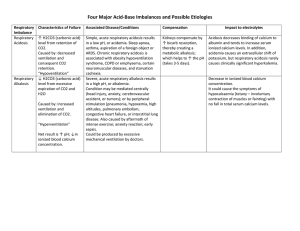
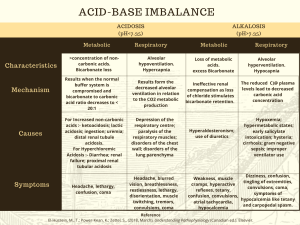
causes of respiratory acidosis respiratory depression from anesthesia, overdose, increased intracranial pressure, airway obstruction from decreased alveolar capillary diffusion like pneumonia, COPD, ARDS, AND PE signs/symptoms of respiratory acidosis hypoventilation (hypoxia), rapid, shallow respirations, decrease in BP, skin/mucous pale to cyanotic, headache, hyperkalemia, dysrhythmias, drowsiness, dizziness, disorientation, muscle weakness, hyperreflexia Nursing management of respiratory acidosis: ventilator, arterial blood gas, low-dose oxygen in chronic conditions, high-dose oxygen in acute hypoxia with acidosis, I/O, promote the release of CO2, turn/cough/deep breathe, assume semi-high fowlers position, clear respiratory secretions, colors of skin, mucous membranes causes of respiratory alkalosis: high pH, low co2 and hyperventilation, initial stages of pulmonary emboli, hypoxia, fever, pregnancy, high altitudes, and anxiety signs/symptoms of respiratory alkalosis: seizures, deep/rapid breathing, hyperventilation, tachycardia, decrease BP, hypokalemia, numbness/tingling in extremities, lethargy/confusion, light headedness, N/V nursing management of respiratory alkalosis: mask or paper bag, sedatives, monitor respiratory rate/depth, tachycardia, low BP, serum K+ levels/ECG levels, hydration status I/O, check for toxicities metabolic acidosis low ph, normal co2 and low bicarbonate metabolic acidosis signs/symptoms: compensatory hyperventilation (kussmaul respirations), headache, decreased BP, hyperkalemia, muscle twitching, warm/flushed skin, N/D/V, changes in LOC, metabolic acidosis signs/symptoms compensatory hyperventilation (kussmaul respirations), headache, decreased BP, hyperkalemia, muscle twitching, warm/flushed skin, N/D/V, changes in LOC, causes of metabolic acidosis: low ph/low bicarbonate, diabetic ketoacidosis, shock, sepsis, severe diarrhea, and renal failure what goes up in acidosis: potassium metabolic acidosis nursing management: BUN, creatinine, hemoglobin/hematocrit levels, monitor hydration, turn/cough/deep breathe, ABG's, check K, Ca usually goes down, weights, vitals causes of metabolic alkalosis: high ph, high bicarb and severe vomiting, excessive GI suctioning, diuretics, and excessive NaHCO3 metabolic alkalosis signs/symptoms: restlessness (lethargy), confusion, dizzy, irritable, dysrhythmias, compensatory hypoventilation, N/V/D, tremors, muscle cramps, tingling of fingers and toes, dehydration metabolic alkalosis nursing management: monitor ECG's, ABG's for pH, K, Ca levels, LOC checks for tetany, tremors, muscle cramps, tingling, what is hyperkalemia frequently associated with: metabolic acidosis what is hyperkalemia frequently associated with metabolic acidosis what is a compensatory mechanism for metabolic alkalosis: decreased respiratory rate and depth to retain CO2 and kidney excretion of bicarbonate decreased output causes: renal failure fluid volume excess causes: heart failure, water intoxication, liver cirrhosis, SIADH, lung cancer, renal failure, primary polydipsia, long term use of cortiosteroids fluid volume excess clinical manifestations: headache, JVD, increased weight, edema, ascites, elevated blood pressure, crackles in lungs, confusion, decreased urine specific gravity, pitting edema, high BP, presence of s3, tachycardia, bounding pulse, changes in LOC, seizures, low pulse ox (below 89%), seizures, coma, muscle spasms, dyspnea fluid volume excess nursing management: fluid volume excess clinical manifestations headache, JVD, increased weight, edema, ascites, elevated blood pressure, crackles in lungs, confusion, decreased urine specific gravity, pitting edema, high BP, presence of s3, tachycardia, bounding pulse, changes in LOC, seizures, low pulse ox (below 89%), seizures, coma, muscle spasms, dyspnea fluid volume excess nursing management: frequent respiratory assessments and LOC, watch for edema, cardiovascular checks, daily weights, fluid restriction, measure intake and output, decrease sodium intake, diuretics fluid volume deficit signs/symptoms: restlessness, drowsiness, lethargy, confusion, thirst, dry mucous membranes, decreased skin turgor, decreased cap refill, postural hypotension, increased pulse 120, decreased CVP, decreased urine output, concentrated urine, increased respiratory rate, weakness, dizziness, seizures, coma, decreased BP 86/50 hypernatremia; fluid volume deficit signs/symptoms: signs of thirst, fever, dry mucous membranes, hypotension, tachycardia, low jugular venous pressure and restlessness, weakness, change of LOC, thready pulses nursing management of hypernatremia: administer hypotonic solution if na known, administer isotonic solution if na is not known, if corrected too quickly can cause cerebral edema hypernatremia nursing interventions: treat the cause, add water to balance sodium, or replace sodium and water, monitor I/O, urine specific gravity greater than 1.025, pulses, tachycardia, tachypnea, changes in sensorium, daily weights, skin turgor and mucous membranes hyponatremia causes: sodium is less than 135 mEq/L, vomiting, diuretics, gastrointestinal suctioning, diarrhea, inadequate salt intake, fluid shift from the ICF to the ECF by hypertonic solutions which leads to dilutional hyponatremia hyponatremia signs and symptoms: cell swells, lethargy, headache, confusion, apprehension, seizures, and coma, change in LOC, muscle weakness, stupor, tendon reflexes decreases hyponatremia interventions: administer hypertonic solutions with known Na value, monitor patients lungs sounds, administer isotonic solutions with unknown sodium level, report LOC changes, fluid restriction if caused by too much water nursing management of hyponatremia: I/O, check for bounding pulses, bulging neck veins, BP changes, signs of cerebral edema, daily weights, pitting edema with fluid excess, daily weights and goal is to restore na and water balance and prevent complications of cerebral edema hyperkalemia caused by life threatening, impaired renal excretion of potassium, excess intake, metabolic acidosis and medications like beta blockers, dehydration hyperkalemia signs/symptoms (MURDER) muscle cramps, urine abnormalities, respiratory distress, decreased cardiac contractility, EKG changes, and reflexes nursing management of hyperkalemia check for muscle weakness, administer diuretics, monitor renal and respiratory status, restricted diet, increase fluid intake, administer insulin-kayexalate, dialysis, monitor ECG, monitor blood sugar hypokalemia is caused by increased excretion of potassium, N/V, sweating, diuretics, dialysis, increased insulin, alkalosis, tissue repair, increased epinephrine, lack of intake hypokalemia assessment muscle weakness and cramps, life threatening if not treated, alkalosis on ABG, fatigue, depressed ST with a U wave, arrhythmias, thready pulse signs/symptoms of hypokalemia (A SIC WALT) alkalosis, shallow respirations, irritability, confusion and drownsiness, weakness and fatigue, arrhythmias, lethargy, thready pulse hypokalemia nursing interventions watch for skeletal muscle weakness, most dangerous drug to administer, on IV pump no more than 10 mEq/hr, causes vein irritation, ice site, lidocaine, monitor, piggyback with normal saline, always on a pump, encourage intake from foods