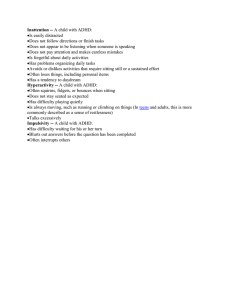
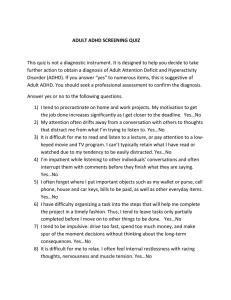
Introduction ADHD is a neurodevelopmental disorder, that can cause higher than normal levels of hyperactivity and impulsivity and may present itself as extreme difficulty in sitting still for long period of time or trouble focusing attention on a single task. The first recorded mention of ADHD dates to 1902, where a pediatrician described children who could not control their behavior like typical children. Whilst ADHD is commonly seen in children, the worldwide prevalence of adults with ADHD is estimated to be about 2.5% roughly translated to 200 million worldwide, with a dominance leaning towards men who are three times frequently diagnosed than females. Current view of ADHD In 2000, with the publication of the latest edition of the DSM (DSM-IV-TR), the best description of ADHD as it is still known today was born with the distinction made between Attention Deficit/Hyperactivity Disorder Combined type , ADHD predominantly Inattentive Type, ADHD Predominantly Hyperactive-Impulsive Type and ADHD Not other specified (American Psychiatric Association diagnostic and statistic manual, 2000) ADHD DSM-V CRITERIA A. Either 1 or 2 or 3 1) Six (or more) of the following symptoms on inattention have persisted for at least 6 months to a degree that is maladaptive and inconsistent with developmental level: Inattention a) Often fails to give attention to details or makes careless mistakes in schoolwork, work, or other activities b) Often has difficulty sustaining attention in tasks or play activities c) Often does not seem to listen when spoken to directly d) Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions) e) Often had difficulty organizing tasks and activities f) Often avoids, dislikes or is reluctant to engage in tasks that require sustained mental effort (such as schoolwork or homework) I g) Often loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, books, or tools)0 h) Is often easily distracted extraneous stimuli i) Is often forgetful in daily activities 2) Six (or more) of the following symptoms of hyperactivity impulsivity have persisted for at least 6 months to a degree that is maladaptive and with developmental level: a) Hyperactivity a) Often fidgets with hands or feet b) Often leaves seat in classroom or in other situations in which remaining seated expected c) Often runs about or climbs excessively in situations in which it is inappropriate (in adolescents or adults, may be limited to subjective feelings of restlessness) d) Often has difficulty playing or engaging in leisure activities quietly e) Is often “on the go” or often acts as if “driven by a motor” f) Often talks excessively b) Impulsivity a) Often blurts out answers before questions have been completed b) Often has difficulty awaiting turn c) Often interrupts or intrudes on other (e.g., butts into conversations or games) 3) Combined – child exhibits six or more symptoms of inattention, hyperactivity and impulsivity for greater than six months B. Some hyperactive -impulsive or inattentive symptoms that caused impairments were present before 7 years of age. C. Some impairment from the symptoms is present in 2 or more settings ( e.g., at school or work or at home) D. There mut be clear evidence of clinically significant impairment in social, academic, or occupational functioning. E. The symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorder and are not better accounted for by another mental disorder (e.g., mood disorder anxiety disorder, dissociative disorder, or personality disorder Criticisms of the DSM-IV-TR Diagnostic criteria Clinicians and researchers have pointed out numerous problems with the DSM-IV-TR criteria for ADHD: 1. The diagnostic criteria for children do not necessarily apply very well to adults with less than symptoms can be clearly impaired, even though they do not exhibit the minimum number (6) of symptoms required for a diagnosis (McGough & McCracken, 2006). 2. According to the criteria, if symptoms do not arise until after age 7, the diagnosis ADHD is not, strictly speaking, applicable (American Psychiatric Association, 2000). However, research studies that examined people whose symptoms arose after age 7 (generally by age 12) found that the symptoms were virtually identical to those of people with an earlier onset of the disorder, which suggests that the cutoff is not meaningful (Ferrone et al., 2006; McGough & Barkley, 2004) 3. Third, symptoms of hyperactivity may be different in females that in males: Girls who have hyperactive symptoms may talk more than other girls or may be more emotionally reactive, rather than hyperactive with their bodies (QUINN ,2005). Some researchers propose that ADHD is underdiagnosed in girls, who are less likely to have behavioral problems at school and are less likely to be referred for evaluation (Quinn, 2005). Before diagnosing ADHD, however , a mental health clinician should be sure that any difficulties in finishing tasks are a result of attentional problems, and not an oppositional attitude or difficulty in understanding the instructions. Example a child could have simply not have been paying attention when she or he was instructed to set up that dinner table or reminded of chores. And lastly when diagnosing adults with ADHD, clinicians should seek collaboration from school records or family members. Comorbid Disorders In addition to the primary symptoms of ADHD, children with this disorder often show other adjustment problems. One such problem is school performance: ADHD children are at risk grade retention, being placed in special education classes, and dropping of school (Barkley,1981; Semrud-Clikeman et al., 1991; Weiss & Hechtman, 1993). And third half of children with ADHD meet criteria for learning disability. There is no conclusive evidence that any of the subtypes of ADHD are more strongly associated with learning disabilities. Also, it is not clear what accounts for this correlation between academic difficulties and ADHD. It may be that the symptoms of ADHD impair children’s abilities to learn up to their potentials. Children with ADHD are likely to have peer difficulties; children with ADHD combined type are likely to be unpopular or rejected by peers , and those with ADHD primarily inattention type are more likely to be shy and withdrawn (Cantwell & Baker, 1992; Carlson, Lahey , & Neper, 1986; Lahey et al.,1984,1987). Children with ADHD have high rates of emotional disorders. Many have comorbid anxiety disorder, and other have comorbid depressive disorder. And children with primarily inattention type are more likely to exhibit depression and anxiety than those with combined Type. The most significant correlate of ADHD and conduct problems/Aggression; estimates of children that have a co-diagnosis of ADHD and conduct disorder range from 30-90%. Etiology ADHD is a disorder with multiple etiologies. Combinations of genetics, neurological, and environmental factors contribute to pathogenesis and phenotypes. Evidence from family, twin, and adoption studies have suggested strongly that ADHD is a highly hereditary polygenic disorder. Gene variants predicting risk for ADHD are important for brain development, cell migration, and encoding for catecholamine receptor and transporter genes. The identification of gene sets affecting neurotransmitter pathways in the brain has suggested that rare copy number variants or the accumulation of larger deletions and duplications influencing gene transcription are more commonly found in individuals with ADHD. Non-inherited neurological factors affecting brain development or resulting in brain injury have been implicated in ADHD pathogenesis. The contribution of pregnancy and birth complications is mixed, but strong evidence supports greater ADHD risk following in utero exposure to alcohol or tobacco and low birth weight. Hypoxic-anoxic brain injury, epilepsy disorders, and traumatic brain injury also contribute to ADHD risk. Exposure to environmental toxins (specially lead, organophosphate pesticides, and polychlorinated biphenyls) has been linked to ADHD symptoms. Except for children experiencing exceptional early deprivation, a causal relationship between family environment and psychosocial adversity and ADHD is unclear. Neuroimaging studies point to ADHD as a disorder of early brain development. Based on volumetric and functional MRI studies, differences are found in the structural development and functional activation in the prefrontal cortex, basal ganglia, anterior cingulate, and cerebellum. Activity among these areas depends on the catecholaminergic brain circuitry. Despite weak evidence for deficits in these neurotransmitters, their role is sustained by their distributions in those areas of the brain involved in ADHD and positive response of ADHD patients to medications that modulate the neurotransmission of catecholamines. A delay in cortical maturation has been documented, with peak cortical thickness attained n the cerebrum at 7 years in typically developing children and at 10 years in those with ADHD. ADHD Treatment Children ages 4-6 years .The first line of treatment should include Parenting training in behavior management Behavior therapy is an effective treatment for ADHD that can improve a child’s behavior ,self-control and self-esteem. It is most effective in young children when it is relieved by parents. When parents become trained in behavior therapy , they learn skills and strategies to help their child with ADHD succeed at school, at home and in relationships. Therapists should teach parents skills and strategies that use positive reinforcement , structure ,and consistent discipline to manage their child’s behavior. Therapists should teach parents positive way to interact and co0mmuinicate with their child. They should assign activities for parents to practice with their child. Classroom Treatment strategies for ADHD There are some school based management strategies shown to be effective for ADHD students: Behavioral classroom management and organizational training. The behavioral classroom management approach encourages a student’s positive behaviors in the classroom, through a reward systems or daily report card, and discourages their negative behaviors. This teacher led approach has been shown to influence student behavioral a constructive manner, increasing academic engagement. Although tested mostly in elementary school’s behavioral classroom management has been shown to work in students of all ages. Organizational training teaches children time management, planning skills, and ways to keep school materials organized in order to optimize student learning and reduce distractions. This management strategy has been tested with children and adolescents.