾ 34.0
543.8 ⫾ 182.6
445.0 ⫾ 162.8**
⫺98.8 ⫾ 31.9
661.8 ⫾ 119.9
561.8 ⫾ 161.0*
⫺100.0 ⫾ 38.4
NS
1428 ⫾ 727
2884 ⫾ 1707***
1457 ⫾ 358
1637 ⫾ 862
2966 ⫾ 1556***
1329 ⫾ 345
1366 ⫾ 861
2128 ⫾ 1083*
763 ⫾ 410
NS
Group/Characteristics
Sitting time, min/wk
Baseline
Final
Change
Total PhA, MET min/wk
Baseline
Final
Change
1314 ⫾ 708
2290 ⫾ 982**
976 ⫾ 367
Physical activity categories, % subjects
Baseline
Final
Change
V̇O2peak, l/min
Baseline
Final
Change
Dinamometry, kg
Baseline
Final
Change
LMH
LMH
LMH
LMH
20.0 73.0 6.7
6.7 13.3 80.0
⫺13.3 ⫺59.7 73.3
6.3 68.8 25.0
6.3 12.5 81.3
0.0 ⫺56.3 56.3
11.8 76.5 11.8
0.0 17.6 82.4
⫺11.8 ⫺58.9 70.6
16.7 75.0 8.3
25.0 41.7 33.3
8.3 ⫺33.3 25.0
P ⬍ 0.05
3251 ⫾ 855
3205 ⫾ 856
⫺46 ⫾ 347
2923 ⫾ 754
2927 ⫾ 696
3 ⫾ 466
3103 ⫾ 692
3405 ⫾ 907**
302 ⫾ 485
2969 ⫾ 817
3019 ⫾ 813
50 ⫾ 290
P ⬍ 0.05
40 ⫾ 14
40 ⫾ 14
0 ⫾ 10
34 ⫾ 15
38 ⫾ 12
4 ⫾ 13
39 ⫾ 11
38 ⫾ 14
2⫾5
36 ⫾ 13
31 ⫾ 19
⫺6 ⫾ 15
NS
Values are expressed as means ⫾ SD. V̇O2peak, peak oxygen consumption; L: low physical activity group; M: moderate physical activity group; H: high
physical activity group. *P ⬍ 0.05, significantly different compared to baseline. **P ⬍ 0.01, Significantly different compared to baseline. ***P ⬍ 0.001,
significantly different compared to baseline. P denotes significant difference for the comparison of mean change after the intervention between treatments, with
baseline values as covariates.
35% of energy from fat, 15–18% from protein, and 50 –55%
from carbohydrates. A recent meta-analysis showed that a
hypocaloric, high-protein, and low-fat diet provides modest
benefits in terms of body composition variables compared with
a standard-protein, low-fat diet (38). On the basis of this
evidence, a hypocaloric balanced diet was designed for use in
the present study (30% of energy from fat, 20% from protein,
and 50% from carbohydrates). All subjects reduced their en-
Table 3. Anthropometric and body composition variables before and after 22 wk of intervention by group
Group/Characteristics
Weight, kg
Baseline
Final
Change
BMI, kg/m2
Baseline
Final
Change
WC, cm
Baseline
Final
Change
TFM, %
Baseline
Final
Change
AF, %
Baseline
Final
Change
AF/GF, %
Baseline
Final
Change
LM, %
Baseline
Final
Change
S n ⫽ 24
E n ⫽ 26
SE n ⫽ 24
C n ⫽ 22
P
96.35 ⫾ 10.20
87.13 ⫾ 9.97***
⫺9.21 ⫾ 0.83
93.50 ⫾ 9.10
82.95 ⫾ 8.91***
⫺10.55 ⫾ 0.80
98.01 ⫾ 13.50
88.13 ⫾ 13.29***
⫺9.88 ⫾ 0.85
92.32 ⫾ 13.03
83.63 ⫾ 12.30***
⫺8.69 ⫾ 0.89
NS
33.28 ⫾ 1.81
30.15 ⫾ 2.26***
⫺3.13 ⫾ 0.32
33.56 ⫾ 2.54
29.57 ⫾ 2.85***
⫺3.99 ⫾ 0.30
33.91 ⫾ 2.66
30.49 ⫾ 2.78***
⫺3.42 ⫾ 0.32
33.11 ⫾ 2.74
30.04 ⫾ 2.99***
⫺3.08 ⫾ 0.34
NS
103.25 ⫾ 7.33
94.42 ⫾ 7.57***
⫺8.83 ⫾ 1.15
101.69 ⫾ 7.14
91.85 ⫾ 6.38***
⫺9.85 ⫾ 1.10
102.91 ⫾ 7.8
94.59 ⫾ 7.94***
⫺8.33 ⫾ 1.17
103.79 ⫾ 9.79
94.52 ⫾ 9.22***
⫺9.26 ⫾ 1.23
NS
41.89 ⫾ 5.56
36.65 ⫾ 6.59***
⫺5.24 ⫾ 0.55
42.89 ⫾ 5.77
37.55 ⫾ 6.47***
⫺5.35 ⫾ 0.55
44.08 ⫾ 6.38
39.23 ⫾ 7.46***
⫺4.85 ⫾ 0.56
41.38 ⫾ 5.58
36.49 ⫾ 6.76***
⫺4.89 ⫾ 0.59
NS
49.80 ⫾ 4.80
40.21 ⫾ 10.37***
⫺9.59 ⫾ 1.27
50.30 ⫾ 5.55
42.79 ⫾ 7.14***
⫺7.51 ⫾ 1.27
51.92 ⫾ 6.15
45.43 ⫾ 8.72***
⫺6.50 ⫾ 1.30
49.74 ⫾ 5.55
42.38 ⫾ 7.73***
⫺7.36 ⫾ 1.36
NS
1.19 ⫾ 0.18
1.16 ⫾ 0.20***
⫺0.03 ⫾ 0.01
1.14 ⫾ 0.19
1.11 ⫾ 0.18***
⫺0.03 ⫾ 0.01
1.18 ⫾ 0.20
1.17 ⫾ 0.22***
⫺0.01 ⫾ 0.01
1.22 ⫾ 0.21
1.17 ⫾ 0.23***
⫺0.04 ⫾ 0.02
NS
56.29 ⫾ 5.25
61.21 ⫾ 6.15***
4.92 ⫾ 2.78
55.46 ⫾ 5.67
60.34 ⫾ 6.09***
4.99 ⫾ 1.85
54.12 ⫾ 5.92
58.76 ⫾ 7.02***
4.54 ⫾ 2.55
56.53 ⫾ 5.27
61.25 ⫾ 6.34***
4.52 ⫾ 2.77
NS
Values are expressed as mean values ⫾ SD. BMI, body mass index; WC, waist circumference; TFM, total fat mass; AF, android fat; AF/GF, android/gynoid
fat ratio; LM, lean mass. ***P ⬍ 0.001, significantly different compared to baseline. P denotes significant difference for the comparison of mean change after
the intervention between treatments, with baseline values as covariates.
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
1012
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
ergy intake and showed good compliance with the protein and
fat intake recommendations. However, the percentage of energy supplied by carbohydrate did not increase enough to attain
the goal set out. Similar findings have been reported in other
interventional studies in which the dietary recommendations
were based on the same criteria (2, 22). However, different
studies suggest that diets supplying 40 –50% of total energy
from carbohydrate may be effective alternatives to those insisting on ⬎50% of energy coming from this macronutrient,
since similar weight losses were achieved (14, 28, 38).
It is important to note that all subjects in the present study
enjoyed considerably improved dietary quality after the intervention; all groups had a diet “needing improvement” at
baseline and at the end all had a “good” HEI index. The
dieticians made sure they informed the subjects on the most
important aspects of diet quality during the nutrition education
sessions. It might be essential to equip participants with the
knowledge and skills necessary to achieve gradual but permanent behavior changes.
In addition to increased obesity, a sedentary lifestyle during
adulthood may also be associated with increased mortality.
Physical activity is important for overall good health (8, 35). In
the present study, all of the physical activity programs (C
group recommendations included) contributed toward increasing the total physical activity and reducing inactivity in all
subjects. All of the groups reduced their sitting time, and the
percentage of people classified as showing “high physical
activity” increased. This was especially true for the exercisetraining groups, with no significant differences observed between them. However, improvement in V̇O2peak was observed
only in the combined training group. Motivational factor could
be responsible for this difference, since combined training is
less monotonous than continuous aerobic training that can be
more effective in obese people (6).
The scientific evidence suggests that the combination of
dietary modification and exercise is the most effective behavioral approach for achieving weight loss (5, 7, 32); hence, the
reason why the present study was designed combining both for
all groups. Different authors have also indicated the urgent
need to design large, effective, evidence-based programs based
on exercise interventions to clarify the role of physical activity
in obesity prevention (19, 21).
After the present interventions, all subjects saw improvements in their anthropometric and body composition variables,
with no significant differences detected between any of the
groups. Other authors have concluded that dietary restriction
combined with endurance exercise training is effective in
achieving weight loss and reducing fat mass in obese subjects
(15, 25, 31). However, few studies have compared the effects
of similar amounts of aerobic and resistance training on body
mass and fat mass in obese people. In the recent STRRIDE
AT/RT (Studies of a Targeted Risk Reduction Through Defined Exercise) study, (37) aerobic training (AT), resistance
training (RT), and a combination of the two, were compared to
determine the optimum mode of exercise for obesity reduction
over an 8-mo intervention period. The authors concluded that
a program of combined AT/RT did not result in significantly
greater fat mass or body mass reduction over AT alone. In fact,
balancing time commitments against health benefits, AT would
appear to be the optimal mode. A program, including RT, is
best if increased muscle mass and strength are sought. It should
•
Benito PJ et al.
be remembered, however, that the STRRIDE AT/RT study did
not include a dietary intervention, and the weight lost over the
8 mo was much less than in the present study (RT: 0.83 ⫾ 2.32
vs. S: ⫺9.21 ⫾ 0.83; AT: ⫺1.76 ⫾ 3.00 vs. E: ⫺10.55 ⫾ 0.80;
AT/RT: ⫺1.63 ⫾ 3.17 vs. SE: ⫺9.88 ⫾ 0.85 kg). Certainly,
other authors have indicated that exercise programs alone are
less efficient than those combined with diet control for achieving good weight management (13, 30). In addition, the
STRRIDE AT/RT study did not include a control group; the
impact of following physical activity recommendations was,
therefore, not determined.
The present study shows that, when adhered to alongside a
hypocaloric diet, different exercise training programs (endurance, strength, or their combination) or the following of physical activity recommendations are equally efficient in terms of
improving body weight and body composition variables in
obesity management. The lack of efficiency of the training
programs may be attributable to a compensatory reduction in
daily physical activity (13). Alternatively, it may be due to a
lack of continuity in their undertaking: while the C group
practiced regular physical activity daily, the S, E, and SE
groups practiced exercise on only 3 days/wk. These results
back up the exercise recommendations in the European Clinical Practice Guidelines for the Management of Obesity in
Adults (32). These explain that the objective should be to
reduce sedentary behavior and increase daily activities (e.g.,
walking or cycling instead of using a car, climbing stairs
instead of using the elevator, etc.).
Subjects should be advised and helped in undertaking (or
increasing) physical activity. Exercise advice must be tailored
to a person’s ability and health, and focus on a gradual increase
with levels that are safe. Current recommendations suggest that
people of all ages should undertake 30 – 60 min of physical
activity of moderate intensity (such as brisk walking) on most,
if not all, days of the week (16, 26, 27). In fact, it is important
to look for exercise interventions that can easily be integrated
into daily life and that are not associated with an increased risk
of trauma. Most importantly, patients should enjoy the proposed kind of physical exercise (20).
Many authors have concluded that the inclusion of an
exercise training program in the treatment of obesity is important for maintaining long-term weight control (13, 30). The
ongoing PRONAF study, therefore, plans to evaluate the effect
of the present programs at 6 mo and 3 yr after the intervention.
The data collected will be presented in a future article.
In conclusion, the present study shows that, when combined
with a hypocaloric diet, the adherence to physical activity
recommendations is just as effective as exercise training programs in the improvement of body weight and body composition in obese subjects.
GRANTS
The PRONAF Study is funded by the Ministerio de Ciencia e Innovación,
Convocatoria de Ayudas I⫹D 2008, Proyectos de Investigación Fundamental
No Orientada del VI Plan de Investigación Nacional 2008 –2011 (Grant code
DEP2008-06354-C04-01).
AUTHOR CONTRIBUTIONS
Author contributions: P.J.B., L.M.B., A.B.P., F.J.C., and C.G.-C. conception and design of research; P.J.B., L.M.B., A.B.P., B.L.-P., R.C., B.S., and
E.A.C. performed experiments; P.J.B., L.M.B., A.B.P., B.L.-P., R.C., B.S., and
E.A.C. analyzed data; P.J.B., L.M.B., A.B.P., B.L.-P., R.C., B.S., and E.A.C.
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.
Obesity: Diet ⫹ Exercise or ⫹ Recommendations?
interpreted results of experiments; P.J.B. and L.M.B. prepared figures; P.J.B.
and L.M.B. drafted manuscript; P.J.B., L.M.B., A.B.P., B.L.-P., R.C., B.S.,
F.J.C., E.A.C., and C.G.-C. edited and revised manuscript; P.J.B., L.M.B.,
A.B.P., B.L.-P., R.C., B.S., F.J.C., E.A.C., and C.G.-C. approved final version
of manuscript.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
REFERENCES
1. Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, BallardBarbash R, Hollenbeck A, Leitzmann MF. Overweight, obesity, and
mortality in a large prospective cohort of persons 50 to 71 years old. N
Engl J Med 355: 763–778, 2006.
2. Arrebola E, Gomez-Candela C, Fernandez-Fernandez C, Loria V,
Munoz-Perez E, Bermejo LM. Evaluation of a lifestyle modification
program for treatment of overweight and nonmorbid obesity in primary
healthcare and its influence on health-related quality of life. Nutr Clin
Pract 26: 316 –321, 2011.
3. Astrup A. The role of dietary fat in obesity. Semin Vasc Med 5: 40 –47,
2005.
4. Berghofer A, Pischon T, Reinhold T, Apovian CM, Sharma AM,
Willich SN. Obesity prevalence from a European perspective: a systematic review. BMC Public Health 8: 200, 2008.
5. Catenacci VA, Wyatt HR. The role of physical activity in producing and
maintaining weight loss. Nat Clin Pract Endocrinol Metab 3: 518 –529,
2007.
6. Coquart JB, Lemaire C, Dubart AE, Luttembacher DP, Douillard C,
Garcin M. Intermittent versus continuous exercise: effects of perceptually
lower exercise in obese women. Med Sci Sports Exerc 40: 1546 –1553,
2008.
7. Del Corral P, Chandler-Laney PC, Casazza K, Gower BA, Hunter
GR. Effect of dietary adherence with or without exercise on weight loss:
a mechanistic approach to a global problem. J Clin Endocrinol Metab 94:
1602–1607, 2009.
8. Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith
BK. American College of Sports Medicine Position Stand. Appropriate
physical activity intervention strategies for weight loss and prevention of
weight regain for adults. Med Sci Sports Exerc 41: 459 –471, 2009.
9. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis
AH. The incidence of co-morbidities related to obesity and overweight: a
systematic review and meta-analysis. BMC Public Health 9: 88, 2009.
10. Guilbert JJ. The world health report 2002—reducing risks, promoting
healthy life. Educ Health (Abingdon) 16: 230, 2003.
11. Gutierrez-Fisac JL, Guallar-Castillon P, Leon-Munoz LM, Graciani
A, Banegas JR, Rodriguez-Artalejo F. Prevalence of general and abdominal obesity in the adult population of Spain, 2008 –2010: the ENRICA study. Obes Rev 13: 388 –392, 2011.
12. Hainer V, Toplak H, Mitrakou A. Treatment modalities of obesity: what
fits whom? Diabetes Care 31: S269 –S277, 2008.
13. Hansen D, Dendale P, Berger J, van Loon LJ, Meeusen R. The effects
of exercise training on fat-mass loss in obese patients during energy intake
restriction. Sports Med 37: 31–46, 2007.
14. Hu T, Mills KT, Yao L, Demanelis K, Eloustaz M, Yancy WS Jr, Kelly
TN, He J, and Bazzano LA. Effects of low-carbohydrate diets versus
low-fat diets on metabolic risk factors: a meta-analysis of randomized
controlled clinical trials. Am J Epidemiol 176 Suppl 7: S44 –S54, 2012.
15. Hunter GR, Byrne NM, Sirikul B, Fernandez JR, Zuckerman PA,
Darnell BE, Gower BA. Resistance training conserves fat-free mass and
resting energy expenditure following weight loss. Obesity (Silver Spring)
16: 1045–1051, 2008.
16. Jakicic JM. Exercise in the treatment of obesity. Endocrinol Metab Clin
North Am 32: 967–980, 2003.
17. Kennedy ET, Ohls J, Carlson S, Fleming K. The healthy eating index:
design and applications. J Am Diet Assoc 95: 1103–1108, 1995.
18. Kirk SF, Penney TL, McHugh TL, Sharma AM. Effective weight
management practice: a review of the lifestyle intervention evidence. Int J
Obes (Lond) 36: 178 –185, 2011.
19. Lemmens VE, Oenema A, Klepp KI, Henriksen HB, Brug J. A
systematic review of the evidence regarding efficacy of obesity prevention
interventions among adults. Obes Rev 9: 446 –455, 2008.
20. Linke A, Mobius-Winkler S, Hambrecht R. Exercise training in the
treatment of coronary artery disease and obesity. Herz 31: 224 –233, 2006.
•
Benito PJ et al.
1013
21. Lombard CB, Deeks AA, Teede HJ. A systematic review of interventions aimed at the prevention of weight gain in adults. Public Health Nutr
12: 2236 –2246, 2009.
22. Loria-Kohen V, Gomez-Candela C, Fernandez-Fernandez C, PerezTorres A, Garcia-Puig J, Bermejo LM. Evaluation of the usefulness of
a low-calorie diet with or without bread in the treatment of overweight/
obesity. Clin Nutr 31: 455–461, 2012.
23. Moreno LA, Kersting M, de Henauw S, Gonzalez-Gross M, SichertHellert W, Matthys C, Mesana MI, Ross N. How to measure dietary
intake and food habits in adolescence: the European perspective. Int J
Obes (Lond) 29 Suppl 2: S66 –S77, 2005.
24. Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A,
Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 138: 24 –32, 2003.
25. Poehlman ET, Dvorak RV, DeNino WF, Brochu M, Ades PA. Effects
of resistance training and endurance training on insulin sensitivity in
nonobese, young women: a controlled randomized trial. J Clin Endocrinol
Metab 85: 2463–2468, 2000.
26. Poirier P, Despres JP. Exercise in weight management of obesity.
Cardiol Clin 19: 459 –470, 2001.
27. Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L,
Fogelholm M, Rissanen A, Schoeller D, Swinburn B, Tremblay A,
Westerterp KR, Wyatt H. How much physical activity is enough to
prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev 4: 101–114, 2003.
28. Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg
I, Golan R, Fraser D, Bolotin A, Vardi H, Tangi-Rozental O, ZukRamot R, Sarusi B, Brickner D, Schwartz Z, Sheiner E, Marko R,
Katorza E, Thiery J, Fiedler GM, Bluher M, Stumvoll M, Stampfer
MJ. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet.
N Engl J Med 359: 229 –241, 2008.
29. Spanish Society of Community Nutrition (SENC). Healthy nutrition
Guide. http://aesan.msssi.gob.es/AESAN/docs/docs/publicaciones_estudios/
nutricion/guia_alimentacion.pdf. Madrid: SENC, 2004.
30. Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role
of exercise and physical activity in weight loss and maintenance. Prog
Cardiovasc Dis 56: 441–447, 2014.
31. Thomson RL, Buckley JD, Noakes M, Clifton PM, Norman RJ,
Brinkworth GD. The effect of a hypocaloric diet with and without
exercise training on body composition, cardiometabolic risk profile, and
reproductive function in overweight and obese women with polycystic
ovary syndrome. J Clin Endocrinol Metab 93: 3373–3380, 2008.
32. Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen
E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, ZahorskaMarkiewicz B. Management of obesity in adults: European clinical
practice guidelines. Obes Facts 1: 106 –116, 2008.
33. Usui C, Asaka M, Kawano H, Aoyama T, Ishijima T, Sakamoto S,
Higuchi M. Visceral fat is a strong predictor of insulin resistance regardless of cardiorespiratory fitness in non-diabetic people. J Nutr Sci Vitaminol (Tokyo) 56: 109 –116, 2010.
34. Van Camp CM, Hayes LB. Assessing and increasing physical activity. J
Appl Behav Anal 45: 871–875, 2013.
35. Waxman A. WHO global strategy on diet, physical activity and health.
Food Nutr Bull 25: 292–302, 2004.
36. Willett WC, Manson JE, Stampfer MJ, Colditz GA, Rosner B, Speizer
FE, Hennekens CH. Weight, weight change, and coronary heart disease
in women. Risk within the ‘normal’ weight range. JAMA 273: 461–465,
1995.
37. Willis LH, Slentz CA, Bateman LA, Shields AT, Piner LW, Bales CW,
Houmard JA, Kraus WE. Effects of aerobic and/or resistance training on
body mass and fat mass in overweight or obese adults. J Appl Physiol
(1985) 113: 1831–1837, 2012.
38. Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD.
Effects of energy-restricted high-protein, low-fat compared with standardprotein, low-fat diets: a meta-analysis of randomized controlled trials. Am
J Clin Nutr 96: 1281–1298, 2012.
39. Zapico AG, Benito PJ, Gonzalez-Gross M, Peinado AB, Morencos E,
Romero B, Rojo-Tirado MA, Cupeiro R, Szendrei B, Butragueno J,
Bermejo M, Alvarez-Sanchez M, Garcia-Fuentes M, Gomez-Candela
C, Bermejo LM, Fernandez-Fernandez C, Calderon FJ. Nutrition and
physical activity programs for obesity treatment (PRONAF study): methodological approach of the project. BMC Public Health 12: 1100, 2012.
J Appl Physiol • doi:10.1152/japplphysiol.00928.2014 • www.jappl.org
Downloaded from journals.physiology.org/journal/jappl (188.154.208.116) on April 25, 2022.