Hypertensive Disorders in Pregnancy: Preeclampsia Overview
advertisement
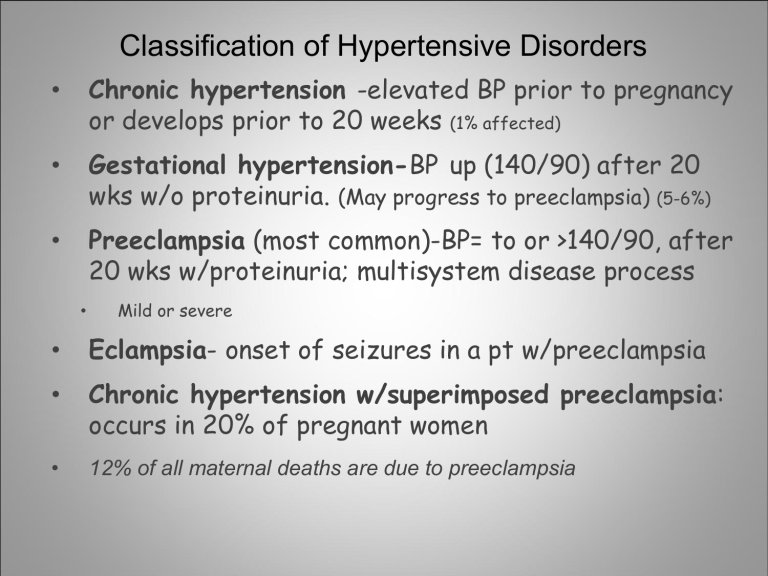
Classification of Hypertensive Disorders • Chronic hypertension -elevated BP prior to pregnancy or develops prior to 20 weeks (1% affected) • Gestational hypertension-BP up (140/90) after 20 wks w/o proteinuria. (May progress to preeclampsia) (5-6%) • Preeclampsia (most common)-BP= to or >140/90, after 20 wks w/proteinuria; multisystem disease process • Mild or severe • Eclampsia- onset of seizures in a pt w/preeclampsia • Chronic hypertension w/superimposed preeclampsia: occurs in 20% of pregnant women • 12% of all maternal deaths are due to preeclampsia Classic Signs of Preeclampsia 1. Hypertension – sustained BP of 140/90 2. Proteinuria -usually develops later than edema & increased BP; a. 300mg/dl or more of protein/24 hr period or b. 100mg/dl in 2 random samples 6 hrs apart 3. Generalized edema – due to fluid retention especially in hands & face 4. Other S/S- headache, drowsiness, mental confusion, visual changes, upset stomach, decrease in output, brisk DTRs Risk Factors: • First pregnancy, 1st pregnancy for FOB • Extreme ages: Age less than 17 years or > 35 yrs • Family history of PIH, FOB history of fathering • Obesity • Chronic renal disease, clotting disorders • Diabetes mellitus • Multiple gestation • Chronic hypertension or preexisting vascular disease • African-Americans Preeclampsia Pathophsiology • 1st stage-Widespread vasospasm & hypoperfusion to all organs including placenta. • 2nd stage-woman’s response to abnormal placentation (s/s appear HTN, proteinuria, & edema due to hypoperfusion) Pathophysiology (cont’d) • Decreased brain perfusion-small cerebral hemorrhages, & s/s of arterial vasospasm • Headaches • Visual disturbances • Blurred vision • Hyperactive DTRs Pathophysiology Decreased kidney perfusion- Body responds to hypovolemia by producing more angiotension II & aldosterone (retain both salt&water). Decreased urine output, Increased serum Na, BUN, uric acid, & creatinine. Edema Excessive wt gain (greater than 2 lbs/wk) Leads to pulmonary edema & generalized edema. Pathophysiology Decreased uterine/placental perfusion – may result in: • Fetal growth restriction (FGR) • Abruptio placenta • Higher risk for fetal death. Pathophysiology • Decreased liver perfusion- leads to impaired liver function, hepatic edema, & subcapsular hemorrhage. • Elevation of liver enzymes • Epigastric pain Edema • Treatment • Bed rest • Reducing environmental stimuli • Administering anticonvulsants Nursing Actions: • Pharmacotherapy • Magnesium sulfate IV infusion • Apresoline/Hydralazine IV Push • Continuous fetal monitoring • Bed rest; lateral position • Non-stimulating environment • Seizure precautions • Hourly intake & output, vital signs, DTR’s • Daily weights • Serum Magnesium levels DTRs Scale Assessing DTRs (patellar) Assessing DTRs The Patient With Preeclampsia • Nursing Diagnosis: Altered tissue perfusion • R/T increased peripheral vascular resistance • AEB: **urine output less than 500ml in 24 hrs **3+ pitting edema of feet **generalized edema of face and hands • Goal: Increased tissue perfusion over next 48 hrs • AEB: **urine output increased to > 750ml in 24 hrs **2+ pitting edema or less in feet **decreased generalized edema of face & hands The Patient With Preeclampsia • Nursing Actions: • Monitor 1.Edema in lower extremities & generalized edema of face/hands q 4 hrs. 2.Amount of protein in urine. Increased peripheral resistance causes reduced blood flow to kidneys. Results in glomerular damage- allows protein to leak across glomerular membrane. Loss of protein reduces colloid osmotic pressure & allows fluid to shift to interstitial spaces causing edema. 3. BP Q1H or as ordered by M.D. Vasospasm decrease diameter of blood vessels, which results in endothelial damage & decreased blood flow to all body organs. Decreased blood flow in renal system can cause damage to glomerular filtration system, causing a shift in fluid from intravascular space to interstitial space. The Patient With Preeclampsia **The patient’s urine output hourly. Reduced blood flow to kidney reduces the glomerular filtration, thereby reducing urine output. **Monitor lung sounds q 2 hrs. **Monitor for dyspnea Decreased colloid oncotic pressure can lead to pulmonary capillary leak that results in pulmonary edema. Manage: **Administer Mag S04 – usually 2 gms/hr IV. Mag S04 used to control seizures that result from inadequate blood flow to brain & hyper-irritability caused from reduced flow. Mag S04 relaxes smooth muscle & reduces vasoconstriction. Increases circulation to vital organs; increased circulation to kidneys leads to diuresis, as interstitial fluid is shifted to vascular space & excreted. The Patient With Preeclampsia **Place foley catheter for urine output measurement. Most accurate way to assess it. **Monitor amount of fluids patient receiving hourly. Usually patient on fluid restriction – 100ml/hr. Pulmonary edema can result from Preeclampsia. Evaluation: The goal of increased tissue perfusion was met in 48 hours AEB: **Urine output has increased to 1000ml in 24 hr period. **Pitting edema decreased from 3+ to 2+ in lower extremities. **No generalized edema of face & only a sm amt in hands. Chronic Hypertension • Women with chronic hypertension are at increased risk for preeclampsia. • Should be monitored closely for proteinuria & edema. • Antihypertensive medication should be initiated if blood pressure is higher than 160/110 mg Hg. • No more treratment of 140/90 due to masking of S/S. • Aldomet (drug of choice)-promotes circulation toElsevier placenta items and derived items © 2013, 2009, 2005 by Saunders, an imprint of 20 Elsevier Inc. Hemolysis, Elevated Liver Enzymes, & Low Platelets (HELLP) • Hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome • Hemolysis occurs as result of fragmentation & distortion of erythrocytes during passage through damaged blood vessels. • Liver enzyme levels increase when hepatic blood flow is obstructed by fibrin deposits. • Low platelet levels are caused by vascular damage resulting from vasospasm. Elsevier items and derived items © 2013, 2009, 2005 by Saunders, an imprint of Elsevier Inc. 21 Safe Antihypertensive Meds • Apresoline (Hydralazine) for BP of >160/110 • Aldomet (drug of choice) for chronic HTN • Nifedipine (Procardia) or Labetatol