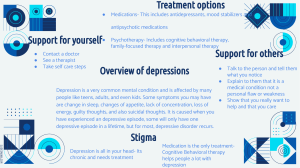
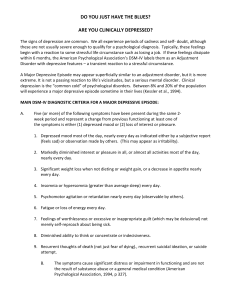
MOOD DISORDERS Mood • the sustained and pervasive emotion subjectively experienced and reported by the patient, and is observable to others. • examples include depression, elation, anger. Mood Disorders • Involve disabling disturbances in emotion – from the extreme sadness and disengagement of depression to the extreme elation and irritability of mania Two broad types • Involves only depressive symptoms • Involves manic symptoms (bipolar disorder) Depressive Disorders • Cardinal symptoms: Profound sadness and/or an inability to experience pleasure • Self-recriminations • Focused on their flaws and deficits • Very negative light, tend to lose hope Depressive Disorders • Physical symptoms: – Fatigue – Low energy – Physical aches and pains • Hard to fall asleep and may wake up frequently • Others sleep throughout the day • Appetite is gone or experience an increase in appetite Depressive Disorders • Psychomotor retardation (thoughts and movements may slow for some) • Psychomotor agitation (they pace, fidget, and wring their hands) • Social withdrawal is common! • Many prefer to sit alone and be silent Major Depressive Disorder (MDD) • Five depressive symptoms to be present for at least 2 weeks • Symptoms must include either depressed mood or loss of interest and pleasure Major Depressive Episode • • • • • • • • • Depressed mood Inability to experience pleasure (anhedonia) Fatigue or loss of energy (anergia) Recurrent thought of death or suicidal ideation Feelings of worthlessness Sleep disturbance Appetite disturbance Diminished ability to concentrate Psychomotor disturbance Major Depressive Disorder (MDD) • An episodic disorder – symptoms tend to be present for a period of time and then clear • Tend to recur- once a given episode clears, a person to likely to experience another episode • 2/3rds will experience at least 1 more episode during their lifetime Subclinical Depression • Sadness plus 3 other symptoms for 10 days • Significant impairments in functioning even though full diagnostic criteria are not met Specifiers of Major Depressive Disorder • Specify the features of the latest depressive episode. • these symptoms, or specifiers, may or may not accompany a depressive disorder; • When they do, they are often helpful in determining the most effective treatment or likely course. • In addition to rating severity of the episode as mild, moderate, or severe, Specifiers of Major Depressive Disorder • Psychotic features • Individual in the midst of a major depressive (or manic) episode may experience psychotic symptoms, specifically hallucinations and delusions • Mood congruent – consistent with the depressed mood • Mood incongruent – do not seem consistent with the depressed mood Specifiers of Major Depressive Disorder • Anxious distress specifier - the presence and severity of accompanying anxiety • indicates a more severe condition, makes suicidal thoughts and completed suicide more likely, and predicts a poorer outcome from treatment. Specifiers of Major Depressive Disorder • Mixed features specifier - predominantly depressive episodes that have several (at least 3) symptoms of mania Specifiers of Major Depressive Disorder • Melancholic features specifier - the specifier applies only if the full criteria for a MDE have been met - some of the more severe somatic (physical) symptoms, such as early-morning awakenings, weight loss, loss of libido (sex drive), excessive or inappropriate guilt, and anhedonia (diminished interest or pleasure in activities). Specifiers of Major Depressive Disorder • Catatonic Features Specifiers - This serious condition involves an absence of movement (a stuporous state) or catalepsy, in which the muscles are waxy and semirigid, so a patient’s arms or legs remain in any position in which they are placed Specifiers of Major Depressive Disorder • Atypical Features Specifier - individuals with this specifier consistently oversleep and overeat during their depression and therefore gain weight Specifiers of Major Depressive Disorder • Peripartum onset specifier - Peri means “surrounding”, in this case the period of time just before and just after the birth. This specifier can apply to both major depressive and manic episodes • Seasonal pattern specifier - it accompanies episodes that occur during certain seasons (for example, winter depression) - In bipolar disorder, individuals may become depressed during the winter and manic during the summer. - At least two years with no evidence of nonseasonal major depressive episodes occurring during that period of time. This condition is called seasonal affective disorder (SAD). Chronic Depressive Disorder • Dysthymia • Persistent Depressive Disorder • Chronically depressed – more than half of the time for at least 2 years ( or 1 year for children and adolescents) Chronic Depressive Disorder • Characterized by either chronic major depressive disorder or a chronic but milder form of depression • Typically begins in childhood or adolescence and tends to follow a chronic course through adulthood Double Depression • Applies to those who have a major depressive episode superimposed on a longer-standing dysthymia • Have more severe depressive episodes than people with major depression alone Other Depressive Disorders • Premenstrual dysphoric disorder (PMDD) • Disruptive mood dysregulation disorder *Added in the DSM - 5 Premenstrual Dysphoric Disorder • Intended to apply to women who experience a range of significant psychological symptoms in the week before menses (and improvement beginning within a few days following the onset of menses) • A range of symptoms need to be present to diagnose PMDD, including symptoms such as • mood swings • sudden tearfulness or feeling of sadness • depressed mood or feelings of hopelessness, • irritability or anger • feelings of anxiety • tension, • being on edge • greater sensitivity to cues of rejection • and negative thoughts about oneself. Disruptive Mood Dysregulation Disorder • Severe recurrent temper outbursts and persistent negative mood for at least 1 year beginning before age 10 Gender Difference in Depression • MDD twice as common in women than men - Similar discrepancy occurs in many countries • Differences emerge in adolescence • Some biological and psychological factors may include • Some biological and psychological factors may include - Hormone - Girls twice as likely to experience sexual abuse - women more likely to experience chronic stressors - girls and women more likely to worry about body image - women may react more intensely to interpersonal loss - women spend more time ruminating; men tend to distract • Before Billy reached the ward, you could hear him laughing and carrying on in a deep voice; it sounded as if he was having a wonderful time. As the nurse brought Billy down the hall to introduce him to the staff, he spied the Ping-Pong table. Loudly, he exclaimed, “PingPong! I love Ping-Pong! I have only played twice but that is what I am going to do while I am here; I am going to become the world’s greatest Ping-Pong player! And that table is gorgeous! • I am going to start work on that table immediately and make it the finest Ping-Pong table in the world. I am going to sand it down, take it apart, and rebuild it until it gleams and every angle is perfect!” Billy soon went on to something else that absorbed his attention • The previous week, Billy had emptied his bank account, taken his credit cards and those of his elderly parents with whom he was living, and bought every piece of fancy stereo equipment he could find. He thought that he would set up the best sound studio in the city and make millions of dollars by renting it to people who would come from far and wide. This episode had precipitated his admission to the hospital. Bipolar Disorders • Three forms Bipolar I Disorder, Bipolar II Disorder, Cyclothymic Disorder • Manic symptoms are the defining feature of each of these disorders • Differentiated by how sever and long-lasting the manic symptoms are. • Most people who experience mania will also experience depression during their lifetime. Manic and Hypomanic Episodes • Typically begins abruptly • The hallmark feature of a manic episode is increased activity or energy • Person experiences a sudden elevation or expansion of mood and feels unusually cheerful, or optimistic • Symptoms cause significant distress or functional impairment Manic or Hypomanic • Deny they have a problem • Spends large amount of money, making foolish business decisions Hypomania • Characterized by less severe symptoms of mania • Clear changes in functioning that are observable to others, but impairment is not marked • No psychotic symptoms are present Manic Episode A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary). Manic Episode B. During the period of mood disturbance and increased energy or activity, 3 (or more) of the following symptoms (4 if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior: At least 3 of the ff: (1 week) • • • • • • • Decreased need for sleep Flight of ideas Increased in goal-directed activity Excessive involvement in pleasurable activities Distractibility Very talkative Inflated self-esteem or grandiosity Hypomanic (4 consecutive days, 3 symptoms) • • • • • • • Decreased need for sleep Flight of ideas Increased in goal-directed activity Excessive involvement in pleasurable activities Distractibility Very talkative Inflated self-esteem or grandiosity Bipolar I Disorder • Meet all successful criteria for MDE and Manic • Or • At least one episode of mania episode Bipolar II Disorder • MDE + hypomania Cyclothymic Disorder • Usually begins in late adolescence or early adulthood and persists for years • During a period of at least 2 years, the adult with cyclothymia has numerous periods of hypomanic symptoms and numerous periods of mild depressive symptoms Rapid-Cycling Specifier • Presence of at least 4 manic or depressive episodes within a year • When this direct transition from one mood state to another happens, it is referred to as rapid switching or rapid mood switching ETIOLOGY OF MOOD DISORDERS Neurobiological Factors • Depression - moderate genetic contribution - about 37% of the variance in depression is explained by genes • Bipolar disorder - high genetic contribution - heritability estimate of 93% Neurotransmitters • MDD - low levels of norepinephrine, dopamine, and serotonin • Mania - high levels of norepinephrine and dopamine, low levels of serotonin Brain Imaging Brain Structures Involved in Major Depression Brain Structure Functional Activation Studies Prefrontal cortex Anterior cingulate Hippocampus Amygdala Diminished Diminished Diminished Elevated Brain Imaging Neuroendocrine System • Overactivity of HPA axis - triggers release of cortisol (stress hormone) • Findings that link depression to high cortisol levels Social Factors • Life events - Some people must be more vulnerable to stress than others - 42-67% report a stressful life event in a year prior to depression onset (e.g. break up, loss of job, death of a loved one) - lack of social support may be one reason a stressor triggers depression Social Factors • Interpersonal Difficulties - High levels of expressed emotion by family members predicts relapse - Marital conflict also predicts depression Social Factors • Behavior of depressed people often leads to rejection by others – Excessive reassurance seeking – Few positive facial expressions – Negative self disclosures – Slow speech and long silences Psychodynamic • Depression – Loss of loved person (object) perceived as rejection/ self-hatred – Rigid superego serves to punished oneself – Caused by anger converted into self-hatred, which in turn leads to depression Psychodynamic • Mania – Viewed as defense against underlying depression – Feelings of worthlessness are converted by means of denial, reaction formation and projection to grandiose delusions Emotional Factors • Affect – High negative affect – Low positive affect Emotional Factors • In response to positive stimuli, depressed individuals experience: – Fewer positive facial expressions – Report less pleasant emotion – Show less motivation – Demonstrate less psychophysiological activity Personality Factors • Neuroticism – Tendency to react with higher levels of negative affect – Predicts onset of depression McCrae and Costa • • • • • Openness to experience Conscientiousness Extraversion Agreeableness neuroticism Personality Factors • Extraversion – Associated with high levels of positive affect – Low extraversion does not always precede depression Personality Factors • Inadequacy – If the child has overbearing, critical and authoritarian parents, it is likely that whatever the child will be will never be enough to please the parent Personality Factors • Anger - those who suppressed their anger has a greater tendency for depression • Dependency on others • Low self-esteem Cognitive View • Depression – Aaron Beck – Negative triad: Self, world, future – Negative schemata: underlying tendency to see the world negatively – Negative schemata cause cognitive biases • Tendency to process information in negative ways Cognitive View • Mania – Individuals denies certain aspects of reality in order to promote or preserve an unrealistic set of self-perceptions – A superficial one that serves to cover up underlying depressed thinking Behavioral View • Learned Helplessness – Martin Seligman – depression results from learning that one’s physical or social environment is beyond one’s personal control – result of three key attributions for negative events: internal, global and stable attributions are likely to lead in depression Behavioral View • Peter Lewinsohn – Depression is a result of low rate of positive social reinforcement TREATMENT OF MOOD DISORDERS Changing the chemistry of the brain • Medication • ECT Medication • Selective Serotonin Reuptake Inhibitors (depression) - Fluoxetine (Prozac) - First treatment choice - Block presynaptic reuptake - Many negative side effects Medication • Mania: Lithium – Hand tremor - Diarrhea – Increased thirst - vomiting – Increased urination - weight gain – Impaired memory - drowsiness – Poor concentration - acne – Muscle weakness - hair loss – Decreased thyroid function Electroconvulsive Therapy • Electroconvulsive Therapy (ECT) - Brief electrical current - Temporary seizures - 6 to 10 treatments - High efficacy - Severe depression - Few side effects - Relapse is common • Immediate side effect: ECT – drowsiness (you may sleep for a while) – confusion – headache – feeling sick – aching muscles – loss of appetite Psychological Treatment • Interpersonal Therapy – Focus on current relationships – The core of the therapy is to examine major interpersonal problems, such as role transitions, interpersonal conflicts, bereavement, and interpersonal isolation. Psychological Treatment • Cognitive therapy – Monitor and identify automatic thoughts • Replace negative thoughts with more neutral or positive thoughts Psychological Treatment • Behavioral Therapy – Increase participation in positively reinforcing activities – Reinforce skills in managing interpersonal situations and environment • Behavioral activation – people are encouraged to engage in pleasant activities that might bolster positive thoughts about one’s self and life. Psychological Treatment • Bipolar: Psychoeducational approaches – Typically help people learn about the symptoms of the disorder, the expected time course of symptoms, the biological and psychological triggers for symptoms, and treatment strategies.