Pressure Injury Prevention: Risk, Assessment, & Interventions
advertisement

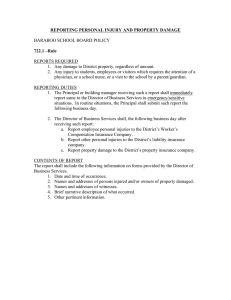
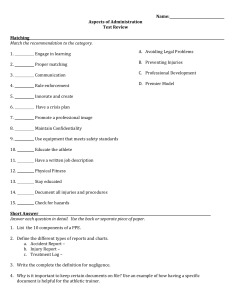
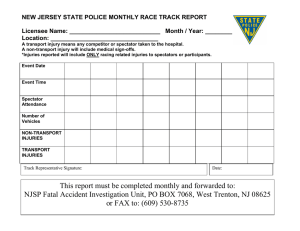
Pressure Injury Prevention 17 North Quality Assurance and Process Improvement Project 2017 Cheryl Koller RN, BA Lead Educator Objectives: How to perform a thorough skin assessment Identify the risk factors for pressure injury development Identify medical devices that have the potential to cause pressure injuries Identify interventions for pressure and mucosal injury prevention How to properly position patients to off set pressure Identify transfer and positioning aids to reduce friction and shear How to select appropriate support surfaces based on pressure injury risk Identify the different types and stages of pressure and mucosal injuries Definitions: Pressure Injury: A pressure injury is localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue. Medical Device Related Pressure Injury: This describes an etiology. Medical device related pressure injuries result from the use of devices designed and applied for diagnostic or therapeutic purposes. The resultant pressure injury generally conforms to the pattern or shape of the device. The injury should be staged using the staging system. Mucosal Membrane Pressure Injury: Mucosal membrane pressure injury is found on mucous membranes with a history of a medical device in use at the location of the injury. Due to the anatomy of the tissue these ulcers cannot be staged. 17 North Pressure Ulcers/Injuries 2013-2017 Stage I Stage II Stage III Stage IV Unstagable DTI Total 2013 2014 2015 2016 7 6 1 7 7 1 5 1 14 21 2 2 2 18 6 1 2 4 44 1 1 9 9 2017 Total 17 North Pressure Ulcers 2013-2017 8 7 6 5 4 3 2 1 0 Stage I Stage II Stage III 2013 Stage IV 2014 2015 2016 2017 Unstagable DTI Performing A Skin Assessment All patients should have a thorough skin assessment upon admission, with each routine physical assessment, upon transfer to a new a unit and with changes in the patient’s condition. Skin is assessed from head to toe. All surface areas should be looked at for abnormalities. Special attention should be placed on bony prominences and under medical devices. Medical devices should be moved or removed (if able) and assessed underneath. Pressure Injury Risk Factors: A population specific pressure injury risk assessment is completed on admission for all patients admitted to Stony Brook Medicine. In addition, it is completed with every routine physical assessment, upon transfer to a new unit and with changes in the patient’s condition. Our current pressure injury risk assessment tool is the Braden Scale. The Braden Scale scores a patient based on: Level of Sensory Perception Moisture Status Activity Level Mobility Nutritional Status Risk of Friction and Sheer Injury Any patient with a Braden Score of 18 or less is considered at risk for pressure injury. Medical devices also have the potential to cause pressure injuries. Medical Devices: Hospitalized patients often require the use of a multitude of medical devices to assist in their care and treatment. Some common medical devices that place patients at risk for pressure injury are: Intravenous Lines Drain Tubing Endotracheal Tubes Tracheostomy Ties Nasogastric Tubes Oxygen Tubing BiPAP/CPAP Masks Retention Sutures Foley Catheters Pressure Injury Prevention Measures: Pressure Injury Prevention Power Plan should be ordered and initiated for all At Risk patients Turning and Positioning at least every 2 hours Use of positioning devices: Wedges Z-Flow cushions and pillows Tortoise Pads Patients should be positioned at a 30 degree tilted side lying position alternating between left, right and back (unless contraindicated due to medical condition). Heel elevation or Z-Flex boots Placement on appropriate pressure relief bed: Versa Care Total Care Sport Bed (for patients requiring frequent respiratory percussion) P-500 (Braden for score of < 15) Tempurpedic (for use in patients with unstable spines) Bariatric (for patients > 350lbs) Pressure Injury Prevention Measures: Prevent friction and shear Mepilex Dressings: Sacral Heel 2x6 Border for spine 4x4 Border for additional bony prominences (Mepilex should be changed every 3 days and as needed) Head of bed at or < 30 degrees If head of is >30 degrees, the foot of bed should be elevated Use of draw sheet, Comfort Glide sheet, or Tortoise pad for lifting and positioning Ensure patient is receiving appropriate nutrition (refer for nutrition consult as needed): NPO Status Pre-Albumin with C-Reactive Protein/Albumin levels Pressure Injury Prevention Measures: Moisture Prevention: Moisture barrier ointment every 8 hours and as needed Avoid use of diapers and plastic chux Use air flow chux Purewick urinary collection device for females * Remember…Bed/Fed/Red/Tread Prevention of Medical Device Related Pressure Injuries: Correct size of the device to fit the individual Cushion and protect the skin area. Examples include: Mepilex under trach ties Mepilex on pressure areas under Bi-PAP/CPAP masks Nasogastric tube holders instead of tape Remove devices and assess the skin during routine physical assessment and for changes in patient status (i.e edema to extremities) Avoid placement over bony prominences and previous pressure injury sites Ensure tubing and drains are not directly under the individual Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Types and Stages of Pressure Injuries: Updated Staging and Definitions: Stage 1 Pressure Injury: Non-blanchable erythema of intact skin Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple or maroon discoloration; these may indicate deep tissue pressure injury. Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible and deeper tissues are not visible. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions). Updated Staging and Definitions: Stage 3 Pressure Injury: Full-thickness skin loss Full-thickness loss of skin, in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury. Stage 4 Pressure Injury: Full-thickness skin and tissue loss Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole (rolled edges), undermining and/or tunneling often occur. Depth varies by anatomical location. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury. Updated Staging and Definitions: Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar (i.e. dry, adherent, intact without erythema or fluctuance) on the heel or ischemic limb should not be softened or removed. Deep Tissue Pressure Injury: Persistent non-blanchable deep red, maroon or purple discoloration Intact or non-intact skin with localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss. If necrotic tissue, subcutaneous tissue, granulation tissue, fascia, muscle or other underlying structures are visible, this indicates a full thickness pressure injury (Unstageable, Stage 3 or Stage 4). Do not use DTPI to describe vascular, traumatic, neuropathic, or dermatologic conditions. Updated Definitions and Staging: Additional pressure injury definitions. Medical Device Related Pressure Injury: This describes an etiology. Medical device related pressure injuries result from the use of devices designed and applied for diagnostic or therapeutic purposes. The resultant pressure injury generally conforms to the pattern or shape of the device. The injury should be staged using the staging system. Mucosal Membrane Pressure Injury: Mucosal membrane pressure injury is found on mucous membranes with a history of a medical device in use at the location of the injury. Due to the anatomy of the tissue these ulcers cannot be staged. Documentation and Notes: Pressure injuries should be documented in I-View assessment immediately upon discovery and a focus note titled “Altered Skin Integrity” must be written to document the abnormal findings. If a pressure injury is discovered upon transfer the transferring unit should be notified by the receiving nurse and should be documented in the acceptance note. A Skin Assessment Sticker should be filled out and signed by 2 nurses verifying the patient’s pressure injury status. All pressure ulcers should be measured and continuously monitored for changes in status. Stage 1and 2 pressure injuries must be verified in I-view by an ET champion. Stage 3, stage 4, unstageable, and deep tissue injuries must by verified by the ET nursing staff. A pressure injury can never be down staged (ex. A stage 3 will never become a stage 2 or 1 even as it heals and improves). References: Stony Brook Medicine Administrative Policy and Procedure https://policymanager.uhmc.sunysb.edu/dotNet/documents/?docid=7274 https://policymanager.uhmc.sunysb.edu/dotNet/documents/?docid=1261 National Pressure Ulcer Advisory Panel http://www.npuap.org/