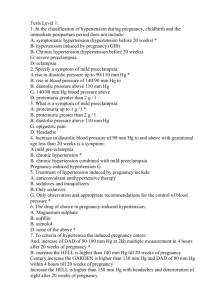
Cardiac Disorders: Functional cardiac status changes in pregnancy 1. 2. 3. 4. Increase in intravascular volume Decreased systemic vascular resistance Cardiac output changes during labor and delivery Intravascular volume changes that occur after delivery Heart disease classification Class 1- asymptomatic with normal levels of activity Class 2- symptomatic with normal levels of activity Class 3- symptomatic with less than ordinary activity Class 4- symptomatic at rest o Determined at 3 mo. And again at 7-8 mo. Progression may occur Risk factors Maternal arrythmias Heart failure Preterm birth Fetal growth restriction Fetal/maternal death (small risk) Complications Peripartum Cardiomyopathy o Development of CHF in the last month of pregnancy or withing the first 5 months post-partum. o From extra fluid during pregnancy o Presents with dyspnea, cough, orthopnea, tachydysrhythmias, edema and cardiomegaly o Treat with diuretics, Na+ restriction, afterload-reducing agents, anticoagulants, and digoxin o Usually goes away on own, will need cardiologist monitoring after pregnancy for 6 mo. o Antepartum care Limit activity Daily weight I+O Infection prevention Nutrition (iron, folic acid, high protein, Na+ restriction) Stool softeners, fiber Meds as needed, heparin or lovonox only for pregnancy Cardiac Decompensation o Presents with increasing fatigue, difficulty breathing, smothering feeling, frequent cough, palpitations, edema, irregular weak rapid pulse (>100 b/m) crackles at base of lung, orthopnea, rapid respirations, moist frequent cough, cyanosis o Intrapartum care ECG Monitoring, continuous O2 BP and fetal monitoring, Resp. status monitoring, hemodynamic monitoring, ABG’s Goal to prevent hypotension, optimize cardiac output, prevent tachycardia Maintain volume, positioning, epidural to decrease workload, induction, Valsalva maneuver, open glottic pushing, operative vaginal delivery (forceps/vacuum) bacterial endocarditis prophylaxis o Postpartum care Assess: hemodynamic (cardiac output, BP, ABG) )2 sat, lung and heart sounds, edema, uterine tone and fundal height, lochia, urinary output, pain Progressive activity, encouraging side lying position, prevent constipation, pain management, meds (cardiac and diuretics) Hypertensive Disorders: Definitions Gestational Hypertension o Onset of hypertension without proteinuria after 20 weeks Preeclampsia/Preeclampsia with severe features o Pregnancy specific, hypertension develops after 20 weeks with proteinuria, proteinuria not always, may also have thrombocytopenia, impaired liver function, new-onset renal insufficiency, pulmonary edema, new-onset cerebral or visual disturbances. Eclampsia o Seizure activity or coma in women with preeclampsia, no hx of preexisting condition, can occur before, after or during birth. Chronic hypertension o Present before pregnancy or diagnosed before 20 weeks Chronic hypertension with superimposed preeclampsia o Hypertension and acquired preeclampsia Hypertension in Pregnancy Classification: SBP >140mmHg DBP >90mmHg MAP >105mmHg, dx onset during pregnancy recorded on 2 separate occasions 4-6 hr apart, proteinuria (30mg/dL or more on 2 random specimens collected 6 hr apart or 24 hr collection of 300mg/dL)(dipstick, +1=30mg/dL +2=100 +3=300 +4=1000) Chronic Hypertension Maternal complications o Superimposed preeclampsia, stroke, acute kidney injury, heart failure, placental abruption, death Fetal complications o Perinatal death, preterm birth, SGA, IUGR Postpartum: high risk women monitored for complications such as renal failure, pulmonary edema, heart failure, encephalopathy Management before conception ideally. Lifestyle changes Meds: Methylopa, labetalol, nifedipine, no ACE inhibitors Gestational Hypertension Hypertension w/o proteinuria after 20 weeks or in the first 24 hours after birth w/o other s+s of preeclampsia and preexisting HTN BP returns to normal w/in 6 weeks of birth Managed with rest and antihypertensives Preeclampsia Development of hypertension and proteinuria after 20 weeks or early postpartum. In absence of proteinuria may have thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema, cerebral or visual symptoms. Risks: o Nulliparity, >40 years, assisted fertility, greater than 7 years between pregnancy, hx of preeclampsia, SGA, obesity, GDM, preexisting medical condition, renal disease, chronic hypertension, type 1 DM Complications o Maternal: cerebral edema hemorrhage or stroke. DIC, pulmonary edema, CHF, renal failure, abruption o Fetal: SGA, IUGR, pre-term, mortality 10-20% Manifestations o BP >140/90 x2 at least 4 hr apart after 20 weeks, proteinuria >300mg in 24 hr specimen and >1+ on dipstick, platelet <100,000/uL, elevated liver enzymes, increased creatine o w/ severe features: BP >160/110, massive proteinuria >5g in 24 hr specimen, <100,000 platelets, elevated liver enzymes, renal insufficiency, cerebral or visual disturbances, pulmonary edema. Prevention o Aspirin. 81mg daily starting between 12-28 weeks Interventions o Bedrest, high protein and low sodium diet, frequent BP assessment, daily weight, daily fetal movement assessment, NST 1-2 times per week BPP as needed o w/ severe features: decrease stimuli, FE replacement, seizure precautions, mag sulf, deliver at 34 if possible. HELLP Syndrome o Hemolysis, Elevated Liver enzymes, Low Platelets o Associated with preeclampsia with severe features. o Hemolysis due to distorted or fragmented RBC’s damaging blood vessels. Elevated liver enzymes from obstructed flow from fibrin deposits. Low platelets from vascular damage with vasospasm and platelet aggression. o Increased risk for: Pulmonary edema, renal failure, liver hemorrhage or failure, DIC (disseminated intravascular coagulation) placental abruption, acute respiratory distress syndrome, sepsis, stroke, fetal/maternal death Magnesium Sulfate o Decreases CNS irritability, helps to prevent seizures. o May have bolus or continuous o Side effects Lethargy, weakness, sweating, warm feeling, N/V, constipation, headache, slurred speech o Toxicity Decreased DTR, oliguria, confusion, slowed respirations (less than 12) o Interventions: VS every hour, DTR assessment every hour, monitor I+O, monitor serum mag, fetal monitoring o Calcium Gluconate antidote Postpartum Care o Assess VS, I+O, DTR, LOC o Mag sulfate infusion after birth for seizure precaution usually 24 hour. o Assess regularly for s+s of preeclampsia Eclampsia Seizure activity or coma in woman diagnosed with preeclampsia, no hx of previous activity o Preceded by: persistent headache, blurred vision, severe epigastric pr right upper quadrant pain, ALOC. Tonic clonic