Depression
advertisement

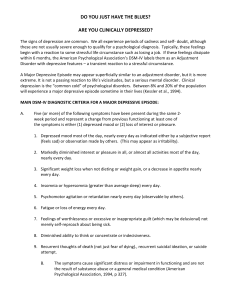
Depression Mood disorders Unipolar Depressive Disorders ○ Major Depressive Disorder Single or Recurrent ○ Dysthymic Disorder ○ Depressive Disorder NOS Bipolar Manic-depressive disorders ○ Bipolar I ○ Bipolar II ○ Cyclothymic Disorder ○ Bipolar Disorder NOS Major Depressive Disorder— DSM-IV Diagnosis One or more episodes Depressed mood OR Anhedonia 4 of 7 additional symptoms Disruption in sleep Appetite (or weight) Concentration Energy Psychomotor agitation OR retardation Excessive guilt or feelings of worthlessness Suicidal ideation Epidemiology Mean age of onset—40 years old Within 1 year—7% (11 million) of Americans will experience a mood disorder 40% comorbid with other psychiatric illnesses/substance-related disorders Associated with medical conditions 25% of pts have chronic, recurrent depression 1 episode puts you at risk for another Risk Factors Prior episode of depression/suicide attempt Family history of depressive disorder/suicide Lack of social support Lack of coping abilities Presence of life and environmental stressors Current substance use and/or abuse Medical comorbidity History sexual abuse Etiology Genetics Common among first-degree biologic relatives Neurobiologic Hypotheses Neuroendocrine & Neuropeptide Hypotheses Cognitive Theory Assessment Key element is change in behavior Most common behavior is depressed mood Screening Tools Beck Depression Inventory Geriatric Depression Scale Mood Depressed Anxiety Physical Changes Anergia Psychomotor retardation Cognition Slow to process ALWAYS assess for Suicidal Ideations!!!!!!!!!! Nursing Diagnoses? Goals Short term: Eliminate symptoms Long term: Lifting of the depressed mood Continuation-prevent relapse Interventions Evidence-based practice recommends antidepressants plus therapies Environmental: safety Nurse-Pt relationship Socialization Cognitive Interventions Help increase sense of control, self-esteem and modify dysfunctional thinking “self-fulfilling prophecy”-victim thinking Explore feelings, define problem, modify thinking Negative thinking Behavioral Interventions Find an activity the pt can be successful at Praise genuine effort Physical exercise ECT Grand mal seizure artificially induced. Pt is sedated, treatments usually 6-12, 2-3x/week, response rate of 80%, usually tried after pharmacotherapy fails, safe for pregnancy. Adverse Effects-headaches, memory difficulties, muscle soreness. Interventions—Pharmacologic Antidepressants SSRIs TCAs MAOIs others Antidepressants SSRI’s Second-generation drugs Newer, more expensive Much less side effects Safer in overdose Side effects: GI, sexual dysfunction, weight gain (some) Serotonin Syndrome Tricyclic antidepressants First-generation drugs Efficacy established Less expensive Side effects: antihistaminic, anticholinergic, orthostasis, cardiac Take at bedtime to minimize side effects SE should subside after a few weeks Lethal in overdose! Monoamine Oxidase Inhibitors (MAOIs) First-generation drugs not used much d/t side effects May precipitate hypertensive crisis Food Cautions Others Serzone, Effexor, Wellbutrin, Trazodone Trazodone-mostly for insomnia Wellbutrin-marketed as Zyban for smoking cessation, potential for seizures Different side effect profiles, still less than TCA’s Complementary and Alternative Therapies For Depression: St. John’s Wort Melatonin Omega 3 fatty acids Acupuncture Massage Exercise Meditation Yoga Phototherapy Other Types of Depression Major Depression Postpartum depression Seasonal Affective Disorder (SAD) Dysthymic Disorder— DSM-IV Diagnosis Depressed mood for most days for at least 2 years 2 or more of following symptoms Poor appetite or overeating Insomnia or oversleeping Low energy or fatigue Low self-esteem Poor concentration or difficulty making decisions Feelings of hopelessness Suicide Epidemiology 1 person every 17 minutes commits suicide in United States 80 suicides a day in United States 1000 suicides a day worldwide Risk Factors Gender Age Psychiatric Dx-Mood D/O, Substance Abuse, Schizophrenia, Anxiety D/O ETOH associated with 25-50% Lack of social support Family hx of suicide Loss Assessment “Have you thought about killing yourself?” “Do you have a plan?” Are the means to carry out this plan available to the pt? Assess plan for lethality Contract for safety Elopement risk Attempt history Goal Pt will not harm self. Interventions Safety: 1:1, close observation, 15 minute checks Remove objects such as belts and shoelaces, mirrors, etc. Contracting Monitor medications Resources www.depression-screening.org Confidential screening tool www.nami.org National Alliance for the Mentally Ill www.med.nyu.edu/psych/screens/depres.html Short assessment