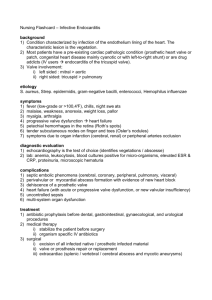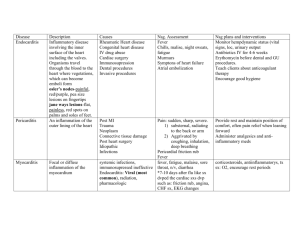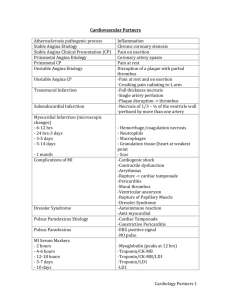
1 Endocarditis Ian James Nova Southeastern University NSG 5630: Adult-Acute Care II Dr. Nekisha Hyman October 14, 2021 2 Endocarditis Endocarditis as defined by Chu (2018) is an infection of the inner layer of the heart (endocardium) with the heart valves being the main areas being affected as seen in the patient case study presented in the Emory Cardiology (2018) Grand Rounds: Infectious Endocarditis video presentation. Endocarditis is usually caused when microorganisms usually bacteria enter the bloodstream through the gums or intestines; by healthcare-related procedures such as intravenous catheter placement, surgery, or hemodialysis; or through the skin because of intravenous drug abuse and attach themselves to the endocardium usually the heart valve. According to Long and Koyfman (2018), major risk factors include previous history of endocarditis, certain congenital heart defects, immune-suppressed patients, an artificial (prosthetic) heart valve, implanted heart devices, poor dental health, acquired valve disease such as valve prolapse or regurgitation (leaking). As seen in the patient case study by Emory Cardiology (2018), the patient had an increased risk of developing endocarditis due to having a medical history of valve regurgitation (leaky valve) and having dental surgery (tooth implants) done 8 months ago. In endocarditis, clumps made of bacteria and cell pieces form an abnormal mass in the heart. These clumps, called vegetations, can break loose and travel to the brain, lungs, abdominal organs, kidneys, or arms and legs. As a result, endocarditis can cause several complications, including stroke, pulmonary embolism, renal failure, and splenomegaly (Holland et al., 2016) The treatment of endocarditis includes antibiotics and sometimes surgery. Antibiotics are targeted based on the bacteria causing the infection. Patients usually receive a long course of antibiotics, usually 4 to 6 weeks. Generally, 4 weeks for native valve endocarditis and 6 weeks for prosthetic valve endocarditis. Some of the most common microbial causes of endocarditis 3 include Staphylococcus aureus, Viridans group streptococci and Streptococcus bovis group, and Enterococcus faecalis. For Staphylococcus aureus, the antibiotic of choice is flucloxacillin and vancomycin. For the Viridans group streptococci and Streptococcus bovis group, benzylpenicillin 1.2 g or ceftriaxone 2 g is recommended. For Enterococcus faecalis, amoxicillin 2 g and gentamicin 1 mg/kg, or ceftriaxone 2 g is recommended (Rajani & Klein, 2020). Some patients may also require surgical repair or replacement of the infected heart valve. According to Emory Cardiology (2018), the purpose of surgery in endocarditis is to remove the infection, restore cardiac integrity and valve function, and remove threatening sources of embolism. According to Emory Cardiology (2018) and Nishimura et al. (2017) patients with endocarditis who are highly appropriate for surgery include those who present with valve dysfunction with symptoms of heart failure. Other patients highly appropriate for surgery include those whose endocarditis is caused by Staphylococcus aureus, fungal, or other highly resistant organisms. Patients whose endocarditis is complicated by heart block, aortic abscess, destructive penetrating lesions, and patients with persistent bacteremia or fevers lasting longer than 5-7 days after starting appropriate antimicrobial therapy are also appropriate for surgical intervention. When it comes to stroke patients with endocarditis the timing of surgery remains controversial with both Emory Cardiology (2018) and Nishimura et al. (2017) recommending early surgery for minor stroke (no evidence of intracranial bleed or extensive neurological damage) and delayed surgery for major stroke. For prosthetic valve endocarditis and relapsing infection both Emory Cardiology (2018) and Nishimura et al. (2017) recommend surgery. For patients with endocarditis with infected implanted heart devices or devices not infected but with highly resistant organisms surgery is recommended to remove the device. 4 References Chu, V. H. (2018). Endocarditis. JAMA, 320(1), 102. Emory Cardiology. (2018, February 04). Cardiovascular fellows rounds 2-02-18. YouTube. https://youtu.be/fSfMnBEafj8 Holland, T. L., Baddour, L. M., Bayer, A. S., Hoen, B., Miro, J. M., & Fowler, V. G., Jr (2016). Infective endocarditis. Nature Reviews Disease Primers, 2, 16059. Long, B., & Koyfman, A. (2018). Infectious endocarditis: An update for emergency clinicians. The American Journal of Emergency Medicine, 36(9), 1686–1692. Nishimura, R. A., Otto, C. M., Bonow, R. O., Carabello, B. A., Erwin, J. P., III, Fleisher, L. A., Jneid, H., Mack, M. J., McLeod, C. J., O’Gara, P. T., Rigolin, V. H., Sundt, T. M., III, Thompson, A., Levine, G. N., Halperin, J. L., Gentile, F., Gidding, S., Hlatky, M. A., Ikonomidis, J., … ACC AHA Task Force Members. (2017). 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease. Journal of the American College of Cardiology, 70(2), 252–289. Rajani, R., & Klein, J. L. (2020). Infective endocarditis: A contemporary update. Clinical Medicine, 20(1), 31–35.