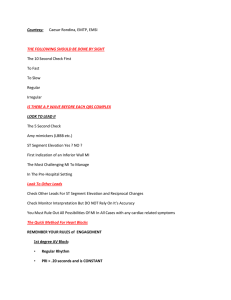
Ekg notes SA node (60-100) AV node (40-60) bundle of his (40-60) bundle branches (20-40)- Purkinjean fibers (20-40) Normal Sinus Rhythm EKG Readings: Rhythm: normal Rate: 60-100 beats per minute P-wave: rounded, small, up-right, 1:1 with QRS PRI: constant throughout the strip, 0.12-0.20 QRS: 1:1 with p-wave, less than 0.12 Treatment None Causes Healthy Sinus Bradycardia EKG Reading Rhythm: normal Rate: less than 60 P-wave: upright, rounded, small, 1:1 with QRS PRI: constant throughout, 0.12-0.20 QRS: 1:1 with p-wave less than 0.12 Signs and Symptoms Hypotensive Pale, clammy, pale Weakness Syncope Angina Treatment: Atropine (increases heart rate) o Only if symptomatic (low perfusion, clammy, pale, cool) Pacemaker Causes: Too medication (beta-blockers, calcium channel blockers, or digoxin) Old age Athletes (but this does not consider life-threatening) MI Pericarditis Obstructive sleep apnea Hypothyroidism Increased intracranial pressure Sinus Tachycardia EKG Reading Rhythm: normal Rate: greater than 101-200 P-wave: upright, rounded, small, 1:1 with QRS PRI: constant throughout, 0.12-0.20 QRS: 1:1 with p-wave less than 0.12 Signs and Symptoms Hypotensive Patient’s activity tolerance will be low Dizziness Dyspnea Increased myocardial oxygen consumption Increased heart rate Treatment: Need OLDCART to rule angina (chest pain aka heart attack) Medication o Beta blockers, drugs that end in “lol” Decreased heart rate by binding to beta receptors in the heart o Calcium channel, drugs that end in “pine” or “zem” Relax the blood vessels and decrease heart workload o Vagal maneuver Bare down Carotid massage o Causes: stress, anemia, hypotension, hypovolemia, HF, hyperthyroid, medications Pacemaker Pacemaker: artificial electronic device used to pace the heart Different types Implanted in the chest pall External/transcutaneous ( epicardial pacing wires) Different pacing o On demand only gives a shock if an abnormal heart rate is detected and then will shut off o Fixed: constantly pacing with no regards to the patient’s heart rate Atrial Fibrillation (AFib) “fibrillation flopping Definition: un-controlled electrical; activity in the atria that causes rapid and disorganized twitching of the atrial musculature or main pacemaker, SA node has lost control EKG Reading Rhythm: irregular Rate: greater than 350-600 o Controlled: ventricular rate that is less than 100 o Uncontrolled: ventricular rate is more than 100 P-wave: not present F-wave: not present PRI: not present QRS: normal, present, 0.06-0.12 Signs and Symptoms Chest pain Oxygen low Lethargic Low BP Anxiety Palpitations of the chest Shortness of breath Elevated ventricular activity or HR Dizziness Treatment: Medication o Beta blockers, drugs that end in “lol” Decreased heart rate by binding to beta receptors in the heart o Calcium channel, drugs that end in “pine” or “zem” Relax the blood vessels and decrease heart workload o Digoxin: increases heart’s contractility and decreases heart rate Be aware of toxicity levels (normal range 0.8-2.0) Signs of toxicity: green halo effect Always check heart before administration, if is less than 60 beats per min DO NOT give Those with low potassium are at risk for digtoxity (3.5-5.0) o Anticoagulants: given if in A-Fib for longer than 48 hours WAD Warfarin-Coumadian Vitamin K antagonist, so it can promote clotting and reduce effectiveness of Warfarin Tell patient to keep Potassium consumption (green leafy) intake the same Check INR levels (2.5-3.5) important for patients with bleeding disorders Dabigatran Apixaban o Antidysrhythmic (p 3-6 months 50% have recurrance of AF) Amiodarone: slow the nerve impulses in the heart. Flecanide Dofetalide Cardioversion : given if in A-Fib for less than 48 hours o Done after TTE to rule out clots o 200-360 o Must be synchronized with patient’s heart rate o Nursing considerations Perform after TTE Skin integrity Patient’s pain tolerance Causes: After heart surgery Heart failure Pulmonary issues: COPD HTN Alcohol Atrial flutter “A FluTTer = sawtooth” Definition: similar to A-Fib, but the electrical signals spread through atria in a fast but regular rhythm EKG Reading Rhythm: regular Rate: greater than 75-150 P-wave: not present F-wave: present throughout (look like teeth or saws) PRI: not present QRS: normal, present, 0.06-0.12 Signs and Symptoms Chest pain Oxygen low Lethargic Low BP Anxiety Palpitations of the chest Shortness of breath Elevated ventricular activity or HR Dizziness Treatment: Medication o Beta blockers, drugs that end in “lol” Decreased heart rate by binding to beta receptors in the heart o Calcium channel, drugs that end in “pine” or “zem” Relax the blood vessels and decrease heart workload o Digoxin: increases heart’s contractility and decreases heart rate Be aware of toxicity levels (normal range 0.8-2.0) Signs of toxicity: green halo effect Always check heart before administration, if is less than 60 beats per min DO NOT give Those with low potassium are at risk for digtoxity (3.5-5.0) o Anticoagulants: given if in A-Fib for longer than 48 hours Warfarin-Coumadian Vitamin K antagonist, so it can promote clotting and reduce effectiveness of Warfarin Tell patient to keep Potassium consumption (green leafy) intake the same Check INR levels (2.5-3.5) important for patients with bleeding disorders Dabigatran Apixaban o Antidysrhythmic (p 3-6 months 50% have recurrence of AF) Amiodarone: slow the nerve impulses in the heart. Flecanide Dofetalide Cardioversion : given if in A-Fib for less than 48 hours o Done after TTE to rule out clots o Must be synchronized with patient’s heart rate o Nursing considerations Perform after TTE Skin integrity Patient’s pain tolerance Causes: Cardiomyopathy Atrial dilation Valve disease Thyroxicities Hypoxia CHF ETOH use 1st degree AV block Definition: delay in conduction of electrical impulse, usually through the AV Node EKG Reading Rhythm: Regular Rate: 60-100 P-wave: present, 1:1 with QRS PRI: present but longer than 0.20 QRS: normal, present, 0.06-0.12 Signs and Symptoms Most common Heart Block Patients are more likely to be asymptotic Some may experience: o Chest pain o Oxygen low o Lethargic o Low BP o Anxiety o Palpitations of the chest o Shortness of breath o Elevated ventricular activity or HR o Dizziness Treatment: Atropine o Increases Heart rate Causes: Hyperkalemia Too much medication o Beta blockers Increases heart rate o CCB Decreses vessel contractility and heart workload Acute inferior Wall MI Ischemic Heart Disease Digitalis Toxicity Second degree AV block Type 2 “missing QRS”, more p’s than QRS Definition: a disease of the distal conduction system (His-Purkinje system) In 2nd Degree, Type I, the HALLMARK IS that the PRI gets PROGRESSIVELY PROLONGED, UNTIL THE QRS IS DROPPED, then the PATTERN begins again Very high potential to convert to Third Degree (Complete) Heart Block Complete block of conduction in one bundle branch and an intermittent block in the other bundle branch EKG Reading Rhythm: irregular Rate: atria rate faster than slower ventricular rate (more p-waves), but its slow P-wave: present, 2:1 OR 3:1, TOO MANY PRI: 0.12- 0.20, normal or prolonged QRS: missing, but if present is normal, but may be prolonged Signs and Symptoms Patients some patients asymptotic but very rare Chest pain Oxygen low+ tachycardia Lethargic Low BP Anxiety Palpitations of the chest Shortness of breath Elevated ventricular activity or HR Dizziness Treatment: Atropine is NOT Effective Stop drugs or decrease o Beta blockers o Calcium channels o Digoxin May require Pacemaker Causes: Damage to the Bundle branches MI Third degree AV Block Definition: complete absence of conduction of electrical impulse through AV node, Bundle of His, and Bundle Branches Atria rhythm independent from ventricular rhythm; regular P-P and regular R-R Life-threatening rhythm, will lead to asystole EKG Reading Rhythm: regular, but P wave and QRS contract independently Rate: slow 40-60 P-wave: normal PRI: varies QRS: normal or wide ST segment: does a little upward “/” Signs and Symptoms Chest pain Oxygen low Lethargic Low BP+ tachycardia Anxiety Palpitations of the chest Shortness of breath Elevated ventricular activity or HR Dizziness *symptoms get progressively worst as heart block progresses* Treatment: Pacing Stop drugs that decrease heart rate Atropine to increase heart rate Dopamine to increase blood pressure Epinephrine which increases heart rate, increased Blood pressure and cardiac output to increase oxygen to the body Causes: Too medication o Beta blockers o Calcium channel blockers o Digoxin MI Inferior wall MI Ischemic heart disease Hyperkalemia Bundle Branch Block “bunny ears” Definition: irregular conduction or block of electrical pathway through bundle branches (aka. Purkinje fibers” Ventricles do not contract simultaneously EKG Rate: depends Rhythm: regular P wave: normal PR interval: normal (because atrium is not involved) QRS: wide or appear notched (bundles lead to ventricles), larger than 0.12 o Notes to self: T-wave or impacted, appear downwards Signs and Symptoms Sometimes patient does not show symptoms Subjective o I feel light-headed or I might pass out” Objective o Chest pain o Oxygen low o Lethargic o Low BP+ tachycardia o Anxiety o Palpitations of the chest o Shortness of breath o Elevated ventricular activity or HR o Dizziness Treatment: Pacing (for extreme cases) o Patient education Cardiac resynchronization: wire connected to both sides of the heart Fall risk interventions Echocardiography Causes: CAD Anterior wall MI HTN Scar tissue Drug toxicity Congenital heart defects PVC “Premature Ventricular Contraction” ventricular sneeze *** may lead to V tach or V fib*** EKG Readings Rate: depends Rhythm: irregular when PVC occurs P-wave: none associated with PVC PR: not associated with PVC QRS: wide without a p-wave and bizarre looking o May indicate a presence of ventricular abnormality Cause: Increased catecholamine (released during stress response) increased sympathetic tone (related to stress) Stimulants Amphetamine and cocaine Myocardial ischemia or infraction CHF Hypoxia Acidosis Dig toxicity Hypokalemia Hypo magnesium Signs and Symptoms Isolated PVC without history of heart disease are insignificant Multipliable o Subjective: heart is pounding or skipping o Objective: Low Blood Pressure Treatment: Identify causes Medications o Lower/ discontinue digoxin o Amiodarone: relax heart o CCB or BB MAYBE Correct electrolyte imbalance o Potassium and magnesium V-Tach “looks like tombstones” Definition: Dysrhythmia originating in an ectopic pacemaker in the bundle branches, purkinje fibers, or ventricular myocardium ** More than 3 PVCs is sustained V Tach** ** Monomorphic or polymorphic(Torsades de Pointes)** Increased frequency can lead to Ventricular Fibrillation which is LIFETHREATENING PULSELESS V TACH IS TREATED THE SAME AS V FIB! EKG Reading Rhythm: irregular Rate: 100-250 P-wave: absent PRI: absent QRS: wide and bizarre Causes Stimulants hypoxia Dig toxicity Electrolyte imbalance: low potassium and magnesium Cardiac injury: MI or heart attack Signs and Symptoms: COLLSPSED Can be short and asymptomatic Treatment: Determine onset and termination Pulse give them amiodarone than cardioversion o Amiodarone to stabilize rhythm and then give cardioversion Pulseless o Call a code o Defibration V-Fib “ squggly lines” Definition: no coordinated ventricular beats are present EKG Reading Rate:300-500 Rhythm: chaotic P-wave: none PRI: none QRS: none o None because ventricles are not fully contracting and cardiac output CEASES Causes: Untreated V-TACH Cardiac injury : post MI Med toxicity Electrical imbalances o Untreated V-Tach, acid-base, electrolyte imbalances, electrical shock Signs and Symptoms COLLSPSED if patient is conscious Usually, patient is not conscious! Treatment Cardioversion (pulse) and Defibrillation(no pulse) Medical Management Atropine Vasopressors Anti-dysthymias Nursing Considerations o Oxygen, Pain management. LAM drugs Asystole or cardiac standstill “flat line” Definition: total absence of electrical activity in the heart, patient is clinically dead ***if patient is talking they are NOT in asystole*** EKG: Rate: none Rhythm: none P-wave: none PRI: none QRS: none o FLATLINE Causes Trauma Un resolved V-tachycardia Signs and symptoms: None, patient is dead Treatment CPR Epinephrine, IM or IV push 10 mL every 3 to 5 minutes What not to do o Give defibrillation Shock needs an electrical impulse to piggyback off of Pulseless Electrical Activity Definition: rhythm present without a pulse Causes: Hypoxemia Hypovolemia Treatments: Call a code Start CPR ACL measures PEA o ATROPINE (IF BARDYCARDIA) o VASSOPESSIN AND EPI PEA o Push epi always o Medications to be aware Atropine “at the top” Function: o Increases heart rate o Blocks the parasympathetic nervous system effects of the heart o Accelerates SA node rate o Increases conduction velocity Administration o IV bolus Indications o Symptomatic bradycardia o First degree AV block o Second degree AV block type 1 Vasopressor Function: vasoconstriction of the arterioles and venous circulation Increases HR Increases the strength of contraction Examples of Drugs “ine: o Vasopressin o Dopamine o Norepinephrine o Dobutamine o Isoproterenol Anti-dysrhythmia Adenosine: suppresses AV and SA node activity Indications o SVT and tachycardia o A-Fib and A-Flutter: but will not terminate it Amiodarone Effects the NA, K, and Ca channels Effective for SVT, VT, V-fib Lidocaine Effective for VT Side effects o Altered consciousness o Bradycardia o Seizures Procainamide (it’s a pro) Suppresses atrial and ventricular dysthymia by slowing down in conduction Used for VT, controls a-fib/a-flutter, PVST Calcium Channel blockers Function: decreases conduction and increases conduction time in AV node Used with Beta-Blocker therapies Indications: Used in A-fib and A-flutter Contradictions: Second Degree AV blocks and Third Degree AV blocks Use with caution in those with Hypotension and CHF