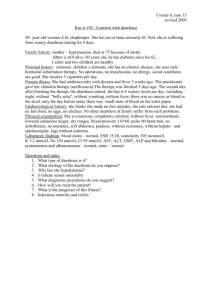
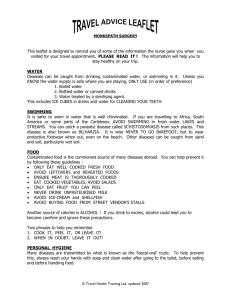
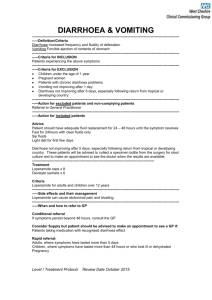
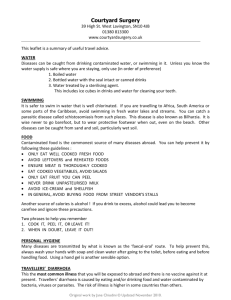
Travellers' Diarrhoea Travel health advice relating to travellers' diarrhoea Diarrhoea is the most common symptom experienced during travel.(1) Although overall the incidence of travellers' diarrhoea is declining, it still affects 10-40% of travellers to certain regions.(1)(2)(3) Travellers’ diarrhoea (TD) is more common in travellers who are:(4) immunocompromised have reduced gastric acid i.e. are on drugs reducing gastric acidity children < 6 years of age and younger adults travelling from developed to undeveloped countries undertaking extreme/adventure travel Aetiology TD can be caused by a wide variety of organisms, all of which are spread through the faecal/oral route.(5)(6)(7) Bacteria account for up to 80% of cases, most commonly Enterotoxigenic E.coli and Enteroaggregative. E.coli. o Other bacterial causes include Campylobacter jejuni, Shigella, Salmonella and occasionally Vibrio cholerae. Viruses such as rotavirus or norovirus cause 5-10% of cases. Parasites account for 2-10% of cases of acute TD, particularly Giardia intestinalis. o Other parasitic causes include Entamoeba histolytica, Cryptosporidia, Cyclospora. o Parasitic causes are usually associated with symptoms lasting >1 week. Infection with more than 1 pathogen is common. Underlying organisms may not be identified in 20-40% cases. Loose motions may also result from a change in diet including, for example, spicy or oily foods, excess alcohol and the stress associated with travel. Epidemiology Destination of travel is one of the most important determinants of travellers' diarrhoea: the world can be divided into the following categories based on the risk of diarrhoea.(1)(2) Low Risk Australia, Canada, Europe, Japan, New Zealand, USA Moderate Risk Caribbean, North East Asia, Oceania, Southern Europe, Russia High Risk Middle East, Parts of South America, most of Africa, Asia and Central America The aetiology of TD varies with travel to different world regions: E. coli is the most common cause of TD after travel to Latin America. Campylobacter is more common after travel to SE Asia.(7) Clinical Signs and Symptoms Travellers’ diarrhoea is defined as the passage of three or more loose or liquid stools in 24 hours, or sudden onset of abnormally loose/watery stool for the individual, accompanied by any of: fever abdominal cramps faecal urgency nausea or vomiting.(5)(8)(9) Most cases occur in the first week of travel.(2)(10) Its severity can be graded as:(9) Mild travellers’ diarrhoea Usually has no accompanying symptoms and does not disrupt normal activities. Most cases are mild and do not significantly alter travel activities. Moderate travellers’ diarrhoea Associated with additional symptoms, is distressing and leads to an interruption of normal activities. Severe travellers’ diarrhoea Associated with additional symptoms, is incapacitating and prevents all planned activities. Usually > 6 stools daily, ~ 3% have 10 or more stools daily. Infection with an invasive organism can result in dysentery, where frank blood and mucous occur in the stool: this is always considered severe and medical attention is required. On average, TD symptoms last for 3-5 days and the majority of cases self resolve without any specific treatment. Persistent diarrhoea is defined as symptoms lasting > 14 days.(9) Sequelae of travellers' diarrhoea are uncommon, but include:(2)(9)(10)(11) post-infectious irritable bowel syndrome Guillain-Barre syndrome reactive arthritis Prevention This depends mainly upon practising good hand hygiene and effective food and water precautions. Hands should always be washed thoroughly using soap and clean water (alcohol hand gel is an alternative when washing facilities are not available): before and after eating and drinking after using the toilet or changing nappies before handling food and particularly after touching raw meat after visiting food markets Travellers should be advised to avoid swimming in recreational water if they have diarrhoea.(12) Diarrhoea may occur even in travellers who stick strictly to food and water precautions; in many destinations the risk is determined by local food hygiene and sanitation practices.(3) In certain circumstances prophylactic medication or vaccination may be considered.(9) Treatment Most cases of TD are self-limiting and resolve within 3 to 5 days. Treatment involves consideration of: rehydration antidiarrhoeal agents antibiotics Rehydration The priority in treatment is preventing dehydration especially in young children. Clear fluids such as diluted fruit juices or ideally, specially prepared oral rehydrating solutions such as Dioralyte® or generic rehydration solutions (available over the counter at pharmacies) should be drunk liberally. All rehydrating drinks must be prepared with safe water. Anti-diarrhoeal Agents Mild/moderate diarrhoea Loperamide (Imodium®) is effective and can help particularly with associated colicky pains. Dose - 4mg orally, then 2mg after each loose stool (up to 16mg daily). Not recommended for use in children under 12 years of age.(13) The effect of loperamide is not instantaneous and may take 1 - 2 hrs to reach its maximal effect.(9) Over-use can cause rebound constipation. Moderate/Severe diarrhoea Loperamide can be used alone for moderate diarrhoea, and as an adjunct for moderate/severe diarrhoea alongside antibiotic therapy.(4) Anti-diarrhoeal agents should be avoided where there is blood/mucous in stool and/or high fever or severe abdominal pain, due to the risk of complications such as septicaemia. Antibiotics Antibiotics are only required in the treatment of severe diarrhoea. Antibiotics should improve diarrhoea within 1-2 days. Marked vomiting, fever, pain, bleeding or dehydration require hospital referral so that intravenous fluids can be administered. The decision on which antibiotic to prescribe should be based on the side effect profile of an antibiotic, potential drug interactions, contraindications and regional bacterial pathogen sensitivities, e.g.: Enterotoxigenic E.coli (ETEC) induced diarrhoea is common in South America and Africa and fluoroquinolone sensitive. Campylobacter associated diarrhoea is most common in South and South East Asia and frequently quinolone resistant.(7) Antibiotics for Empiric Treatment (for adults)(9) Azithromycin - 500-1000mg for 1 day or 500mg od for 3 days.(14) Preferred regime if signs of invasive diarrhoea (blood/mucous in stool) or febrile diarrhoea. Use first line for travel to South-east Asia/India or if fluoroquinolone resistant ETEC/Campylobacter. Rifaximin - 200mg tds for 3 days.(5)(15)(16) Avoid if symptoms of invasive diarrhoea (blood/mucous in stool). o Efficacy against invasive organisms is unconfirmed (Campylobacter, Salmonella, Shigella species). Ciprofloxacin – 750mg od for 1 day or 500mg bd for 1 day. If no improvement can be used for 3 days. Should not be used if symptoms of invasive diarrhoea (blood/mucous in stool) or travel to region with known fluoroquinolone resistance (Southeast Asia/India). Self-treatment Self-treatment can be carried by travellers and involves consideration of: rehydration anti-diarrhoeal agents antibiotics Antibiotic self-treatment is unnecessary for the majority of travellers and should NOT be recommended routinely. Self-treatment with antibiotics should only be used in severe diarrhoea. Travellers who may be suitable for self-treatment include those who: travel to remote rural areas with a high diarrhoea risk and are distant from medical help have pre-existing bowel problems such as inflammatory bowel disease where infection may trigger a relapse have pre-existing medical conditions which may be compromised by severe infection or dehydration e.g. poorly controlled diabetes, renal impairment etc Travellers prescribed antibiotics for self-treatment must be counselled appropriately on their use, and be aware that: The vast majority of cases of TD are mild and settle spontaneously or with simple measures. Widespread injudicious use of antibiotics for prophylaxis and treatment promotes drug resistance. o Colonization during travel with highly drug resistant colonic bacteria has been linked to antibiotic use (particularly fluoroquinolones) for travellers' diarrhoea, and can be transmitted to close household contacts. (9)(17)(18)(19) The risk of side effects from antibiotics is likely to be greater than the discomfort of travellers' diarrhoea. Viral and parasitic causes of diarrhoea are not affected by antibiotics. Medical help should be sought if despite antibiotics, symptoms persist without improvement after 72 hours. Note: Probiotics have been used both as treatment and prophylaxis for acute infectious diarrhoea in numerous studies. To date, results are conflicting and/or inconclusive and their use is thus not recommended.(9)(20)(21) Prophylaxis Prophylaxis to reduce the likelihood of diarrhoea includes consideration of: non-antibiotic agents antibiotics vaccination Non-antibiotic Agents Bismuth subsalicylate:(5)(9) An effective, non antibiotic approach to prevent travellers' diarrhoea with an overall efficacy of about 60%. Available in tablet (Pepto-bismol® tablets) or liquid formulation (Pepto-bismol® liquid or Boots Pepti-calm®). To prevent travellers diarrhoea : 2 tablets or 30 ml are taken 4 times daily (max of 16 tablets or 240ml) at meal times and on retiring Note: causes blackening of the stool and tongue should not be used for >3 weeks should be avoided in: o those on salicylate (aspirin) preparations, or warfarin, methotrexate, probenacid o those with hypersensitivity to salicylates o those with renal insufficiency o those with gout o pregnancy o children under 16 years of age may interfere with the absorption of doxycycline used for malaria prophylaxis Antibiotic Prophylaxis Antibiotic chemoprophylaxis should not be used routinely:(9) The vast majority of cases of TD are mild and settle spontaneously or with simple measures. Widespread injudicious use of antibiotics for prophylaxis and treatment promotes drug resistance. Colonization during travel with highly drug resistant colonic bacteria has been linked to antibiotic use for travellers diarrhoea.(16)(17) The risk of side effects from antibiotics is likely to be greater than the discomfort of travellers diarrhoea. Viral and parasitic causes of diarrhoea are not affected by antibiotics. Antibiotic chemoprophylaxis should be used for short periods only, up to 2 weeks.(4) It may be considered in travellers with pre-existing bowel problems such as colitis or inflammatory bowel syndrome where an attack of diarrhoea could seriously aggravate symptoms or cause relapse. Antibiotic Dose Used for Preventing TD Rifaximin 200mg bd or 600mg od.(5)(22) Rifaximin is the only drug currently recommended for prophylaxis due to widespread antibiotic resistance in enteric pathogens to ciprofloxacin.(10) It is non-absorbable and is well tolerated with few side effects.(23) Efficacy 48 - 72% in prevention of diarrhoea.(23) The use of antibiotics for prophylaxis is off license. Campylobacter species are resistant to rifaximin. Note: Vaccination No licensed vaccines are available in the UK against TD. Dukoral® (oral cholera vaccine) Not licensed in the UK for TD prevention. May give some protection, specifically due to heat labile toxin producing enterotoxigenic E.Coli (ETEC) (about 50% of ETEC strains). Widespread use of this vaccine is not advised for TD.(5) References Travellers' Diarrhoea References 1. Steffen R. Epidemiology of travellers’ diarrhea. J Travel Med. 2017 Apr 1;24(suppl_1):S2–S5. 2. Steffen R, Hill DR, DuPont HL. Traveler’s diarrhea: a clinical review. JAMA. 2015 Jan 6;313(1):71–80. 3. Lalani T, Maguire JD, Grant EM, Fraser J, Ganesan A, Johnson MD, et al. Epidemiology and self-treatment of travelers’ diarrhea in a large, prospective cohort of department of defense beneficiaries. J Travel Med. 2015 Jun;22(3):152–160. 4. Taylor DN, Hamer DH, Shlim DR. Medications for the prevention and treatment of travellers’ diarrhea. J Travel Med. 2017 Apr 1;24(suppl_1):S17–S22. 5. Hill DR, Beeching NJ. Travelers’ diarrhea. Curr Opin Infect Dis. 2010 Oct;23(5):481–487. 6. Lääveri T, Antikainen J, Pakkanen SH, Kirveskari J, Kantele A. Prospective study of pathogens in asymptomatic travellers and those with diarrhoea: aetiological agents revisited. Clin Microbiol Infect. 2016 Jun;22(6):535– 541. 7. Jiang ZD, DuPont HL. Etiology of travellers’ diarrhea. J Travel Med. 2017 Apr 1;24(suppl_1):S13–S16. 8. Zaidi D, Wine E. An update on travelers’ diarrhea. Curr Opin Gastroenterol. 2015 Jan;31(1):7–13. 9. Riddle MS, Connor BA, Beeching NJ, DuPont HL, Hamer DH, Kozarsky P, et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J Travel Med. 2017 Apr 1;24(suppl_1):S57– S74. 10. Kittitrakul C, Lawpoolsri S, Kusolsuk T, Olanwijitwong J, Tangkanakul W, Piyaphanee W. Traveler’s Diarrhea in Foreign Travelers in Southeast Asia: A Cross-Sectional Survey Study in Bangkok, Thailand. Am J Trop Med Hyg. 2015 Sep;93(3):485–490. 11. Schwille-Kiuntke J, Mazurak N, Enck P. Systematic review with metaanalysis: post-infectious irritable bowel syndrome after travellers’ diarrhoea. Aliment Pharmacol Ther. 2015 Jun;41(11):1029–1037. 12. CDC. Diarrhea and Swimming [Internet]. Healthy Swimming: Healthy Water. 2021 [cited 29 June 2021]. Available from: https://www.cdc.gov/healthywater/swimming/swimm ers/rwi/diarrheal-illness.html 13. National Institute for Health and Care Excellence (NICE). Diarrhoea prevention and advice for travellers [Internet]. CKS. 2019 [cited 29 May 2020]. Available from: https://cks.nice.org.uk/diarrhoea- prevention-and-advice-for-travellers#!scenario 14. Tribble DR, Sanders JW, Pang LW, Mason C, Pitarangsi C, Baqar S, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3day levofloxacin regimen. Clin Infect Dis. 2007 Feb 1;44(3):338–346. 15. Koo HL, DuPont HL. Rifaximin: a unique gastrointestinal-selective antibiotic for enteric diseases. Curr Opin Gastroenterol. 2010 Jan;26(1):17–25. 16. Layer P, Andresen V. Review article: rifaximin, a minimally absorbed oral antibacterial, for the treatment of travellers’ diarrhoea. Aliment Pharmacol Ther. 2010 Jun;31(11):1155–1164. 17. Arcilla MS, van Hattem JM, Haverkate MR, Bootsma MCJ, van Genderen PJJ, Goorhuis A, et al. Import and spread of extended-spectrum βlactamase-producing Enterobacteriaceae by international travellers (COMBAT study): a prospective, multicentre cohort study. Lancet Infect Dis. 2017 Jan;17(1):78–85. 18. Kantele A, Lääveri T, Mero S, Vilkman K, Pakkanen SH, Ollgren J, et al. Antimicrobials increase travelers’ risk of colonization by extendedspectrum betalactamase-producing Enterobacteriaceae. Clin Infect Dis. 2015 Mar 15;60(6):837–846. 19. Connor BA, Keystone JS. Editorial Commentary: Antibiotic Self-treatment of Travelers’ Diarrhea: Helpful or Harmful? Clin Infect Dis. 2015 Mar 15;60(6):847–848. 20. Xie C, Li J, Wang K, Li Q, Chen D. Probiotics for the prevention of antibiotic-associated diarrhoea in older patients: a systematic review. Travel Med Infect Dis. 2015 Apr;13(2):128–134. 21. McFarland LV, Goh S. Are probiotics and prebiotics effective in the prevention of travellers’ diarrhea: A systematic review and meta-analysis. Travel Med Infect Dis. 2019;27:11–19. 22. Martinez-Sandoval F, Ericsson CD, Jiang Z-D, Okhuysen PC, Romero JHMM, Hernandez N, et al. Prevention of travelers’ diarrhea with rifaximin in US travelers to Mexico. J Travel Med. 2010 Apr;17(2):111– 117. This page was last changed on 21 July 2021