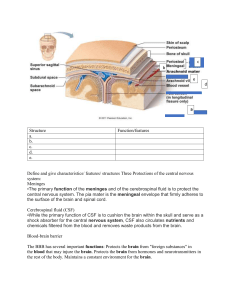
Nursing Assessment of Patients with Neurological Disorders 56 Nursing Assessment Nervous System LEARNING OUTCOMES 1. Differentiate between the functions of neurons and glial cells. 2. Explain the anatomic location and functions of the cerebrum, brainstem, cerebellum, spinal cord, peripheral nerves, and cerebrospinal fluid. 3. Identify the major arteries supplying the brain. 4. Describe the functions of the 12 cranial nerves. 5. Compare the functions of the two divisions of the autonomic nervous system. 6. Link the age-related changes in the neurologic system to the differences in assessment findings. 7. Select significant subjective and objective data related to the nervous system that should be obtained from a patient. 8. Select appropriate techniques to use in the physical assessment of the nervous system. 9. Differentiate normal from abnormal findings of a physical assessment of the nervous system. 10. Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the nervous system. STRUCTURES AND FUNCTIONS OF NERVOUS SYSTEM Human nervous system is responsible for the control & integration of the body’s many activities. The nervous system is divided into the central nervous system and peripheral nervous system. The central nervous system (CNS) consists of brain, spinal cord, & cranial nerves I & II. The peripheral nervous system (PNS) consists of cranial nerves III to XII, spinal nerves, and the peripheral components of the autonomic nervous system (ANS). Cells of Nervous System The nervous system is made up of two types of cells: neurons and glial cells. Neurons Neurons are the primary functional unit of the nervous system; they have many shapes & sizes. Characteristics neurons: 1) Excitability, or the ability to generate a nerve impulse; 2) Conductivity, or the ability to transmit an impulse; and 3) Influence other neurons, muscle cells or glandular cells by transmitting nerve impulses to them. A typical neuron consists of a cell body, multiple dendrites, and an axon (Fig. 1). The cell body is the metabolic center of the neuron. Dendrites extending from cell body that receive impulses from the axons of other neurons and conduct impulses toward the cell body. The axon (cm - > meter). The axon carries nerve impulses to other neurons or to end organs. Many axons in the CNS and PNS are covered by a myelin sheath, (white, lipid substance that acts as an insulator for the conduction of impulses). Axons may be myelinated (long fibers) or unmyelinated (smaller fibers). Neurons are nonmitotic, if damaged, neurons could not be replaced. The discovery of neuronal stem cells now demonstrates that neurogenesis occurs in adult brains after cerebral injury. 1 FIG. 1 Structural features of neurons: dendrites, cell body, and axons. Glial Cells Glial cells (glia or neuroglia) provide support, nourishment & protection to neurons. Glial cells constitute half of the brain & spinal cord mass and are 5-10 times more numerous than neurons. Glial cells are divided into microglia and macroglia. Microglia → macrophages → (phagocytosis) protect neurons, move within brain and multiply when brain is damaged. Macroglial cells include → Astrocytes, Oligodendrocytes & Ependymal cells. Astrocytes are found primarily in gray matter, they performed the following action. Provide structural support to neurons. Play a role in synaptic transmission (conduction of impulses between neurons). Phagocytes for neuronal debris when the brain is injured. They help restore neurochemical milieu Provide support for repair. Proliferation of astrocytes contributes to the formation of scar tissue (gliosis) in the CNS. Oligodendrocytes are specialized cells that produce the myelin sheath of nerve fibers in the CNS and are primarily found in the white matter of the CNS. Ependymal cells line the brain ventricles and aid in the secretion of cerebrospinal fluid (CSF). Neuroglia are mitotic & can replicate. In general, when neurons are destroyed, the tissue is replaced by the proliferation of neuroglial cells. Nerve Regeneration Damaged nerve cells attempt to grow back by sprouting many branches from damaged ends of their axons. Axons in CNS are less successful than peripheral axons in regeneration. Injured nerve fibers in PNS can regenerate by growing within the protective myelin sheath of the supporting Schwann cells if cell body is intact. Nerve Impulse The neuron initiate, receive & process messages about events both within & outside the body. Once an action potential is initiated, a series of action potentials travels along axon. When the impulse reaches the end of the nerve fiber, it is transmitted across the junction between nerve cells (synapse) by a chemical interaction involving neurotransmitters. 2 This chemical interaction generates another set of action potentials in the next neuron. These events are repeated until the nerve impulse reaches its destination. Because of its insulating capacity, myelination of nerve axons facilitates the conduction of an action potential. Many peripheral nerve axons have nodes of Ranvier (gaps in the myelin sheath) that allow an action potential to travel much faster by jumping from node to node without traversing the insulated membrane segment. This is called salutatory (hopping) conduction. In an unmyelinated fiber, the wave of depolarization travels the entire length of the axon, with each portion of the membrane becoming depolarized in turn. Synapse. A synapseis the structural and functional junction between two neurons. It is the point at which the nerve impulse is transmitted from one neuron to another. The nerve impulse can also be transmitted from neurons to glands or muscles. The essential structures of synaptic ransmission are a presynaptic terminal, a synaptic cleft, and a receptor site on the postsynaptic cell. Neurotransmitters Neurotransmitters are chemicals that affect the transmission of impulses across the synaptic cleft. Excitatory neurotransmitters (e.g., epinephrine, norepinephrine, glutamate) activate postsynaptic receptors that increase the chance that an action potential will be generated. Inhibitory neurotransmitters (e.g., serotonin, γ-aminobutyric acid [GABA], dopamine) activate postsynaptic receptors to decrease the chance that an action potential will be generated. For example, endorphins block pain transmission while substance P makes nerves more sensitive to pain. TABLE -1 NEUROTRANSMITTERS Neurotransmitter Acetylcholine Amines Epinephrine (adrenalin) Norepinephrine Serotonin Dopamine Amino Acids γ-Aminobutyric acid (GABA) Glutamate and aspartate Clinical Relevance A decrease in acetylcholine-secreting neurons Is seen in Alzheimer’s disease. Myasthenia gravis results from a reduction in acetylcholine receptors. Is both a hormone and neurotransmitter. Produced in neurons of CNS and neurosecretory cells of adrenal medulla. Critical component of the fight-or-flight response of SNS. Is both a hormone and neurotransmitter. Has important role as neurotransmitter released from SNS affecting the heart. Along with epinephrine, has important role in fight-or-flight response, increasing heart rate, triggering the release of glucose from energy stores, and increasing blood flow to skeletal muscle. Primarily found in GI tract, platelets, and CNS. Involved in moods, emotions, and sleep. Produced in several areas of brain. Involved in emotions and moods and regulating motor control. Parkinson’s disease results from destruction of dopamine-secreting neurons. Chief inhibitory neurotransmitter in CNS. Has a role in regulating neuronal excitability throughout the nervous system. Drugs that increase GABA function have been used to treat seizure disorders. Plays key role in learning and memory. Sustained release of glutamate and prolonged excitation is toxic to nerve cells. Glutamate is a destructive factor in amyotrophic lateral sclerosis. Neuropeptides Endorphins Endogenous opioids that function as neurotransmitters. Produced in pituitary and enkephalins gland and hypothalamus. Produce analgesia and a feeling of well-being. The opioids morphine and heroin bind to endorphin and enkephalin receptors 3 Substance P and produce the same effect as the endogenous opioids. Neurotransmitter in pain transmission pathways. Morphine blocks its release. Central Nervous System Components of the CNS include cerebrum (cerebral hemispheres), brainstem, cerebellum & spinal cord. Spinal Cord The spinal cord is continuous with the brainstem and exits from the cranial cavity through the foramen magnum. A cross section of the spinal cord reveals gray matter that is centrally located in an H shape and is surrounded by white matter. The gray matter contains the cell bodies of voluntary motor neurons, preganglionic autonomic motor neurons, and association neurons (interneurons). The white matter contains the axons of the ascending sensory and the descending (suprasegmental) motor fibers. The spinal pathways or tracts are named for the point of origin and the point of destination (e.g., spinocerebellar tract [ascending], corticospinal tract [descending]). Ascending Tracts In general, the ascending tracts carry specific sensory information to higher levels of the CNS. This information comes from special sensory receptors in the skin, muscles and joints, viscera, and blood vessels and enters the spinal cord by way of the dorsal roots of the spinal nerves. The fasciculus gracilis and fasciculus cuneatus (commonly called dorsal or posterior columns) carry information and transmit impulses concerned with touch, deep pressure, vibration, position sense, and kinesthesia (appreciation of movement, weight, and body parts). The spinocerebellar tracts carry information about muscle tension and body position to cerebellum for coordination of movement. The spinothalamic tracts carry pain and temperature sensations. Descending Tracts Descending tracts carry impulses that are responsible for muscle movement. Among the most important descending tracts are the corticobulbar & corticospinal tracts, collectively termed the pyramidal tract, these tracts carry volitional (voluntary) impulses from cerebral cortex to cranial & peripheral nerves. Another group of descending motor tracts carries impulses from the extrapyramidal system (all motor systems except the pyramidal) concerned with voluntary movement. It includes pathways originating in the brainstem, basal ganglia, and cerebellum. Lower and Upper Motor Neurons Lower motor neurons (LMNs) are the final common pathway through which descending motor tracts influence skeletal muscle. The cell bodies of LMNs, which send axons to innervate the skeletal muscles of the arms, trunk, and legs, are located in the anterior horn of the corresponding segments of the spinal cord (e.g., cervical segments contain LMNs for the arms). LMNs for skeletal muscles of the eyes, face, mouth, and throat are located in the corresponding segments of the brainstem. These cell bodies and their axons make up the somatic motor components of the cranial nerves. LMN lesions generally cause weakness or paralysis, denervation atrophy, hyporeflexia or areflexia, and decreased muscle tone (flaccidity). Upper motor neurons (UMNs) Originate in the cerebral cortex and project downward. The corticobulbar tract ends in the brainstem, and the corticospinal tract descends into the spinal cord. These neurons influence skeletal muscle movement. UMN lesions generally cause weakness or paralysis, disuse atrophy, hyperreflexia, and increased muscle tone (spasticity). 4 Reflex Arc A reflex is an involuntary response to stimuli. In the spinal cord, reflex arcs play an important role in maintaining muscle tone, which is essential for body posture. The components of a monosynaptic reflex arc (Fig. 2) are a receptor organ, an afferent neuron, an effector neuron, and an effector organ (e.g., skeletal muscle). The afferent neuron synapses with the efferent neuron in the gray matter of the spinal cord. More complex reflex arcs have other neurons (interneurons) in addition to the afferent neuron influencing the effector neuron. FIG.-2 Basic diagram of the patellar “knee jerk” reflex arc, including the (1) sensory stretch receptor, (2) afferent sensory neuron, (3) interneuron, (4)efferent motor neuron, and (5) quadriceps muscle (effector organ) Brain The term brain usually refers to the three major intracranial components: cerebrum, brainstem, and cerebellum. FIG -3 Left hemisphere of cerebrum, lateral surface, showing major lobes and areas of the brain. Cerebrum The cerebrum is composed of the right & left cerebral hemispheres and divided into four lobes: frontal, temporal, parietal, and occipital (Fig.3). The functions of the cerebrum are multiple and complex (Table -2). The frontal lobe controls higher cognitive function, memory retention, voluntary eye movements, voluntary motor movement, and speech in Broca's area. The temporal lobe integrates somatic, visual, and auditory data & contains Wernicke’s speech area. The parietal lobe interprets spatial information and contains the sensory cortex. Processing of sight takes place in the occipital lobe. The division of the cerebrum into lobes is useful to delineate portions of the neocortex (gray matter), which makes up the outer layer of the cerebral hemispheres. Neurons in specific parts of the neocortex are essential for various highly complex and sophisticated aspects of mental function, such as language, memory, and appreciation of visual-spatial relationships. The basal ganglia, thalamus, hypothalamus, and limbic system are also located in the cerebrum. 5 The basal ganglia are a group of structures located centrally in the cerebrum and midbrain. Most of them are on both sides of the thalamus. The function of the basal ganglia includes the initiation, execution, and completion of voluntary movements, learning, emotional response, and automatic movements associated with skeletal muscle activity (e.g., swinging the arms while walking, swallowing saliva, and blinking). The thalamus (part of the diencephalon) lies directly above the brainstem (Fig.-4) and is the major relay center for afferent inputs to the cerebral cortex. The hypothalamus is located just inferior to the thalamus and slightly in front of the midbrain. It regulates the ANS and the endocrine system. The limbic system is located near the inner surfaces of the cerebral hemispheres and is concerned with emotion, aggression, feeding behavior, and sexual response. Brainstem The brainstem includes the midbrain, pons, and medulla (Fig. -4). Ascending and descending fibers to and from the cerebrum and cerebellum pass through the brainstem. The nuclei of cranial nerves III through XII are in the brainstem. Vital centers concerned with respiratory, vasomotor & cardiac function are located in medulla. Also located in the brainstem is the reticular formation, a diffusely arranged group of neurons and their axons that extend from the medulla to the thalamus and hypothalamus. The functions of the reticular formation include relaying sensory information, influencing excitatory and inhibitory control of spinal motor neurons, and controlling vasomotor and respiratory activity. The reticular activating system (RAS) is a complex system that requires communication among the brainstem, reticular formation, and cerebral cortex. The RAS is responsible for regulating arousal and sleep-wake transitions. The brainstem also contains the centers for sneezing, coughing, hiccupping, vomiting, sucking, and swallowing. (Fig.4) Major divisions of the central nervous system (CNS). Cerebellum The cerebellum is located in the posterior part of the cranial fossa inferior to the occipital lobe. The cerebellum coordinates voluntary movement and maintains trunk stability and equilibrium. The cerebellum receives information from the cerebral cortex, muscles, joints, and inner ear. It influences motor activity through axonal connections to the motor cortex, the brainstem nuclei, and their descending pathways. 6 TABLE 2 FUNCTION OF CEREBRUM Part Cortical Areas Motor Primary Supplemental Sensory Somatic Visual Auditory Association areas Location Precentral gyrus Anterior to precentral gyrus Postcentral gyrus Occipital lobe Superior temporal gyrus Parietal lobe Function Motor control and movement on opposite side of body Facilitates proximal muscle activity, including activity for stance and gait, and spontaneous movement and coordination Posterior temporal lobe Anterior temporal lobe Anterior frontal lobe Sensory response from opposite side of body Registers visual images Registers auditory input Integrates somatic and sensory input Integrates visual and auditory Input for language comprehension Integrates past experiences Controls higher-order Processes (e.g., judgment, reasoning) Language Comprehension Wernicke’s area Integrates auditory language (understanding of spoken words) Expression Broca’s area Regulates verbal expression Basal Ganglia Near lateral ventricles of Both cerebral hemispheres Control and facilitate learned and automatic movements Thalamus Below basal ganglia Relays sensory and motor input to and from the cerebrum Hypothalamus Below thalamus Regulates endocrine and autonomic functions Limbic System Lateral to hypothalamus Influences emotional behavior and basic drives such as feeding and sexual behavior Ventricles and Cerebrospinal Fluid The ventricles are four interconnected fluid-filled cavities. The lower portion of the fourth ventricle becomes the central canal in the lower part of the brainstem. The spinal canal extends centrally through the full length of the spinal cord. Cerebrospinal fluid (CSF) CSF circulates within the subarachnoid space that surrounds the brain, brainstem, and spinal cord. This fluid provides cushioning for the brain and the spinal cord, allows fluid shifts from the cranial cavity to the spinal cavity, and carries nutrients. The formation of CSF in the choroid plexus in the ventricles involves both passive diffusion and active transport of substances. CSF resembles an ultrafiltrate of blood. Although CSF is produced at an average rate of about 500 mL/day, many factors influence CSF production and absorption. The ventricles and central canal are normally filled with an average of 135 mL of CSF. Changes in the rate of production or absorption will result in a change in the volume of CSF that remains in the ventricles and central canal. Excessive buildup of CSF results in a condition known as hydrocephalus. The CSF circulates throughout the ventricles and seeps into the subarachnoid space surrounding the brain and spinal cord. It is absorbed primarily through the arachnoid villi (tiny projections into the subarachnoid space), into the intradural venous sinuses, and eventually into the venous system. The analysis of CSF composition provides useful diagnostic information related to certain nervous system diseases. CSF pressure is often measured in patients with actual or suspected intracranial injury. Increased intracranial pressure, indicated by ↑ CSF pressure, can force downward (central) herniation of the brain and brainstem. 7 Peripheral Nervous System The PNS includes all the neuronal structures outside the CNS. It consists of the spinal and cranial nerves, their associated ganglia (groupings of cell bodies), and portions of the ANS. Spinal Nerves The spinal cord is series of spinal segments; each segment contains a pair of dorsal (afferent) sensory nerve fibers or roots and ventral (efferent) motor fibers or roots, which innervate a specific region of the body. This combined motor-sensory nerve is called a spinal nerve (Fig. 5). The cell bodies of the voluntary motor system are located in the anterior horn of the spinal cord gray matter. The cell bodies of the autonomic (involuntary) motor system are located in the anterolateral portion of the spinal cord gray matter. The cell bodies of sensory fibers are located in the dorsal root ganglia just outside the spinal cord. On exiting the spinal column, each spinal nerve divides into ventral and dorsal rami, a collection of motor and sensory fibers that eventually goes to peripheral structures (e.g., skin, muscles, viscera). A dermatome is the area of skin innervated by the sensory fibers of a single dorsal root of a spinal nerve (Fig.6). The dermatomes give a general picture of somatic sensory innervation by spinal segments. A myotome is a muscle group innervated by the primary motor neurons of a single ventral root. The dermatomes and myotomes of a given spinal segment overlap with those of adjacent segments because of the development of ascending and descending collateral branches of nerve fibers. Fig.5 Cross section of spinal cord showing attachments of spinal nerves and coverings of the spinal cord. Cranial Nerves The cranial nerves (CNs) are the 12 paired nerves composed of cell bodies with fibers that exit from the cranial cavity. Unlike the spinal nerves, which always have both afferent sensory and efferent motor fibers, some CNs are only sensory, some only motor, and some both. Table 56-3 summarizes the motor and sensory components of the CNs. Fig. 56-7 shows the position of the CNs in relation to the brain and spinal cord. Just as the cell bodies of the spinal nerves are located in specific segments of the spinal cord, so are the cell bodies (nuclei) of the CNs located in specific segments of the brain. Exceptions are the nuclei of the olfactory and optic nerves. The primary cell bodies of the olfactory nerve are located in the nasal epithelium, and those of the optic nerve are in the retina. TABLE 56-3 CRANIAL NERVES Nerve Connection With Brain Function I Olfactory II Optic Anterior ventral cerebrum Lateral geniculate body of the thalamus Midbrain Sensory: from olfactory (smell) Sensory: from retina of eyes (vision) III Oculomotor 8 Motor: to four eye movement muscles and levator IV Trochlear Midbrain V Trigeminal Ophthalmic branch Maxillary branch Mandibular branch Pons Pons Pons VI Abducens VII Facial Pons Junction of pons and medulla VIII Vestibulocochlear Vestibular branch Cochlear branch IX Glossopharyngeal Junction of pons and medulla Junction of pons and medulla Medulla X Vagus Medulla XI Accessory Medulla & segments Medulla XII Hypoglossal superior spinal palpebrae muscle Parasympathetic: smooth muscle in eyeball Motor: to one eye movement muscle, the superior oblique muscle Sensory: from forehead, eye, superior nasal cavity Sensory: from inferior nasal cavity, face, upper teeth, mucosa of superior mouth Sensory: from surfaces of jaw, lower teeth, mucosa of lower mouth, and anterior tongue Motor: to muscles of mastication Motor: to the lateral rectus of the eye Motor: to facial muscles of expression and cheekmuscle Sensory: taste from anterior two thirds of tongue Sensory: from equilibrium sensory organ, the vestibular apparatus Sensory: from auditory sensory organ, the cochlea Sensory: from pharynx and posterior tongue, including taste Motor: to superior pharyngeal muscles Sensory: from much of viscera of thorax and abdomen Motor: to larynx and middle and inferior pharyngeal muscles Parasympathetic: heart, lungs, most of digestive system Motor: to sternocleidomastoid and trapezius muscles Motor: to muscles of tongue TABLE 56-4 GERONTOLOGIC ASSESSMENT DIFFERENCES Nervous System Component Central Nervous System Brain Peripheral Nervous System Cranial and spinal nerves Functional Divisions Motor Sensory* Changes Differences Findings in Assessment ↓ Cerebral blood flow and Alterations in mental functioning. metabolism Impaired ability to adapt to ↓ Efficiency of temperatureenvironmental temperature. regulating mechanism Conduction of nerve impulses ↓ Neurotransmitters, loss of slowed, response time slowed. neurons Changes in gait and ambulation. ↓ O2 supply Diminished kinesthetic sense. Cerebral tissue atrophy and ↑ size Altered balance, vertigo, syncope. of ventricles ↑ Postural hypotension. Proprioception diminished. ↓ Sensory input. Loss of myelin and ↓ conduction ↓ Reaction time in specific nerves. time ↓ Speed and intensity of neuronal Cellular degeneration, death of reflexes. neurons ↓ Muscle bulk ↓ Sensory receptors ↓ Electrical activity Atrophy of taste buds Degeneration and loss of fibers in olfactory bulb Degenerative changes in nerve 9 Diminished strength and agility. Diminished sense of touch, pain, and temperature. Slowing of or alteration in sensory reception. Signs of malnutrition, weight loss. Diminished sense of smell. cells in inner ear, cerebellum, and Poor ability to maintain balance, proprioceptive pathways widened gait. Reflexes ↓ Deep tendon reflexes ↓ Sensory conduction velocity Reticular Formation Reticular activating system Below-average reflex score. Sluggish reflexes, slowing of reaction time. Modification of hypothalamic Disturbances in sleep patterns. function, ↓ stage IV sleep Autonomic Nervous System Sympathetic nervous system and parasympathetic nervous system Morphologic features of ganglia, Orthostatic hypotension, systolic slowing of autonomic nervous hypertension. system responses Autonomic Nervous System The autonomic nervous system (ANS) is divided into the sympathetic and parasympathetic systems. The ANS governs involuntary functions of cardiac muscle, smooth muscle, and glands through both efferent and afferent pathways. The two systems function together to maintain a relatively balanced internal environment. The preganglionic cell bodies of the sympathetic nervous system (SNS) are located in spinal segments T1 through L2. The major neurotransmitter released by the postganglionic fibers of the SNS is norepinephrine, and the neurotransmitter released by the preganglionic fibers is acetylcholine. The preganglionic cell bodies of the parasympathetic nervous system (PSNS) are located in the brainstem and the sacral spinal segments (S2 through S4). Acetylcholine is the neurotransmitter released at both preganglionic and postganglionic nerve endings. SNS stimulation activates the mechanisms required for the “fight-or-flight” response that occurs throughout the body. In contrast, the PSNS is geared to act in localized and discrete regions. It serves to conserve & restore the body’s energy stores. The ANS provides dual and often reciprocal innervation to many structures. For example, the SNS increases the rate and force of heart contraction and the PSNS decreases the rate and force. Cerebral Circulation The brain’s blood supply arises from the internal carotid arteries (anterior circulation) and the vertebral arteries (posterior circulation), which are shown in Fig.-8. 1. Internal carotid arteries provide blood flow to anterior and middle portions of cerebrum. 2. Vertebral arteries join to form basilar artery and provide blood flow to brainstem, cerebellum, and posterior cerebrum. 3. Circle of Willisis formed by communicating arteries that join basilar & internal carotid arteries (Fig.-9). The circle of Willis is a safety valve for regulating cerebral blood flow when differential pressures or vascular occlusions are present. 4. Superior to circle of Willis, three pairs of arteries supply blood to the left and right hemispheres. The anterior cerebral artery feeds the medial and anterior portions of the frontal lobes. 5. The middle cerebral artery feeds outer portions of frontal, parietal, & superior temporal lobes. 6. The posterior cerebral artery feeds medial portions of the occipital and inferior temporal lobes. Venous blood drains from the brain through the dural sinuses, which form channels that drain into the two jugular veins. 11 FIG.6 The cranial nerves are numbered according to the FIG.7 Dermatomes of the body. order in which they leave the brain FIG. -8 Arteries of the head and neck. Brachiocephalic artery, right common carotid artery, right subclavian artery, and their branches. The major arteries to the head are the common carotid and vertebral arteries. FIG. -9 Arteries at the base of the brain. The arteries that compose the circle of Willis are the two anterior cerebral arteries joined to each other by the anterior communicating cerebral artery and to the posterior cerebral arteries by the posterior communicating arteries Blood-Brain Barrier The blood-brain barrieris a physiologic barrier between blood capillaries and brain tissue.5 This barrier protects the brain from harmful agents, while allowing nutrients and gases to enter. The structure of brain capillaries differs from that of other capillaries, so substances that normally pass into most tissues are prevented from entering brain tissue. Lipid-soluble compounds enter the brain easily, whereas water-soluble and ionized drugs enter the brain and the spinal cord slowly. 11 Thus the blood-brain barrier affects the penetration of drugs. Only certain drugs can enter the CNS from the bloodstream. Protective Structures Meninges The meninges consist of three protective membranes that surround the brain and spinal cord: dura mater, arachnoid, and pia mater. Skull The skull protects the brain from external trauma. It is composed of eight cranial bones and 14 facial bones. It has many ridges, prominences, and foramina (holes through which blood vessels and nerves enter the intracranial vault). The largest hole is the foramen magnum, through which the brainstem extends to the spinal cord. This foramen offers the only major space for the expansion of brain contents when increased intracranial pressure occurs. Vertebral Column The vertebral column protects spinal cord, supports head, & provides flexibility. The vertebral column is made up of 33 individual vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 sacral (fused into one), and 4 coccygeal (fused into one). Each vertebra has a central opening through which the spinal cord passes. Intervertebral discs occupy the spaces between vertebrae. Fig. -10 shows the vertebral column in relation to the trunk. FIG. -10 The vertebral column (three views). ASSESSMENT OF NERVOUS SYSTEM TABLE 5 HEALTH HISTORY Nervous System Health Perception–Health Management What are your usual daily activities? Do you use alcohol, tobacco, or recreational drugs?* What safety practices do you perform in a car? On a motorcycle? On a bicycle? 12 Do you have hypertension? If so, is it controlled? Have you ever been hospitalized for a neurologic problem?* Nutritional-Metabolic Are you able to feed yourself? Do you have any problems getting adequate nutrition because of Chewing or swallowing difficulties, facial nerve paralysis, or poor muscle coordination?* Give a 24-hr dietary recall. Elimination Do you have incontinence of your bowels or bladder?* Do you ever experience problems with hesitancy, urgency, retention?* Do you postpone defecation?* Do you take any medication to manage neurologic problems? If so, what? Activity-Exercise Describe any problems you experience with usual activities and exercise as a result of a neurologic problem. Do you have weakness or lack of coordination?* Are you able to perform your personal hygiene needs independently?* Sleep-Rest Describe your sleep pattern. When you have trouble sleeping, what do you do? Cognitive-Perceptual Have you noticed any changes in your memory?* Do you experience dizziness, heat or cold sensitivity, numbness, or tingling?* Do you have chronicpain?* Do you have any difficulty with verbal or written communication?* Have you noticed any changes in vision or hearing?* Self-Perception–Self-Concept How do you feel about yourself, about who you are? Describe your general emotional pattern. Role-Relationship Have you experienced changes in roles such as spouse, parent, or breadwinner?* Sexuality-Reproductive Are you dissatisfied with sexual functioning?* Are problems related to sexual functioning causing tension in an important relationship?* Do you feel the need for professional counseling related to your sexual functioning?* Coping–Stress Tolerance Describe your usual coping pattern. Do you think your present coping pattern is adequate to meetthe stressors of your life?* What needs are unmet by your current support system? Value-Belief Describe any culturally specific beliefs and attitudes that may influence your care. DIAGNOSTIC STUDIES OF NERVOUS SYSTEM Numerous diagnostic studies are available to assess the nervous system. Tables 56-8 and 56-9 present the most common studies, and select studies are described in more detail below. 13 Cerebrospinal Fluid Analysis CSF analysis provides information about a variety of CNS diseases. o Normal CSF fluid is clear, colorless, odorless, and free of red blood cells and contains little protein. o Normal CSF values are listed in Table 56-9. CSF may be obtained through lumbar puncture or ventriculostomy. Table -9 Normal Cerebrospinal Fluid Values Parameter Specific gravity pH Appearance Red blood cells (RBCs) White blood cells (WBCs) Protein • Lumbar • Cisternal • Ventricular Glucose Microorganisms Pressure Normal Value 1.007 7.35 Clear, colorless None 0-5 cells/µL (0-5×106 cells/L) 15-45 15-25 5-15 40-70 None 60-150 mg/dL mg/dL mg/dL mg/dL (0.15-0.45 g/L) (0.15-0.25 g/L) (0.05-0.15 g/L) (2.2-3.9 mmol/L) mm H2O Lumbar Puncture Lumbar puncture is the most common method of sampling CSF. A lumbar puncture is contraindicated in the presence of increased intracranial pressure or infection at the site of puncture. Before the procedure, o Have the patient void. o The patient is side lying. o A seated position may also be used. o Inform the patient that, as a sterile needle is passed between two lumbar vertebrae, he or she may feel temporary pain radiating down the leg. o A manometer is attached to the needle to obtain a CSF pressure. o CSF is withdrawn in a series of tubes and sent for analysis. o Monitor for headache intensity, meningeal irritation (nuchal rigidity), or signs and symptoms of local trauma (e.g., hematoma, pain). FOCUSED ASSESSMENT Nervous System Use this checklist to make sure the key assessment steps have been done. Subjective Ask the patient about any of the following and note responses. Blackouts/loss of memory Weakness, numbness, tingling in arms or legs Headaches, especially new onset Loss of balance/coordination Orientation to person, place, and time 14 YN YN YN YN YN Objective: Diagnostic Check the following laboratory results for critical values. Lumbar puncture CT or MRI of brain EEG Objective: Physical Examination Inspect/Observe General level of consciousness/orientation Oropharynx for gag reflex and soft palate movement Peripheral sensation of light touch and pinprick (face, hands, feet) Smell with an alcohol wipe Eyes for extraocular movements, PERRLA, peripheral vision, nystagmus Gait for smoothness and coordination Palpate Strength of neck, shoulders, arms, and legs full and symmetric Percuss Reflexes ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ Radiologic Studies Computed Tomography Computed tomography (CT) scans provide a rapid means of obtaining radiographic images of the brain (see Fig. 56-15, A). When viewed in succession, these images provide a three-dimensional representation of the intracranial contents. Denser material appears white, whereas fluid and air appear dark or black. Brain CT can be completed both with and without contrast media in only a few minutes. Magnetic Resonance Imaging Magnetic resonance imaging (MRI) provides greater detail than CT and improved resolution (detail) of the intracranial structures (see Fig. 56-15, B). However, MRI requires a longer time to complete and may not be appropriate in life-threatening emergencies. Techniques of functional MRI (fMRI) provide time-related (temporal) images that can be used to evaluate how the brain responds to various stimuli. Cerebral Angiography Cerebral angiography is indicated when vascular lesions or tumors are suspected. A catheter is inserted into femoral (or brachial) artery and passed through aortic arch and into the base of a carotid or a vertebral artery for injection of contrast media. Timed sequence radiographic images are obtained as contrast flows through arteries, smaller vessels, and veins. This study can help to identify and localize abscesses, aneurysms, hematomas, arteriovenous malformations, arterial spasm, and certain tumors. Because this is an invasive procedure, adverse reactions may occur; patient may have an allergic (anaphylactic) reaction to the contrast medium. Once the patient returns to his or her room after the procedure, observe for bleeding at the catheter puncture site (usually the groin). 15 Electrographic Studies Electroencephalography Electroencephalography (EEG) involves recording electrical activity of the surface cortical neurons of the brain by electrodes placed on specific areas of the scalp. Specific tests may be done to evaluate brain’s electrical response to lights & loud noises. This test is done to evaluate not only cerebral disease but also the CNS effects of many metabolic and systemic diseases. Among the cerebral diseases assessed by EEG are seizure disorders, sleep disorders, cerebrovascular lesions, and brain injury. Prolonged EEG monitoring is becoming a common test to diagnose and treat seizure disorders. An EEG is noninvasive. Assure patients that there is no risk of electric shock. Electromyography and Nerve Conduction Studies Electromyography (EMG) is recording of electrical activity associated with innervation of skeletal muscle. Needle electrodes are inserted into the muscle to record specific motor units because recording from the skin is not sufficient. Normal muscle at rest shows no electrical activity. Electrical activity occurs only when the muscle contracts. Activity altered in diseases of muscle (e.g., myopathic conditions) or in disorders of muscle innervation (e.g., segmental or LMN lesions, peripheral neuropathic conditions). Nerve conduction studies involve applying a brief electrical stimulus to a distal portion of a sensory or mixed nerve and recording the resulting wave of depolarization at some point proximal to the stimulation. For example, a stimulus can be applied to the forefinger and a recording electrode placed over the median nerve at the wrist. The time between the stimulus onset and the initial wave of depolarization at the recording electrode is measured (nerve conduction velocity). Damaged nerves have slower conduction velocities. Evoked Potentials Evoked potentials are recordings of electrical activity associated with nerve conduction along sensory pathways. The electrical activity is generated by a specific sensory stimulus related to the type of study (e.g., clicking sounds for auditory evoked potentials, mild electrical pulses for somatosensory evoked potentials).11 Electrodes placed on specific areas of skin & the scalp record electrical activity. Increases in the normal time from stimulus onset to a given peak (latency) indicate slowed nerve conduction or nerve damage. This technique is useful in diagnosing abnormalities of the visual or auditory systems because it reveals whether a sensory impulse is reaching the appropriate part of the brain. Indications for these tests include evaluation of consciousness, multiple sclerosis (optic neuritis), and acoustic neuroma. TABLE 6 NORMAL PHYSICAL ASSESSMENT OF NERVOUS SYSTEM Parameter Findings Alert and oriented, orderly thought processes. Mental Appropriate mood and affect. status Smell intact to soap or coffee. Cranial Visual fields full to confrontation. nerves Intact extraocular movements. 16 Motor system Sensory system Reflexes‡ No nystagmus. Pupils equal, round, reactive to Light and accommodation. Intact facial sensation to light touch and pinprick. Facial movements full. Intact gag & swallow reflexes. Symmetric smile. Midline protrusion of tongue. Full strength with head turning and shoulder shrugging. Normal gait and station. Normal tandem walk. Negative Romberg test. Normal and symmetric muscle bulk, tone, and strength. Smooth performance of finger-nose, heel-shin movements. Intact sensation to light touch, position sense, pinprick, heat and cold. Biceps, triceps, brachioradialis, patellar & Achilles tendon reflexes 2/5 bilaterally. Downgoing toes with plantar stimulation. TABLE 7 ASSESSMENT ABNORMALITIES Nervous System Finding Description Mental Status Altered consciousness Anosognosia Speech Aphasia, dysphasia Dysarthria Eyes Anisocoria Diplopia Homonymous hemianopsia Cranial Nerves Dysphagia Ophthalmoplegia Papilledema Motor System Apraxia Ataxia Dyskinesia Hemiplegia Nystagmus Sensory System Analgesia Possible Etiology and Significance Stuporous, mute, diminished response to verbalcues or pain Inability to recognize bodily defect or disease Intracranial lesions, metabolic psychiatric disorders Lesions in right parietal cortex Loss of or impaired language faculty (comprehension, expression, or both) Lack of coordination in articulating speech Left cerebral cortex lesion Cerebellar or cranial nerve lesion Antiseizure drugs, sedatives, hypnotic drug toxicity (including alcohol) Inequality of pupil size Double vision Loss of vision in one side of visual field Optic nerve injury Lesions affecting nerves of extraocular muscles, cerebellar damage Lesions in the contralateral occipital lobe Difficulty in swallowing Paralysis of eye muscles “Choked disc,” swelling of optic nerve head Lesions involving motor pathways of CNs IX, X (including lower brainstem) Lesions in brainstem Increase in intracranial pressure Inability to perform learned movements despite having desire and physical ability to perform them Lack of coordination of movement Impairment of voluntary movement, resulting in fragmentary or incomplete movements Paralysis on one side Jerking or bobbing of eyes as they track moving object Cerebral cortex lesion Lesions of sensory or motor pathways, cerebellum Antiseizure drugs, sedatives, hypnotic drug toxicity (including alcohol) Disorders of basal ganglia, idiosyncratic reaction to psychotropic drugs Stroke and other lesions involving motor cortex Lesions in cerebellum, brainstem, vestibular system Antiseizure drugs,sedatives, hypnotic toxicity (including alcohol Loss of pain sensation Lesion in spinothalamic tract or thalamus, specific medications 17 disorder, Anesthesia Absence of sensation Paresthesia Astereognosis Alteration in sensation Inability to recognize form of object by touch Reflexes Extensor plantar response Deep tendon reflexes Spinal Cord Bladder dysfunction o Atonic (autonomous) o Hypotonic o Hypertonic Paraplegia Tetraplegia (quadriplegia) Upgoing toes stimulation Diminished or response with plantar absent motor Absence of muscle tone and contractility, enlargement More ability than atonic bladder but less than normal Increase in muscle tone, diminished capacity, reflex emptying, dribbling, incontinence Paralysis of lower extremities Paralysis of all extremities Lesions in spinal cord, thalamus, sensory cortex, or peripheral sensory nerve Specific medications Lesions in the posterior column or sensory cortex Lesions in parietal cortex Suprasegmental or upper motor neuron lesion Lower motor neuron lesions Of capacity, no sensation of discomfort, overflow With large residual, inability to voluntarily empty Early stage of spinal cord injury Interruption of afferent pathways from bladder Lesions in pyramidal tracts (efferent pathways) Spinal cord transaction or mass lesion (thoracolumbar region) Spinal cord transaction or mass lesion (cervical region) TABLE 56-8 DIAGNOSTIC STUDIES Study Description and Purpose Cerebrospinal Fluid Analysis Nursing Responsibility CSF is aspirated by needle insertion in L3-4 or L4-5 interspace to assess many CNS diseases. Ensure that patient does not have signs of increased ICP because of the risk of downward herniation from CSF removal. Patient assumes and maintains lateral recumbent position. Use strict aseptic technique. Ensure labeling of CSF specimens in proper sequence. Encourage fluids. Monitor neurologic signs and VS. Administer analgesia as needed. Radiology Skull and spine xrays Simple x-ray of skull and spinal column is done to detect fractures, bone erosion, calcifications, abnormal vascularity. Explain that procedure is noninvasive. Explain positions to be assumed. Cerebral angiography Serial x-ray visualization of intracranial and extracranial blood vessels is performed to detect vascular lesions and tumors of brain (Fig. 56-14). Contrast medium is used. Preprocedure: Assess patient for stroke risk before procedure, since thrombi may be dislodged during procedure. Withhold preceding meal. Explain that patient will have hot flush of head and neck when contrast medium is injected. Administer premedication. Explain need to be absolutely still during procedure. Postprocedure: Monitor neurologic signs and VS every 15-30 min for first 2 hr, every hour for next 6 hr, then every 2 hr for 24 hr. Maintain bed rest until patient is alert and VS are stable. Report any neurologic status changes. Computer-assisted x-ray of multiple cross sections of body parts to detect problems such as hemorrhage, tumor, cyst, edema, infarction, brain atrophy & other abnormalities (Fig. 5615, A). Contrast media may be used to enhance Assess for contraindications to contrast media, including allergy to shellfish, iodine, or dye. Explain appearance of scanner. Instruct patient to remain still during procedure. Lumbar puncture Computed tomography scan (CT) 18 visualization of brain structures. Magnetic resonance imaging (MRI) Imaging of brain, spinal cord, and spinal canal by means of magnetic energy (Fig 56-15, B). Used to detect strokes, multiple sclerosis, tumors, trauma, herniation, and seizures. No invasive procedures are required. Contrast media may be used to enhance visualization. Has greater contrast in images of soft tissue structures than CT scan. Screen patient for metal parts and pacemaker in body. Instruct patient on need to lie very still for up to 1 hr. Sedation may be necessary if patient is claustrophobic Magnetic resonance angiography (MRA) Uses differential signal characteristics of flowing blood to evaluate extracranial and intracranial blood vessels. Provides both anatomic and hemodynamic information. Can be used in conjunction with contrast media. Similar to MRI (see above) Positron emission tomography (PET) Measures metabolic activity of brain to assess cell death or damage. Uses radioactive material that shows up as a bright spot on the image (see Fig. 16-7). Used for patients with stroke, Alzheimer’s disease, seizure disorders, Parkinson’s disease, and tumors. Explain procedure to patient. Explain that two IV lines will be inserted. Instruct patient not to take sedatives or tranquilizers. Have patient empty bladderbefore procedure. Patient may be asked to perform different activities during test. Single-photon emission computed tomography (SPECT) A method of scanning similar to PET, but it uses more stable substances and different detectors. Radiolabeled compounds are injected, and their photon emissions can be detected. Images made are accumulation of labeled compound. Used to visualize blood flow or O2 or glucose metabolism in the brain. Useful in diagnosing strokes, brain tumors, and seizure disorders. Similar to PET (see above) Myelogram X-ray of spinal cord and vertebral column after injection of contrast medium into subarachnoid space. Used to detect spinal lesions (e.g., herniated or ruptured disc, spinal tumor). Preprocedure: Administer sedative as ordered. Instruct patient to empty bladder. Inform patient that test is performed with patient on tilting table that is moved during test. Postprocedure: Patient should lie flat for a few hours. Encourage fluids. Monitor neurologic signs and VS. Headache, nausea, and vomiting may occur after procedure Electrographic Studies Electroencephalogra phy (EEG) Electrical activity of brain is recorded by scalp electrodes to evaluate seizure disorders, cerebral disease, CNS effects of systemic diseases, brain death. Inform patient that procedure is noninvasive and without danger of electric shock. Determine whether any medications (e.g., tranquilizers, antiseizure drugs) should be withheld. Resume medications and instruct patient towash electrode paste out of hair after test. Magnetoencephalog raphy (MEG) Uses a biomagnetometer to detect magnetic fields generated by neural activity. It can accurately pinpoint the part of the brain involved in a stroke, seizure, or other disorder or injury. Measures extracranial magnetic fields and scalpelectric field (EEG). MEG, a passive sensor, does not make physical contact with patient. Explain procedure to patient. Electromyography (EMG) and nerve conduction studies Electrical activity associated with nerve and skeletal muscleis recorded by insertion of needle electrodes to detect muscle and peripheral nerve disease. Inform patient that pain and discomfort are associated with insertion of needles. Evoked potentials Electrical activity associated with nerve conduction along sensory pathways is recorded by electrodes placed on skin and scalp. Stimulus generates the impulse. Explain procedure to patient. 19 Procedure is used to diagnose disease (e.g., multiple sclerosis), locate nerve damage, and monitor function intraoperatively. Ultrasound Carotid duplex studies Combined ultrasound and pulsed Doppler technology. Probe is placed over the carotid artery and slowly moved along the course of the common carotid artery. Frequency of reflected ultrasound signal corresponds to the blood velocity. Increased blood flow velocity can indicate stenosis of a vessel. Explain procedure to patient. Duplex scanning is anoninvasive study that evaluates the degree of stenosis of the carotid and vertebral arteries Transcranial Doppler Same technology as carotid duplex, but evaluates blood flow velocities of the intracranial blood vessels. Probe is placed on the skin at various “windows” in the skull (areas in the skull that have only thin bony covering) to register velocities of the blood vessels. Explain procedure to patient. Noninvasive technique that is useful in assessing vasospasm associated with subarachnoid hemorrhage, altered intracranial blood flow dynamics associated with occlusive vascular disease, presence of emboli & cerebral autoregulation. 21