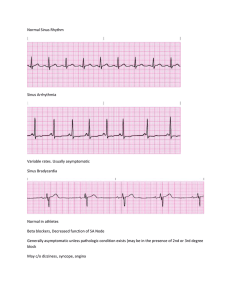
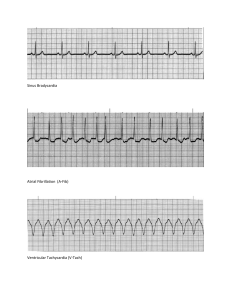
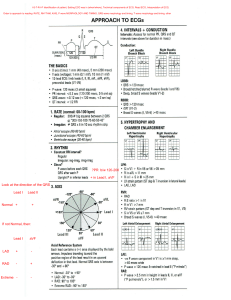
ARRHYTMIAS AND THEIR CONSEQUENCES. Normally, heart work depends on normal automatism (conditions of driver sino-atrial node), excitability, conductive heart system condition and contractive myocardium properties: Arrhythmia is the condition, which is characterized by the violation of such heart physiological properties, as automatism, conduction of impulses through conductive ways, contractive myocardium properties by the violation of heart ability to learning of excitation rhythm, by the violation of frequency, rhythm or coordination of heart beats. Etiology of heart rhythm disorder The rhythm violations arise under the influence of different pathological agents, which can be divided on such groups: 1) Functional violations and influences, for example: violation of vegetative nerves system condition (sympathetic or parasympathetic link hyperactivity), physical work, physical overload, body temperature changes, the increase of intracranium pressure, respiration (especially in children); 2) Organic injury of myocardium, for example: inflammation of myocardium (as the result of infection), the myocardium dystrophy (in the result of hypoxia, ischemia or amiloidosis), necrosis of myocardium; 3) Influences of toxic substances on the myocardium (alcohol, drugs, big dose adrenalin and noradrenalin, glucocorticoids, bacterial toxins, phosphororganic substances); 4) Hormone balance disorder (hyperthyroidism, hypothyroidism, hyperfunction of supranephral glands); 5) Violation of intracellular or extracellular ions balance (changes of sodium, potassium, calcium, magnesium and chlorine concentration); 6) Mechanical influences on the heart (catheter using for the diagnosis and treatment heart diseases, operation on the heart, chest trauma). Pathogenesis of heart rhythm disorder Ability to automatic impulses formation depends on pacemaker cells activity of the sinoatrial node, in which spontaneous slow depolarization of cells membrane takes place during diastole. As the result, action membrane potential arises after achievement of some critical level (threshold level critical potential). Impulses generation depends on maximum diastolic potential of these cells, on maximum diastolic potential measure, after which action membrane potential arises, and on speed of slow diastolic depolarization. The decrease of the threshold level maximum diastolic potential SA node p-cells or/and slow diastolic depolarization speed increase stimulates of the sinus tachycardia appearance at body temperature increase, in the result of sympathetic stimulation or withdrawal of vagal tone. On the contrary, decrease of speed slow spontaneous diastolic depolarization or/and increase threshold level critical potential and hyperpolarization in diastole causes the sinus bradycardia. Tone oscillations of n. Vagus at breathing time can induce the sinus respiratory arrhythmia (increase of hear beats during the inspiration). Respiratory arrhythmia in norm is in children, but now very often can be observed in adult. Own automatism of lower part conductive heart system can appear in pathological conditions (arises so-called heterotopic or ectopic rhythm driver). That condition is the result of the automatism sinoatrial node ability decrement, so generation of the impulses arises in another myocardium conductive parts, new ectopic automatism driver appears. Beginning such automatism driver is the result damage of the different part conductive system, or electrical heterogeneous of myocardiocytes, or electrical unstable of myocardiocytes (especially in fourth phase action potential during formation of the resting membrane potential). In that cases extraordinary heart contractive or only ventricles arises (extrasystole). There are three mechanisms of the new ectopic rhythm driver appearance. 1. Appearance of the injured electricity in myocardium. It is the result of electrical heterogeneous myocardiocytes. So, between the uninjured myocardium (membrane charge is -90 mV – membrane resting potential) and injured one (membrane is partly or totally depolarized, membrane charge, for example, is 0 mV or +20 mV) arises difference of the potential and it is the reason of the ectopic rhythm beginning. 2. Ectopic rhythm driver activation. It is the result of electrical unstability myocardiocytes and beginning in one case of the subthreshold level oscillations (unstable low amplitude oscillations of the resting membrane potential) and in other one - the beginning of overthreshold level oscillations (at the retardation or breaking of repolarization). 3. Re-entry mechanism. Under normal conditions, an electrical impulse is conducted through the heart in an orderly, sequential manner. The electrical impulse then dies out and does not reenter adjacent tissue because that tissue has already been depolarized and is refractory to immediate stimulation. However, under certain abnormal conditions, an impulse can reenter an area of myocardium that was previously depolarized and depolarize it again. There three conditions are the necessary for this mechanism beginning: 1 – two conductive ways are the functionally or anatomically disconnected; 2 – some conductive way is blocked; 3 – the antegrade conductive way is blocked, but the retrograde one is preserved. So, in that condition impulse (or impulses) travels numerous through some area of conductive system and returns through another pathway to the reactivated myocardiocytes. Classification of heart rhythm disorders The classification of heart arrhythmia types is based on the main heart properties violations. 1. Automatism violations. There are two groups of arrhythmias, which arise in the result of sinus-atrium node functional state violation. The first group is named nomotopic automatism violation and includes sinus tachycardia, sinus bradycardia and sinus arrhythmia. The second group is named heterotopic automatism violation and includes atrium-ventricular rhythm and idioventricular rhythm. 2. Conduction violations. There are two groups. The first group conduction violation unites block: sinus one, atrium one, atrium-ventricular one, ventricle one. The second group includes Wolf-Parkinson-White syndrome (pre-excitations syndrome). 3. Arrhythmias in the result of combined heart properties violations (automatism, conduction and excitability). This group unites extrasystole, paroxysmal tachycardia, atria flutter, ventricle flutter, atria fibrillation, and ventricle fibrillation. Automatism violations Nomotopic (sinus node) rhythms. 1. Sinus tachycardia refers to a rapid heart rate (> 100 to 180 beats per minute) that has the origin in the SA node. The main reasons are physical or emotional stress, myocardial ischemia or infarction, myocardial dystrophy, congestive heart failure, fever, hyperthyroidism, pharmacological agents (atropine, isoproterenol, adrenalin), compensatory response to decreased cardiac output. ECG sings: all waves have normal configuration and priority, P wave and PR interval (0.12 to 0.20 second) precedes each QRS complex (sinus rhythm), all R-R are shortened. Sinus tachycardia 2. Sinus bradycardia describes a slow heart rate (< 60 to 40 beats per minute) that has the origin in the SA node. It may be normal in trained athletes who maintain a large stroke volume, during sleep; in pathological condition after influenza or typhoid, intracranium pressure rise, irritation of the n. Vagus nucleases, may be an indicator of poor prognosis in patient with acute myocardial infarction that is associated with hypotension. ECG sings: all waves have normal configuration and priority, normal P wave and PR interval precedes each QRS complex (sinus rhythm), all R-R are lengthened. This arrhythmia may cause heart output decrease and leads to cerebral or coronary blood flow insufficiency, in that condition ectopic pacemaker could be activated. Sinus bradycardia 3. Sinus (respiratory) arrhythmia is characterized by gradually lengthening (at expiration) and shortening (at inspiration) R-R intervals and is the result of intrathoracic pressure changes during respiration. It is the normal for the children and can occur in adult after influenza, at neurocirculative dystone, hypertension, congestive heart failure, diabetes mellitus. ECG sings: sinus rhythm, difference of all R-R is more than 0.15 second (at norm difference of all R-R is less than 0,15 sec). Sinus (respiratory) arrhythmia Heterotopic rhythms. They are the result of ectopic automatism driver activation that is localized out SA node (for example, in atrium, in AV-node or in ventricle) because SA node failure (reasons - digitalis toxicity, myocardial infarction, acute myocarditis, excessive vagal tone, hyper- or hypokalemia). 1. Tardy ectopic rhythm (vicarious, passive) arises at the SA node arrest. ECG sings: heart beats not more 60 per minute. If ectopic pacemaker is localized in atrium on ECG inverted P wave is observed before QRS. If ectopic pacemaker is localized in AV node on ECG inverted P wave is observed after normal QRS, or hidden in QRS (atrial-ventricular rhythm). If ectopic pacemaker is localized in ventricle heart rate is less then 40 per minute, QRS is deformed (wide, distorted), it is so called idioventricular rhythm. 2. Unparoxismal tachycardia begins and ends gradually, heart rate is 90 – 130/min. Ectopic driver may be localized in atrium, in AV node or in ventricle. So, complex PQRST has sings of nonsinus rhythm (alteration of configuration, duration and succession waves) 3. Migration of supraventricular rhythm driver is characterized by the gradual removal of rhythm driver from SA node to AV one. ECG sings: violation of P wave configuration and lasting, dysrtythmia. Conduction violations Conduction violations include two groups of arrhythmias: heart block and preexcitation syndrome and has the results from abnormality impulse conduction. Causes of heart block are conductive ways damage (myocardial infarction, myocarditis, cardiosclerosis, heart failure, coronary heart disease, vagal tone). Conduction block can arise in the AV nodal fibers, in bungle of His, in the Purkinje conduction system, between SA node and atrium, inside atrium. 1. Sinoatrial block has such sings: impulses are not transmitted out the SA node, so on ECG waves P, QRS, and T are absent, pause is equal 2 (R-R). Some time occurs sinus arrest and on ECG no 3 or 4 (sequence) cardiac complex, it may result irregular pulse, prolonged period of asystole. Second-degree sinoatrial block 2. Atrial block ECG sings: P waves are deformed and their duration is more than 0.11 second. 3. Atrium-ventricular block has three degree. First-degree AV block is characterized only by the prolonged P-Q interval (< 0.2 second) in the result of retardation impulses conduction from atria to ventricles through AV node. Isolated first-degree AV block is never symptomatic. First-degree AV block Second-degree AV block is divided into two types. Type-first (Mobitz type I or Wenkebach phenomenon) is characterized by progressive lengthening of the PQ interval until an impulse is blocked, one cardiac cycle falls and then the cycle repeats again. After the fall of ventricle contraction Р-Q interval is restored, gradually becoming longer with each heart contraction. R-R are different, rhythm is irregular and there are more P waves than QRS complexes Type-first (Mobitz type I) Type II (Mobitz type II) is usually associated with organic cardiac disease. It is the intermittent block of atrial impulses conduction with a constant PR interval (normal or long), but QRS complexes fall more frequently, may be such correlations: 2:1; 3:1; 4:1. This type is complicated by cardiac output decrease. Type II (Mobitz type II) Third-degree AV block, or complete AV block, occurs when the conduction link between the atria and ventricles is lost. The atria continue to beat at a normal rate and the ventricles develop their own rate, which normally is slow (30-40/min, idioventricular rhythm). The atria and ventricles rates are regular but dissociated (on ECG P waves and QRS complexes occur independently, count of P waves more than QRG. It causes periods of syncope, known as a Stokes-Adams attack (sings: asystole more than 10-20 sec, a decrease of cardiac output, insensibility, convulsions, is possible death). Third-degree AV block 4. Ventricle block. Interruption of impulse conduction through the bundle branches is called bundle branch block. These blocks usually do not cause alterations in the rhythm of the heartbeat. Bundle branch block interrupts the normal progression of depolarization, causing the ventricles to depolarize one after the other because the impulses must travel through muscle tissue rather than through the specialized conductive tissue. It cause the QRS deformation, it is wide (normal is 0.08 to 0.12 second) and distorted. The left bundle branch bifurcates into left anterior and posterior fascicles. An interruption of one of these fascicles is referred to as a hemiblock. Their ECG sings are very difference, but the main sing is QRS complex deformation. The left bundle branch block Pre-excitation or Wolff-Parkinson-White (WPW) syndrome exists when atrial impulses are transmitted directly to the ventricles through shortcut conduction pathways. The impulses do not travel through the AV node but through accessory brunch (bungle of Kent). This connects the conduction system of the atria to either ventricle, bypassing the AV node. Impulses go down the accessory pathways and return by the normal conduction system to set up a re-entry system, it can cause supraventricular tachycardia. The ECG is characterized by a short P-R (less than 0.12 sec), a slurred upstoke on the QRS (delta wave), a wide QRS (more than 0.10 sec), secondary ST and T waves are changed (repolarization is altered). Another pre-excitation pattern is the Lown-Ganong-Levine syndrome, characterized by a short PR interval without a delta wave. These syndromes are dangerous because may cause electricity unstabilized myocardium, activation of ectopic driver and extrasistoles or paroxysmal ventricular tachycardia beginning. Arrhythmias in the result of combined heart properties violations Combined heart properties violations include disorders of automatism, conduction and irritability. Extrasystole is the extraordinary systole in the result of ectopic pacemaker activation. New pacemaker (out sinus node) causes beginning excitation wave, which spreads in altered direction. Dependency on cell localization, where the extraordinary impulse is formed, distinguishes such types of extrasystole: sinus, atrial, atria-ventricular and ventricular. Sinus extrasystole or premature atrial contraction is a beat initiated by an ectopic atrial focus that appears early in the cycle (before the next expected sinus beat). An excitation wave is usually conducted through the ventricular pathway in the normal manner not changes the shape of the QRS. A pause will follow the beat, and the SA node will start a new cycle. Atrial extrasystole is the result of ectopic pacemaker activation in different parts of atria. It is characterized by Р wave distortion (depressed, dysphasic, negative) because excitation wave goes retrograde, by partial compensatory pause. Sinus extrasystole Atrio-ventricular extrasystole is observed at beginning ectopic pacemaker in AV node (top and middle part). Excitation wave spreads in two directions: in ventricles — in normal, in atria – in retrograde. So, Р wave is negative and indicates or after normal QRS complex or can be coincide with QRS. Atrio-ventricular extrasystole Ventricular extrasystole or premature ventricular contraction (it is caused by a ventricular ectopic pacemaker) is more dangerous than sinus or atrial because violates the pumping action of the heart. After such extrasystole the ventricle usually is not able to repolarise sufficiently to respond to the next impulse that arises in the SA node (compensatory pause arises), diastolic volume is usually insufficient for ejection of blood. On the ECG: extrasystole complex is registered early in the cycle, is not usually preceded by P wave, QRS is distorted and wide, large looping ST segment opposite in direction to that of the QRS, full compensatory pause (interval between the R waves before and after the extrasystole complex is twice that of the normal R-R). Ventricular extrasystole Paroxysmal tachycardia. Extraordinary contractions can arise one by one or by groups. Paroxysmal tachycardia develops in case of numerous extrasystoles, with a rapid heart rate (in measure 140-250 beats per min, averaging about 170), which sudden onset and offset and couses physiological rhythm break. Duration of paroxysm can be different – from (some) seconds to (some) minutes, after that it similarly suddenly ends and adjusts normal rhythm. Atrial paroxysmal tachycardia is mostly observed. The patient frequently complains of a sudden pounding or fluttering in the chest associated with weakness or breathlessness. The fast rate stresses then heart and increases its need for oxygen. The tachycardia may also diminish cardiac output because of shortened ventricular filling tame. The heart is beating so rapidly that the ventricle doesn’t have time to fill completely, each beat pumps out less blood. If this tachycardia persists, the usual treatment is stimulation of the n.Vagus by carotid sinus or eyes massage, which slows the heart rate. Since this can produce dangerous slowing or cardiac arrest, the patient should be monitored. Atrial flutter is a rapid and regular atrial ectopic tachycardia, with a rate that ranges from 240 to 450 beats per minute. There two types of atrial flutter. Type I flutter is the result of re-entry mechanism in the right atrium and the rate frequency may be 240-350/min. The mechanism of type II is unknown. The atrial rate ranges between 350 and 450 beats in minute. On the ECG are defined regular and rapid F-waves (sawtooth pattern). Not all of the impulses are conduced, so the ventricular rate is usually slower. Because the impulses are coming so rapidly, the AV node cannot accept and conduct each one and ventricle response may be regular or irregular (some degree of block occurs at the node). Atrial fibrillation is the result of chaotic current flow within the atria. When the atrial cells cannot repolarize in time for the next incoming stimulus, the ectopic current is rejected by the refractory cells and sent in another direction. On ECG: atrial electrical activity is disorganized and indicated by f-waves with frequency 350-700/min. Conduction through the AV node is disorganized, so complexes QRS appear irregular; the peripheral pulse is grossly irregular, and a pulse deficit can be observed. Ventricle flutter (ventricular tachycardia) is the result of ventricle frequency excitement by permanently circulation impulses (re-entry mechanism). A rate usually is 150-200/min. On ECG: rate is fast, QRS is wide, and P waves may sometime be visible in the complex QRS. It is very dangerous arrhythmia because it leads to reduced cardiac output, and many times, to ventricular fibrillation. Ventricle flutter In ventricular fibrillation, the ventricle quivers but doesn’t contract, so there is no cardiac output, and there are no palpable or audible pulses. The classic ECG pattern of ventricular fibrillation is that of gross disorganization without identifiable waveforms or intervals (frequency 200-500/min). Ventricular fibrillation Preventing more serious arrhythmias often involves drug therapy, electrical stimulation, or surgical intervention. The correction of very dangerous arrhythmias can involve the use of an electronic pacemaker, cardioversion, or defibrillation. Electrical interventions can be used in emergency and elective situations. A pacemaker is an electronic device that delivers an electrical stimulus to the heart. It is used to initiate heartbeats in situations when the normal pacemaker of the heart is defective or in complete heart block in which the rate of cardiac contraction and consequent cardiac output is inadequate to perfuse vital tissue. Overdrive pacing is used to treat recurrent ventricular tachycardia, atrial flutter. A pacemaker may be used as a temporary or a permanent measure. Defibrillation and synchronized cardioversion are two reliable methods for treating ventricular tachycardia and fibrillation. The discharge of electrical energy that is synchronized with the R wave of the ECG is referred to as synchronized cardioversion, and unsynchronized discharge is known as defibrillation. The goal of both these techniques is to provide an electrical pulse to the heart in such a way as to completely depolarize the heart during passage of the current. This electrical current interrupts the disorganized impulses, allowing the SA node to regain control of the heart. Defibrillation depolarizes all of the myocardial cells simultaneously and allows the SA node to resume normal conduction.