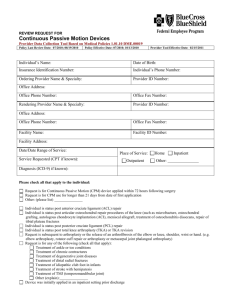
The Journal of Arthroplasty 32 (2017) 2604e2611 Contents lists available at ScienceDirect The Journal of Arthroplasty journal homepage: www.arthroplastyjournal.org Review Arthrofibrosis Associated With Total Knee Arthroplasty Victor A. Cheuy, PhD a, *, Jared R.H. Foran, MD b, Roger J. Paxton, PhD a, Michael J. Bade, PT, PhD a, Joseph A. Zeni, PT, PhD c, Jennifer E. Stevens-Lapsley, PT, PhD a, d a Physical Therapy Program, Department of Physical Medicine and Rehabilitation, University of Colorado, Aurora, Colorado Panorama Orthopaedics and Spine Center, Golden, Colorado c Department of Physical Therapy, University of Delaware, Newark, Delaware d Geriatric Research, Education and Clinical Center, Veterans Affairs Medical Center, Denver, Colorado b a r t i c l e i n f o a b s t r a c t Article history: Received 17 August 2016 Received in revised form 3 January 2017 Accepted 5 February 2017 Available online 14 February 2017 Background: Arthrofibrosis is a debilitating postoperative complication of total knee arthroplasty (TKA). It is one of the leading causes of hospital readmission and a predominant reason for TKA failure. The prevalence of arthrofibrosis will increase as the annual incidence of TKA in the United States rises into the millions. Methods: In a narrative review of the literature, the etiology, economic burden, treatment strategies, and future research directions of arthrofibrosis after TKA are examined. Results: Characterized by excessive proliferation of scar tissue during an impaired wound healing response, arthrofibrotic stiffness causes functional deficits in activities of daily living. Postoperative, supervised physiotherapy remains the first line of defense against the development of arthrofibrosis. Also, adjuncts to traditional physiotherapy such as splinting and augmented soft tissue mobilization can be beneficial. The effectiveness of rehabilitation on functional outcomes depends on the appropriate timing, intensity, and progression of the program, accounting for the patient's ability and level of pain. Invasive treatments such as manipulation under anesthesia, debridement, and revision arthroplasty improve range of motion, but can be traumatic and costly. Future studies investigating novel treatments, early diagnosis, and potential preoperative screening for risk of arthrofibrosis will help target those patients who will need additional attention and tailored rehabilitation to improve TKA outcomes. Conclusion: Arthrofibrosis is a multi-faceted complication of TKA, and is difficult to treat without an early, tailored, comprehensive rehabilitation program. Understanding the risk factors for its development and the benefits and shortcomings of various interventions are essential to best restore mobility and function. © 2017 Elsevier Inc. All rights reserved. Keywords: arthrofibrosis total knee arthroplasty range of motion stiffness Characterizing Arthrofibrosis Arthrofibrosis is a well-known complication of injury or trauma, characterized by the production of excessive fibrous scar tissue in a joint [1e4]. The major consequence of arthrofibrosis is the loss of range of motion because of the painful stiffness of proliferated scar tissue, which interferes with the patient's ability to adequately perform functional tasks of daily living [5,6]. Arthrofibrosis is a debilitating complication after knee surgery that may also result in One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.arth.2017.02.005. * Reprint requests: Victor A. Cheuy, PhD, Mail Stop C244, 13121 East 17th Ave., Aurora, CO 80045. http://dx.doi.org/10.1016/j.arth.2017.02.005 0883-5403/© 2017 Elsevier Inc. All rights reserved. pain that does not subside at predictable time points, pain with palpation, lack of patellar movement with quadriceps muscle contraction, or a knee joint that is warm or swollen unrelated to effusion [7,8]. There is a lack of consensus on the diagnostic criteria for arthrofibrosis of the knee, which obscures its true prevalence after surgical procedures [9,10]. The spectrum of classification ranges from broadly assessing patient difficulty with activities of daily living attributable to limited range of motion (including decreased range of motion preoperatively), to quantitative thresholds of flexion and/or extension loss [5,11]. These quantitative thresholds vary and include a flexion contracture of >15 degrees and/or <75 degrees of flexion; >10 degrees of extension deficit and/or <95 degrees of flexion; or a total knee arc range of motion <70 degrees [12e14]. Imaging techniques have been used to supplement patient history and clinical examinations, and can be valuable in assisting V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 2605 Fig. 1. Risk factors for arthrofibrosis and typical postoperative care strategies. NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physical therapy; RICE, rest-ice-compressionelevation; ROM, range of motion; TKA, total knee arthroplasty. with diagnosis and treatment planning [15]. Magnetic resonance imaging (MRI) and ultrasound have both demonstrated the ability to detect focal fibrous proliferation based on heterogeneous signal intensity in the knee, ankle, and foot [15e17]. However, MRI is not part of the standard of care, even with the development of metal suppression sequences to reduce artifacts and improve image quality [18,19]. Advanced imaging is used (if at all) only after patient history, physical examination, and radiographs all fail to identify the cause of pain and/or stiffness after total knee arthroplasty (TKA) [20]. MRI also suffers from the drawbacks of cost, the timeconsuming nature of scans, and concerns over patient claustrophobia and keeping still for extended periods. The etiology of arthrofibrosis is multifactorial, and numerous preoperative, intraoperative, and postoperative risk factors have been identified (Fig. 1). Decreased preoperative knee range of motion, higher complexity surgery (ie, amount of trauma, length of surgery), and history of surgery increase the risk of excessive scar tissue after TKA [21]. Previous studies have shown the rate of arthrofibrosis doubles or even triples when patients have undergone previous surgeries for multiple ligamentous injuries or surgeries that require immobilization [9,22,23]. Postoperative factors contributing to arthrofibrosis include poor patient motivation and immobility, delay in starting a rehabilitation program, lack of compliance with prescribed rehabilitation, poor pain tolerance, and infection [5,9,23]. In addition, a genetic predisposition to forming excessive intraarticular scar tissue after injury and/or surgery has been implicated in several studies [24e26]. The exact pathophysiology of how these factors cause arthrofibrosis is not completely clear, but what is known is the coordination of cell growth, differentiation, and death controlled by various cytokines and growth factor signaling is disrupted, directly affecting tissue homeostasis and organization, and allowing for uninhibited proliferation of fibroconnective tissue [9,22,27]. Fibrosis can occur in many different organs (eg, skin, liver, lungs), and can ultimately lead to organ failure [25,28,29]. In the normal wound healing response, the cascade of biological responses is tightly regulated. The migration of inflammatory cells and the proliferation of fibroblasts trigger the release of cytokines, growth factors, and reactive oxygen species that are responsible for tissue remodeling and restoring tissue integrity [30]. Once the healing process is complete, the inflammatory cells undergo apoptosis (ie, programmed cell death), the release of signaling molecules stops, and the inflammatory response critical to restoring tissue to its functional state subsides [30,31]. However, the arthrofibrotic condition is characterized by a lack of apoptosis in the proinflammatory phase, resulting in an imbalance between synthesis 2606 V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 and degradation [29,31]. Persistent transforming growth factor-b (TGF-b) and bone morphogenetic protein 2 (BMP2) secretion and downstream responses are thought to contribute to a sustained inflammatory response [25,28,31,32]. Without apoptosis to balance proliferation during this time, pathologic scar formation is inevitable, where functional cell types are eventually replaced by connective tissue [33,34]. Proteoglycans, collagens, and extracellular matrix components aggressively accumulate in the intercellular space and stiffen, creating a fibrotic state [25,30,31,33]. Interventions directed at some of these potential biological targets have not been successful, and there has been no specific pharmacological therapy able to prevent or cure arthrofibrosis [29]. Association With TKA TKA is the standard of care to manage the pain and disability associated with end-stage knee osteoarthritis, with more than 700,000 TKA surgeries performed annually in the United States [35]. Arthrofibrosis is a debilitating complication of TKA, with a reported incidence of between 1% and 13% postoperatively [4,6,10,13,36]. The range of values can be attributed to the varying quantitative thresholds of flexion and/or extension loss used to define arthrofibrosis, as described previously. As a predominant failure mechanism, arthrofibrosis accounts for 28% of hospital readmissions due to surgical complications within 90 days of discharge, and 10% of all revisions within 5 years of initial surgery within the United States [37,38]. Patients with arthrofibrosis are at elevated risk for prolonged, high treatment costs, especially for those whose limited range of motion persists despite varied treatment techniques [38,39]. One quarter of patients treated with a motion-restoring surgical procedure still required multiple surgeries, with only 37% reporting satisfactory results [22]. With the incidence of TKA projected to reach 3.5 million by 2030, the growing cohort of TKA patients with postoperative arthrofibrosis provides an important target for research [40]. The excessive scar tissue formation in the knee joint with arthrofibrosis results in decreased knee extension and flexion range of motion, leading to tissue contracture, increased pain, and functional deficits in many activities of daily living (eg, standing up, walking, stair climbing) [11,41e44]. Previous studies have shown that the functional deficits vary depending on the severity of flexion loss; approximately 70 degrees of flexion are necessary for typical gait, 80 -90 for stair ascent and descent, and at least 125 for squatting to pick an object up from the floor [9,43,45]. Loss of extension can be even more incapacitating and difficult to manage, as just small limitations in extension range of motion increase energy consumption and place undue strain on the quadriceps muscles [9,27,45]. As little as a 5 loss in extension results in altered gait mechanics (eg, limping) and walking on a 15 flexed knee requires 22% more extensor demand [9,46]. over a primary); those receiving a revision are also twice as likely to require readmission (higher rates of complications such as infection); and those receiving a revision may have worse outcomes, as patients may remain stiff even after their procedure [38,49e52]. If the use of invasive techniques for management of arthrofibrosis could be minimized while still achieving adequate range of motion, the costs and incidence of complications associated with arthrofibrosis could be reduced. Rehabilitation is comparatively low cost, at approximately $1500 per knee arthroplasty [53]. Importance of Initial Management Physiotherapy rehabilitation is a fundamental component of the postoperative care after primary TKA. The arthrofibrotic knee represents a difficult challenge for the therapist that requires careful attention and skill to improve functional outcomes and potentially save the health care system tens of thousands of dollars per patient in future medical costs. An effective rehabilitation program emphasizes (1) the management of inflammation, swelling, and pain, (2) frequent monitoring, and (3) maintaining or restoring range of motion as soon as arthrofibrosis is recognized [27,54e56]. This is in contrast to the typical intervention after TKA, in which the emphasis is on increasing muscle strength of the quadriceps as well as managing inflammation and swelling. However, because range of motion is the limiting factor in patients with arthrofibrosis, the intervention needs to prioritize range of motion deficits early before the fibrotic tissue has a chance to mature and become resistant to physiotherapy later on [10]. The arthrofibrotic knee requires intensive, structured, and well-monitored rehabilitation to aggressively treat range of motion deficits, and its effectiveness is also highly dependent on patient motivation and compliance [5,11,22,57e59]. Concurrently, adequate pain management must be maintained and progress should be monitored closely [55]. The intensity of rehabilitation should be aggressive, as intense physical therapy was found to be the most influential factor for postoperative flexion, while a decrease in days of aggressive inpatient physical therapy correlated with an increased rate of MUAs [60,61]. Preoperative educational meetings can also engage patients as active participants in their own healthcare to address motivation and compliance; attendance of educational meetings was associated with a significantly decreased risk of postoperative stiffness requiring MUA [59]. Several supplements to a prescribed rehabilitation program exist that target range of motion, with a long-term goal of avoiding additional operations if possible. These adjuncts to rehabilitation may help maintain or even promote range of motion gains achieved with physical therapy, with implementation and timing of these treatment modalities typically customized to each patient (see below) [22,41]. Nonsteroidal Anti-Inflammatory Drugs and the Rest-IceCompression-Elevation Method Economic Burden of Arthrofibrosis Post-TKA TKA is generally a successful and cost-effective procedure, but adverse outcomes like arthrofibrosis can lead to costly follow-up procedures [47]. Although manipulation under anesthesia (MUA) is typically the initial treatment option for post-TKA arthrofibrosis, it is no guarantee of improved function, decreased pain, and increased satisfaction [14,48]. More aggressive procedures may improve knee range of motion, but are more traumatic and are associated with an increased risk of continued postoperative treatment. Furthermore, compared with a primary TKA, a revision TKA is more costly (1.6 times less cost-effective for the same increase in Western Ontario and McMaster Universities Arthritis Index score, and an increased hospitalization cost of almost $7000 Nonsteroidal anti-inflammatory drugs and the rest-icecompression-elevation method assist with decreasing the inflammatory response, pain, and swelling. Shortening the inflammatory phase decreases the pathogenesis of scar tissue, whereas proper pain and swelling management allow rehabilitation to begin or to continue without excessive patient discomfort [62]. Such symptom management is important for patient motivation and adherence to therapy, which are both crucial to successful outcomes, as gains in range of motion may be lost because of lack of activity or immobility [63]. Therapist supervision is vital in determining if acute inflammation persists through treatment. Although immediate and aggressive range of motion exercises improve outcomes for patients with early motion problems, if inflammation is not well V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 2607 Fig. 2. Management algorithm for arthrofibrosis of the knee after total knee arthroplasty. controlled, such aggressive intervention may have the opposite effect and actually promote scar tissue formation [64]. In these cases, a milder, but consistently implemented range of motion exercise intervention might achieve the best results. Continuous Passive Motion Devices Although active motion training is preferred, continuous passive motion (CPM) devices are occasionally used to promote flexion. However, several studies have found no advantage in improving range of motion or any greater benefit when paired with physiotherapy [65e67]. Boese et al [68] randomized a total of 160 subjects into 3 groups: CPM device on and moving from the immediate postoperative period, CPM device on and stationary at 90 flexion for the first night and then moving throughout the rest of their stay, and no CPM. They found no significant differences in all outcome variables (range of motion, swelling, blood loss, and pain scores) and that CPM provided no benefit to patients recovering from TKA [68]. systematic review of 12 randomized controlled trials investigating bracing after ACL reconstruction rehabilitation found no evidence that range of motion was affected by brace use, findings which may extend to bracing after TKA as well [69]. Both static progressive splints, which use stress relaxation to stretch tissues, and dynamic progressive splints, which apply a low-grade force to the joint to gradually flex or extend the joint, have been shown to improve knee flexion deficits by 19 and knee flexion contractures by 7 -19 [39,71]. However, research in this area is limited to only 2 small cohort studies. Neuromuscular Electrical Stimulation Neuromuscular electrical stimulation applies an electrical current that overrides voluntary activation deficits to help re-educate the quadriceps muscle to contract normally [72]. Improving muscle function increases the speed of recovery and long-term functional performance, and may help reduce or prevent extension lag [41,72,73]. Bracing Soft Tissue Mobilization Static bracing is often used to maintain full extension range of motion [8,69]. Unfortunately, an extension brace may worsen arthrofibrosis due to limited flexion and, if bracing is used, the recommendation is alternating periods of bracing with periods of motion so as to limit development of stiffness [8,70]. Bracing is common practice after anterior cruciate ligament (ACL) reconstruction, and although it is a different pathology of the knee, a Mechanical soft-tissue stimulation with hand-held instruments (Astym, Performance Dynamics Inc, Muncie, Indiana) has also been shown to improve knee flexion deficits by 35 and knee flexion contractures by 12 in a small cohort of individuals who had failed to respond to traditional rehabilitation and MUA [74]. The rationale is the topical application of appropriate shear force and pressure 2608 V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 Table 1 Indications and Contraindications for Surgical Treatment Modalities. Procedure Indications Contraindications MUA [75,76] 90 degrees of flexion at 6-wk follow-up Within 3 mo of primary TKA Arthroscopic and open debridement [6,77] Revision total knee arthroplasty [4] Recurrent stiffness after physical therapy and MUA First attempt arthroscopic, then open More than 3 mo after primary TKA Clear diagnosis for cause of stiffness, which can be corrected operatively Preferably within 2 y of primary TKA Infection, wound problems >10 degrees of extension loss (fracture concern) Component malalignment Infection, wound problems Component malalignment Extrinsic source of stiffness Insufficient pain and functional limitation to outweigh risk of additional surgery MUA, manipulation under anesthesia. stimulates regeneration of damaged tissues and breakdown of scar tissue. Treatment Modalities Post-TKA After Physical Therapy Arthrofibrosis is a challenging complication after primary TKA because deficits in range of motion can persist, mitigating the therapeutic effects of rehabilitation [41]. Treatment options available after physical therapy are MUA, debridement, and revision TKA (Fig. 2), whose indications and contraindications are summarized in Table 1. MUA Management of arthrofibrosis with MUA is typically the first option when range of motion has not improved with physiotherapy in the early postoperative period, as it is the least invasive operative procedure and the scar tissue has not yet matured [10,48,78,79]. The reported incidence of patients undergoing a MUA after TKA to address limited range of motion is between 2% and 6% [48,58,75,76]. The most common technique for MUA is general anesthesia, muscle relaxants, and a combination of administered hip and knee flexion [80]. While the patient is under anesthesia, the physician flexes the hip to 90 , and progressively flexes and extends the knee while receiving auditory and tactile feedback of the adhesions breaking away, culminating with several 20-30 second holds at the new maximal knee positions [81]. Historically, there has been disagreement on the optimal interval of time between TKA and MUA [75]. Initially, no major differences were found in knee flexion improvement between MUA performed early (12 weeks postop) and late (>12 weeks postop) [82,83]. However, recent research has found an inverse relationship between time to MUA postoperatively and final range of motion, where earlier MUA increased flexion range of motion 30 42 and overall knee range of motion 31 -47 [13,75,78,80,84,85]. Namba and Inacio [48] compared patients who received MUA within or beyond 3 months of surgery (1.8 [SD 0.7] vs 5.5 [SD 3.0] months, respectively), and found that those patients who received MUA beyond 3 months gained approximately half the flexion range of motion of the cohort who had MUA within 3 months (17 vs 33 ). Issa et al [86] found that patients who underwent manipulation within 12 weeks achieved double the mean gain in flexion (36.5 vs 17 ), over 20 more in total arc range of motion (119 vs 95 ), and had higher Knee Society objective and function scores than those who had late MUA. No significant differences in these outcomes were found between patients who received an MUA within 6 weeks and between 7 and 12 weeks. A recent survey of 82 surgeons found confirmatory attitudes toward MUA timing, where 71% performed MUA within 3 months, while only 19% performed manipulations between 3 and 6 months postoperatively [5]. With patients typically returning to clinic 4-6 weeks postoperatively, manipulation of those with severely limited motion should not be delayed much longer, as potential range of motion gains begin to decrease and incidence of subsequent revision TKA increase (from 3.8%-5.3%) after 8 weeks post-TKA [58,75,76]. MUA may not be effective for the severely stiff knee, in which flexion range of motion is less than 70 , or for those who require multiple sessions of MUA, as both these clinical presentations tend to have poorer outcomes and require more aggressive treatment [14,84,87]. When assessing the clinical benefits of MUA, the patient and surgeon must also weigh the potential complications, which include fracture, wound dehiscence, patellar tendon avulsions, quadriceps strain or rupture, hemarthrosis, heterotopic bone formation, and pulmonary embolism [79,85]. Debridement When previous interventions like an MUA have failed to restore adequate range of motion, or if the patient is more than 3 months post-TKA, arthroscopic or open debridementdalso known as lysis of adhesionsdis typically considered [10,11]. The reported incidence of patients undergoing a debridement after TKA to address limited range of motion is 0.8% [88]. Arthroscopic debridement is a minimally invasive surgical procedure that introduces various cutting or shaving instruments through multiple arthroscopic portals to break up focal and diffuse arthrofibrosis [77]. The focus of the procedure is on the release of adhesions within the suprapatellar pouch, the lateral and medial gutters, and the intercondylar notch [89]. Previous studies have found arthroscopic debridement improved flexion range of motion 24 -34 , extension range of motion 12 -23 , and overall knee range of motion 24 -31 [83,88,90,91]. When arthrofibrosis is severe enough that nonoperative and arthroscopic techniques fail, open debridement is the more invasive alternative [6,10,45,62]. During the open surgery, blunt and sharp tools are used to break up adhesions with enhanced visualization and easier access to all the articular structures that require debridement [62]. Improvement in overall knee range of motion range averaged 39 with the open method [13,83,92e94]. Because the gains in range of motion for both arthroscopic and open debridement are comparable with those from an MUA, the utility of debridement (specifically open) may only exist for those patients with severe arthrofibrosis and who have not responded to any previous treatments [6]. A recent survey of 82 surgeons found that a majority (55%) do not perform open or arthroscopic debridement, and only 4% routinely performed debridement [5]. Although debridement is generally a safe treatment modality, the risks associated with it include damage to the metal prosthesis, hemarthrosis, extensor mechanism injury, fracture, infection, and neurovascular injury [77]. V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 Revision TKA Revision TKA is the final treatment option available for persistent limited motion if all previous treatments have failed. Previous research has found that 10% of all revisions within 5 years of initial surgery are due to arthrofibrosis [37]. A revision involves a partial or complete replacement of the original prosthesis. Previous literature is scant on the outcomes of revision surgery for arthrofibrosis, but Ries et al did find an improvement in range of motion in 6 patients, averaging a 50 increase in total knee range of motion [14,95]. Unfortunately, pain and function scores after revision TKA for arthrofibrosis have been shown to still lag behind scores for revision TKA for other reasons (eg, infection, instability, wear, and loosening) [96]. Arthrofibrosis may still occur after a revision due to the surgical trauma, postsurgical rehabilitation process, or patient predisposition, as those patients who require a revision due to arthrofibrosis are also those with the highest risk for the persistent development of severe fibrosis. Kim et al [57] found that over 25% of revision TKAs due to stiffness required a second revision. Greidanus et al [97] asserted that “most revision patients will never experience an outcome as favorable as their primary procedure.” The additional risks associated with a revision are similar for primary TKA surgery and as mentioned previously, including infection, hemarthrosis, and neurovascular injury [98]. Future Directions Novel Treatments Novel operative and nonoperative treatment options for arthrofibrosis after TKA are being developed, although most still require larger, prospective, randomized studies. Saltzman et al [99] has described supplementing arthroscopic debridement with the use of indwelling epidural catheters begun preoperatively that continue postoperatively for 6 weeks. The rational for extended pain analgesia is that inadequate postoperative pain control prevents knee flexion, resulting in adhesion formation and knee stiffness [5]. Although the retrospective analysis was completed on a small cohort (n ¼ 20), those receiving epidural catheters showed improved knee extension, knee flexion, and self-reported pain levels, with 70% maintaining range of motion success long-term (6-month follow-up) and minimal complications [99]. Formby et al [100] used hydraulic distension, a technique typically used to treat adhesive capsulitis, as a substitute for an MUA. Hydraulic distension of the knee involves (1) aspirating the suprapatellar pouch, (2) distending the capsule with irrigation fluid and anesthesia until rupture, (3) aspirating the distension fluid, and (4) injecting corticosteroid coupled with manipulation of the knee. The 3 patients receiving hydraulic distension showed a 23 increase in knee flexion postoperatively, which was maintained at follow-up (average 12 months) with no complications [100]. Smith et al [101] performed a prospective, randomized, doubleblinded, placebo-controlled trial comparing the use of botulinum toxin A vs placebo for the treatment of knee flexion contracture after TKA in patients without a specific preexisting neuromuscular disorder. The authors postulated that botulinum toxin A can been used to relieve hamstring tightness that developed secondary to a flexion contracture. The results for 15 knees were that a single injection into the hamstring musculature resulted in a significant improvement in extension at 1 month and a greater amount of improvement at 1 year compared with placebo, although both groups recovered near full extension at the 1-year time point [101]. Treatment options are targeting inhibition of the fibrotic process as well: Farid et al evaluated low-dose irradiation immediately before constrained revision TKA to suppress fibroblastic proliferation; 2609 Dixon et al hypothesize an interleukin-1 receptor antagonist, anakinra, can have an inhibitory effect on fibroblasts; and animal models reveal novel anti-inflammatory agents may reduce knee stiffness [102e104]. These studies serve as impetus for further work into interventions during all perioperative phases of TKA. Screening Certain individuals may develop arthrofibrosis as part of their healing process, indicative of a genetic component to arthrofibrosis [26,105]. The development of an assessment of patient susceptibility to arthrofibrosis would aid healthcare professionals in optimizing perioperative care, targeting those at high risk of complication. For example, a physical therapist could tailor the rehabilitation program more effectively through improving timing, level of aggressiveness, and speed of progression based on the patient's risk level, resulting in faster recovery and better functional outcomes. Differences in genetic disposition and gene expression between patients with and without arthrofibrosis is a promising area of future study. The genetic targets of interest would be those genes and signaling pathway regulators that relate most to the fibrogenic process, capsular remodeling, and long-term inflammatory reactions, all associated with changes in extracellular matrix and collagen production [25,27]. Although allelic association studies have implicated a genetic predisposition toward forming excessive joint scar tissue after injury and/or surgery, a genome-wide association study (GWAS) would offer a far more robust approach for establishing a genetic risk profile [24,25,106]. A GWAS takes into account the entire genome, unbiased with respect to selecting certain single nucleotide polymorphisms. A meta-analysis of multiple GWAS could identify target single nucleotide polymorphisms associated with arthrofibrosis and better inform future candidate gene studies. Determining the genetic variation and what is differentially expressed in those with postoperative arthrofibrosis could then be applied preoperatively through a screening tool to determine patient risk. This knowledge would guide the health care professionals in modifying the timing and aggressiveness of noninvasive postoperative care before the rapid formation of scar tissue, and ideally prevent the need for invasive procedures such as arthroscopic/open arthrolysis or revision TKA in the future. Identification of those individuals at high risk for severe arthrofibrosis could even become a contraindication to receiving a primary TKA. Conclusion Arthrofibrosis is a multi-faceted complication of TKA, and is difficult to treat without an early, tailored, comprehensive rehabilitation program. Understanding the risk factors for its development, as well as the benefits and shortcomings of various interventions are essential to best restore mobility and function (Fig. 1). Future studies investigating early diagnosis and potential preoperative screening for risk of arthrofibrosis will help target those patients who will need additional attention to prevent prolonged, expensive healthcare costs. References [1] Sanders T, Kremers H, Bryan A, Kremers W, Stuart M, Krych A. Procedural intervention for arthrofibrosis after ACL reconstruction: trends over two decades. Knee Surg Sports Traumatol Arthrosc 2015:1e6. http://dx.doi.org/ 10.1007/s00167-015-3799-x. [2] Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty 2007;22:33e8. http://dx.doi.org/10.1016/j.arth.2007.03.034. 2610 V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 [3] Vezeridis PS, Goel DP, Shah AA, Sung S-Y, Warner JJP. Postarthroscopic arthrofibrosis of the shoulder. Sports Med Arthrosc 2010;18:198e206. http://dx.doi.org/10.1097/JSA.0b013e3181ec84a5. [4] Donaldson JR, Tudor F, Gollish J. Revision surgery for the stiff total knee arthroplasty. Bone Joint J 2016;98-B:622e7. [5] Vun SH, Shields DW, Sen A, Shareef S, Sinha S, Campbell AC. A national questionnaire survey on knee manipulation following total knee arthroplasty. J Orthop 2015;12:193e6. http://dx.doi.org/10.1016/j.jor.2015.05.016. [6] Manrique J, Gomez MM, Parvizi J. Stiffness after total knee arthroplasty. J Knee Surg 2015;28:119e26. http://dx.doi.org/10.1055/s-0034-1396079. [7] Solanki RB, Bhise AR. Arthrofibrosis following total knee arthroplasty. Int J Physiother Res 2014;2:762e5. http://dx.doi.org/10.16965/ijpr.2014.686. [8] Millett PJ, Johnson B, Carlson J, Krishnan S, Steadman JR. Rehabilitation of the arthrofibrotic knee. Am J Orthop (Belle Mead NJ) 2003;32:531e8. [9] Magit D, Wolff A, Sutton K, Medvecky MJ. Arthrofibrosis of the knee. J Am Acad Orthop Surg 2007;15:682e94. [10] Kalson NS, Borthwick LA, Mann DA, Deehan DJ, Lewis P, Mann C, et al. International consensus on the definition and classification of fibrosis of the knee joint. Bone Joint J 2016;98-B:1479e88. [11] Bong MR, Di Cesare PE. Stiffness after total knee arthroplasty. J Am Acad Orthop Surg 2004;12:164e71. [12] Christensen CP, Crawford JJ, Olin MD, Vail TP. Revision of the stiff total knee arthroplasty. J Arthroplasty 2002;17:409e15. http://dx.doi.org/10.1054/ arth.2002.32105. [13] Yercan HS, Sugun TS, Bussiere C, Ait Si Selmi T, Davies A, Neyret P. Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee 2006;13:111e7. http://dx.doi.org/10.1016/j.knee.2005.10.001. [14] Kim J, Nelson CL, Lotke PA. Stiffness after total knee arthroplasty. Prevalence of the complication and outcomes of revision. J Bone Joint Surg Am 2004;86A:1479e84. http://dx.doi.org/10.1016/j.arth.2004.02.008. [15] Linklater J, Fessa C. Imaging findings in arthrofibrosis of the ankle and foot. Semin Musculoskelet Radiol 2012;1:185e91. http://dx.doi.org/10.1055/s0032-1320059. C, Velleman M, Suleman FE. MRI findings of cyclops lesions of the [16] Minne knee. SA Orthop J 2012;11:56e60. [17] Devu S, M UM, Rajani S, Marda SS, Mvr S, Devu S. Cyclops - the giant in postoperative knee. Innov J Med Heal Sci 2014;4:298e300. [18] Talbot BS, Weinberg EP. MR imaging with metal-suppression sequences for evaluation of total joint arthroplasty. Radiographics 2015;36:209e25. http:// dx.doi.org/10.1148/rg.2016150075. [19] Sneag DB, Bogner EA. Magnetic resonance imaging evaluation of the painful total knee arthroplasty. Semin Musculoskelet Radiol 2015;19:40e8. [20] Scuderi GR. Techniques in revision hip and knee arthroplasty: expert consult. Philadelphia, PA: Elsevier Saunders; 2014. [21] Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today-has anything changed after 10 years? J Arthroplasty 2014;29:1774e8. http://dx.doi.org/10.1016/j.arth.2013.07.024. [22] Stephenson JJ, Quimbo RA, Gu T. Knee-attributable medical costs and risk of re-surgery among patients utilizing non-surgical treatment options for knee arthrofibrosis in a managed care population. Curr Med Res Opin 2010;26: 1109e18. http://dx.doi.org/10.1185/03007991003676479. [23] Haller JM, Holt DC, Mcfadden ML, Higgins TF, Kubiak EN, Mcfadden ML. Arthrofibrosis of the knee following a fracture of the tibial plateau. Bone Joint J 2015;9797:109e14. http://dx.doi.org/10.1302/0301-620X.97B1. [24] Campbell TM, Trudel G, Wong KK, Laneuville O. Genome wide gene expression analysis of the posterior capsule in patients with osteoarthritis and knee flexion contracture. J Rheumatol 2014;41:2232e9. http:// dx.doi.org/10.3899/jrheum.140079. [25] Hold GL, Untiveros P, Saunders KA, El-Omar EM. Role of host genetics in fibrosis. Fibrogenesis Tissue Repair 2009;2:6. http://dx.doi.org/10.1186/ 1755-1536-2-6. [26] Su EP, Su SL. The stiff total knee replacement: evaluation and treatment. Semin Arthroplasty 2013;24:142e8. http://dx.doi.org/10.1053/j.sart.2013.08.007. [27] Gillespie MJ, Friedland J, Dehaven KE. Arthrofibrosis: etiology, classification, histopathology, and treatment. Oper Tech Sports Med 1998;6:102e10. http://dx.doi.org/10.1016/S1060-1872(98)80057-9. [28] Remst DFG, Blaney Davidson EN, Vitters EL, Blom AB, Stoop R, Snabel JM, et al. Osteoarthritis-related fibrosis is associated with both elevated pyridinoline cross-link formation and lysyl hydroxylase 2b expression. Osteoarthritis Cartilage 2013;21:157e64. http://dx.doi.org/10.1016/ j.joca.2012.10.002. [29] Watson RS, Gouze E, Levings PP, Bush ML, Kay JD, Jorgensen MS, et al. Gene delivery of TGF-beta1 induces arthrofibrosis and chondrometaplasia of synovium in vivo. Lab Invest 2010;90:1615e27. http://dx.doi.org/10.1038/ labinvest.2010.145. [30] Freeman TA, Parvizi J, Della Valle CJ, Steinbeck MJ. Reactive oxygen and nitrogen species induce protein and DNA modifications driving arthrofibrosis following total knee arthroplasty. Fibrogenesis Tissue Repair 2009;2:5. http://dx.doi.org/10.1186/1755-1536-2-5. [31] Faust I, Traut P, Nolting F, Petschallies J, Neumann E, Kunisch E, et al. Human xylosyltransferasesemediators of arthrofibrosis? New pathomechanistic insights into arthrofibrotic remodeling after knee replacement therapy. Sci Rep 2015;5:12537. http://dx.doi.org/10.1038/srep12537. [32] Pfitzner T, Geissler S, Duda G, Perka C, Matziolis G. Increased BMP expression in arthrofibrosis after TKA. Knee Surg Sports Traumatol Arthrosc 2012;20: 1803e8. http://dx.doi.org/10.1007/s00167-011-1774-8. € tting C, Kuhn J, Kleesiek K. Human xylosyltransferases in health and dis[33] Go ease. Cell Mol Life Sci 2007;64:1498e517. http://dx.doi.org/10.1007/s00018007-7069-z. [34] Black DW. Treatment of knee arthrofibrosis and quadriceps insufficiency after patellar tendon repair: a case report including use of the graston technique. Int J Ther Massage Bodywork 2010;3:14e21. http://dx.doi.org/ 10.3822/ijtmb.v3i2.79. [35] Rissman CM, Keeney BJ, Ercolano EM, Koenig KM. Predictors of facility discharge, range of motion, and patient-reported physical function improvement after primary total knee arthroplasty: a prospective cohort analysis. J Arthroplasty 2016;31:36e41. http://dx.doi.org/10.1016/j.arth.2015.09.002. [36] Desai AS, Karmegam A, Dramis A, Board TN, Raut V. Manipulation for stiffness following total knee arthroplasty: when and how often to do it? Eur J Orthop Surg Traumatol 2014;24:1291e5. http://dx.doi.org/10.1007/s00590013-1387-7. [37] Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty 2013;28:116e9. http://dx.doi.org/10.1016/ j.arth.2013.04.056. [38] Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res 2014;472: 181e7. http://dx.doi.org/10.1007/s11999-013-3030-7. [39] Bonutti PM, Marulanda GA, McGrath MS, Mont MA, Zywiel MG. Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2010;18:194e9. http://dx.doi.org/10.1007/s00167-009-0947-1. [40] Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780e5. http://dx.doi.org/10.2106/JBJS.F.00222. [41] Seyler TM, Marker DR, Bhave A, Plate JF, Marulanda GA, Bonutti PM, et al. Functional problems and arthrofibrosis following total knee arthroplasty. J Bone Joint Surg Am 2007;89(Suppl 3):59e69. http://dx.doi.org/10.2106/ JBJS.G.00457. [42] Bhave A, Mont M, Tennis S, Nickey M, Starr R, Etienne G. Functional problems and treatment solutions after total hip and knee joint arthroplasty. J Bone Joint Surg Am 2005;87(Suppl 2):9e21. http://dx.doi.org/10.2106/JBJS.E.00628. [43] Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther 1972;52:34e43. [44] Unterhauser FN, Bosch U, Zeichen J, Weiler A. Alpha-smooth muscle actin containing contractile fibroblastic cells in human knee arthrofibrosis tissue. Arch Orthop Trauma Surg 2004;124:5855e91. http://dx.doi.org/10.1007/ s00402-004-0742-x. [45] Creighton RA, Bach BR. Arthrofibrosis: evaluation, prevention, and treatment. Tech Knee Surg 2005;4:163e72. http://dx.doi.org/10.1097/ 01.btk.0000175762.33382.e0. [46] Perry J, Antonelli D, Ford W. Analysis of knee-joint forces during flexed-knee stance. J Bone Joint Surg Am 1975;57:961e7. [47] Pfefferle KJ, Shemory ST, Dilisio MF, Fening SD, Gradisar IM. Risk factors for manipulation after total knee arthroplasty: a pooled electronic health record database study. J Arthroplasty 2014;29:2036e8. http://dx.doi.org/10.1016/ j.arth.2014.05.001. [48] Namba RS, Inacio M. Early and late manipulation improve flexion after total knee arthroplasty. J Arthroplasty 2007;22:58e61. http://dx.doi.org/10.1016/ j.arth.2007.02.010. [49] Bozic KJ, Kamath AF, Ong K, Lau E, Kurtz S, Chan V, et al. Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res 2015;473:2131e8. http://dx.doi.org/10.1007/s11999-014-4078-8. [50] Burns AWR, Bourne RB, Chesworth BM, MacDonald SJ, Rorabeck CH. Cost effectiveness of revision total knee arthroplasty. Clin Orthop Relat Res 2006;446:29e33. http://dx.doi.org/10.1097/01.blo.0000214420.14088.76. [51] Vincent KR, Vincent HK, Lee LW, Alfano AP. Inpatient rehabilitation outcomes in primary and revision total knee arthroplasty patients. Clin Orthop Relat Res 2006;446:201e7. http://dx.doi.org/10.1097/01.blo.0000214435.72398.0e. [52] Maradit Kremers H, Visscher SL, Moriarty JP, Reinalda MS, Kremers WK, Naessens JM, et al. Determinants of direct medical costs in primary and revision total knee arthroplasty knee. Clin Orthop Relat Res 2013;471: 206e14. http://dx.doi.org/10.1007/s11999-012-2508-z. [53] Graver R, Da Deppo L, Harris E, Feingass S. The total economic cost of primary total joint replacement surgery in the United States. 2010 Annual Meeting of the American Academy of Orthopaedic Surgeons, New Orleans. 2010. [54] Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med 1991;19:332e6. http:// dx.doi.org/10.1177/036354659101900402. [55] Ranawat CS, Ranawat AS, Mehta A. Total knee arthroplasty rehabilitation protocol: what makes the difference? J Arthroplasty 2003;18:27e30. http:// dx.doi.org/10.1054/arth.2003.50080. [56] Westby MD, Brittain A, Backman CL. Expert consensus on best practices for post-acute rehabilitation after total hip and knee arthroplasty: a Canada and V.A. Cheuy et al. / The Journal of Arthroplasty 32 (2017) 2604e2611 [57] [58] [59] [60] [61] [62] [63] [64] [65] [66] [67] [68] [69] [70] [71] [72] [73] [74] [75] [76] [77] [78] [79] [80] [81] United States Delphi study. Arthritis Care Res (Hoboken) 2014;66:411e23. http://dx.doi.org/10.1002/acr.22164. Kim GK, Mortazavi SMJ, Parvizi J, Purtill JJ. Revision for stiffness following TKA: a predictable procedure? Knee 2012;19:332e4. http://dx.doi.org/ 10.1016/j.knee.2011.06.016. Werner BC, Carr JB, Wiggins JC, Gwathmey FW, Browne JA. Manipulation under anesthesia after total knee arthroplasty is associated with an increased incidence of subsequent revision surgery. J Arthroplasty 2015;30:72e5. http://dx.doi.org/10.1016/j.arth.2015.01.061. Livbjerg AE, Froekjaer S, Simonsen O, Rathleff MS. Pre-operative patient education is associated with decreased risk of arthrofibrosis after total knee arthroplasty: a case control study. J Arthroplasty 2013;28:1282e5. http:// dx.doi.org/10.1016/j.arth.2013.01.016. Shoji H, Solomonow M, Yoshino S, D'Ambrosia R, Dabezies E. Factors affecting postoperative flexion in total knee arthroplasty. Orthopedics 1990;13:643e9. Mauerhan DR, Mokris JG, Ly A, Kiebzak GM. Relationship between length of stay and manipulation rate after total knee arthroplasty. J Arthroplasty 1998;13:896e900. http://dx.doi.org/10.1016/S0883-5403(98)90196-6. Millett PJ, Williams RJ, Wickiewicz TL. Open debridement and soft tissue release as a salvage procedure for the severely arthrofibrotic knee. Am J Sports Med 1999;27:552e61. Kim Y-M, Joo YB. Prognostic factors of arthroscopic adhesiolysis for arthrofibrosis of the knee. Knee Surg Relat Res 2013;25:202. http://dx.doi.org/ 10.5792/ksrr.2013.25.4.202. Schiavone Panni A, Cerciello S, Vasso M, Tartarone M. Stiffness in total knee arthroplasty. J Orthop Traumatol 2009;10:111e8. http://dx.doi.org/10.1007/ s10195-009-0054-6. Pope RO, Corcoran S, McCaul K, Howie DW. Continuous passive motion after primary total knee arthroplasty. Does it offer any benefits? J Bone Joint Surg Br 1997;79:914e7. LA, Davies DM, Jones CA, Cinats JG. Exercise combined with Beaupre continuous passive motion or slider board therapy compared with exercise only: a randomized controlled trial of patients following total knee arthroplasty. Phys Ther 2001;81:1029e37. Joshi RN, White PB, Murray-Weir M, Alexiades MM, Sculco TP, Ranawat AS. Prospective randomized trial of the efficacy of continuous passive motion post total knee arthroplasty: experience of the hospital for special surgery. J Arthroplasty 2015;30:2364e9. http://dx.doi.org/10.1016/j.arth.2015.06.006. Boese CK, Weis M, Phillips T, Lawton-Peters S, Gallo T, Centeno L. The efficacy of continuous passive motion after total knee arthroplasty: a comparison of three protocols. J Arthroplasty 2014;29:1158e62. http://dx.doi.org/10.1016/ j.arth.2013.12.005. Wright RW, Fetzer GB. Bracing after ACL reconstruction: a systematic review. Clin Orthop Relat Res 2007;455:162e8. http://dx.doi.org/10.1097/ BLO.0b013e31802c9360. Azim K, Parsley B, Brinker M. Chronic patellar tendon rupture and arthrofibrosis after total knee arthroplasty. Curr Orthop Pract 2015;26:204e7. McGrath MS, Mont MA, Siddiqui JA, Baker E, Bhave A. Evaluation of a custom device for the treatment of flexion contractures after total knee arthroplasty. Clin Orthop Relat Res 2009;467:1485e92. http://dx.doi.org/10.1007/s11999009-0804-z. Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther 2012;92: 210e26. http://dx.doi.org/10.2522/ptj.20110124. Bade MJ, Stevens-Lapsley JE. Restoration of physical function in patients following total knee arthroplasty: an update on rehabilitation practices. Curr Opin Rheumatol 2012;24:208e14. http://dx.doi.org/10.1097/BOR.0b0 13e32834ff26d. Chughtai M, Mont MA, Cherian C, Cherian JJ, Elmallah RDK, Naziri Q, et al. A novel, nonoperative treatment demonstrates success for stiff total knee arthroplasty after failure of conventional therapy. J Knee Surg 2016;29: 188e93. http://dx.doi.org/10.1055/s-0035-1569482. Bawa HS, Wera GD, Kraay MJ, Marcus RE, Goldberg VM. Predictors of range of motion in patients undergoing manipulation after TKA knee. Clin Orthop Relat Res 2013;471:258e63. http://dx.doi.org/10.1007/s11999-012-2591-1. Cates HE, Schmidt JM. Closed manipulation after total knee arthroplasty: outcome and affecting variables. Orthopedics 2009;32:398. http://dx.doi.org/ 10.3928/01477447-20090511-10. Enad JG. Arthroscopic lysis of adhesions for the stiff total knee arthroplasty. Arthrosc Tech 2014;3:e611e4. http://dx.doi.org/10.1016/j.eats.2014.07.001. Issa K, Kapadia BH, Kester M, Khanuja HS, Delanois RE, Mont MA. Clinical, objective, and functional outcomes of manipulation under anesthesia to treat knee stiffness following total knee arthroplasty. J Arthroplasty 2014;29: 548e52. http://dx.doi.org/10.1016/j.arth.2013.07.046. Mohammed R, Syed S, Ahmed N. Manipulation under anaesthesia for stiffness following knee arthroplasty. Ann R Coll Surg Engl 2009;91:220e3. http://dx.doi.org/10.1308/003588409X359321. Fitzsimmons SE, Vazquez EA, Bronson MJ. How to treat the stiff total knee arthroplasty?: A systematic review. Clin Orthop Relat Res 2010;468: 1096e106. http://dx.doi.org/10.1007/s11999-010-1230-y. €fer R, Lahrmann J, Kluba T. Stiffness after knee arthrotomy: Ipach I, Scha evaluation of prevalence and results after manipulation under anaesthesia. [82] [83] [84] [85] [86] [87] [88] [89] [90] [91] [92] [93] [94] [95] [96] [97] [98] [99] [100] [101] [102] [103] [104] [105] [106] 2611 Orthop Traumatol Surg Res 2011;97:292e6. http://dx.doi.org/10.1016/ j.otsr.2011.01.006. Keating EM, Ritter MA, Harty LD, Haas G, Meding JB, Faris PM, et al. Manipulation after total knee arthroplasty. J Bone Joint Surg Am 2007;89: 282e6. http://dx.doi.org/10.2106/JBJS.E.00205. Scranton PE. Management of knee pain and stiffness after total knee arthroplasty. J Arthroplasty 2001;16:428e35. http://dx.doi.org/10.1054/ arth.2001.22250. Ipach I, Mittag F, Lahrmann J, Kunze B, Kluba T. Arthrofibrosis after TKA influence factors on the absolute flexion and gain in flexion after manipulation under anaesthesia. BMC Musculoskelet Disord 2011;12:184. http:// dx.doi.org/10.1186/1471-2474-12-184. Pariente GM, Lombardi AV, Berend KR, Mallory TH, Adams JB. Manipulation with prolonged epidural analgesia for treatment of TKA complicated by arthrofibrosis. Surg Technol Int 2006;15:221e4. Issa K, Banerjee S, Kester MA, Khanuja HS, Delanois RE, Mont MA. The effect of timing of manipulation under anesthesia to improve range of motion and functional outcomes following total knee arthroplasty. J Bone Joint Surg Am 2014;96:1349e57. http://dx.doi.org/10.2106/JBJS.M.00899. Choi HR, Siliski JM, Malchau H, Kwon YM. Effect of repeated manipulation on range of motion in patients with stiff total knee arthroplasty. Orthopedics 2015;38:e157e62. Tjoumakaris FP, Tucker BS, Post Z, Pepe MD, Orozco F, Ong AC. Arthroscopic lysis of adhesions for the stiff total knee: results after failed manipulation. Orthopedics 2014;37:e482e7. Hegazy AM, Elsoufy MA. Arthroscopic arthrolysis for arthrofibrosis of the knee after total knee replacement. HSS J 2011;7:130e3. http://dx.doi.org/ 10.1007/s11420-011-9202-7. Jerosch J, Aldawoudy AM. Arthroscopic treatment of patients with moderate arthrofibrosis after total knee replacement. Knee Surg Sports Traumatol Arthrosc 2007;15:71e7. http://dx.doi.org/10.1007/s00167-006-0099-5. Schwarzkopf R, William A, Deering RM, Fitz W. Arthroscopic lysis of adhesions for stiff total knee arthroplasty. Orthopedics 2013;36:e1544e8. Hutchinson JRM, Parish EN, Cross MJ. Results of open arthrolysis for the treatment of stiffness after total knee replacement. Bone Joint J 2005;87: 1357e60. Mont MA, Seyler TM, Marulanda GA, Delanois RE, Bhave A. Surgical treatment and customized rehabilitation for stiff knee arthroplasties. Clin Orthop Relat Res 2006;446:193e200. Babis GC, Trousdale RT, Pagnano MW, Morrey BF. Poor outcomes of isolated tibial insert exchange and arthrolysis for the management of stiffness following total knee arthroplasty. J Bone Joint Surg Am 2001;83:1534e6. Ries MD, Badalamente M. Arthrofibrosis after total knee arthroplasty. Clin Orthop Relat Res 2000:177e83. Pun SY, Ries MD. Effect of gender and preoperative diagnosis on results of revision total knee arthroplasty. Clin Orthop Relat Res 2008;466:2701e5. http://dx.doi.org/10.1007/s11999-008-0451-9. Greidanus NV, Peterson RC, Masri BA, Garbuz DS. Quality of life outcomes in revision versus primary total knee arthroplasty. J Arthroplasty 2011;26: 615e20. http://dx.doi.org/10.1016/j.arth.2010.04.026. Mortazavi SMJ, Schwartzenberger J, Austin MS, Purtill JJ, Parvizi J. Revision total knee arthroplasty infection: incidence and predictors. Clin Orthop Relat Res 2010;468:2052e9. http://dx.doi.org/10.1007/s11999-010-1308-6. Saltzman BM, Dave A, Young A, Ahuja M, Amin SD, Bush-Joseph CA. Prolonged epidural infusion improves functional outcomes following knee arthroscopy in patients with arthrofibrosis after total knee arthroplasty: a retrospective evaluation. J Knee Surg 2016;29:40e6. http://dx.doi.org/ 10.1055/s-0034-1394163. Formby PM, Donohue MA, Cannova CJ, Caulfield JP. Hydraulic distension of the knee: a novel treatment for arthrofibrosis after total knee replacement (case series). ANZ J Surg 2016;86:480e2. http://dx.doi.org/10.1111/ ans.13540. Smith EB, Shafi KA, Greis AC, Maltenfort MG, Chen AF. Decreased flexion contracture after total knee arthroplasty using Botulinum toxin A: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 2016;24: 3229e34. http://dx.doi.org/10.1007/s00167-016-4277-9. Farid YR, Thakral R, Finn HA. Low-dose irradiation and constrained revision for severe, idiopathic, arthrofibrosis following total knee arthroplasty. J Arthroplasty 2013;28:1314e20. http://dx.doi.org/10.1016/j.arth.2012.11.009. Dixon D, Coates J, del Carpio Pons A, Horabin J, Walker A, Abdul N, et al. A potential mode of action for Anakinra in patients with arthrofibrosis following total knee arthroplasty. Sci Rep 2015;5:16466. http://dx.doi.org/ 10.1038/srep16466. Efird W, Kellam P, Yeazell S, Weinhold P, Dahners LE. An evaluation of prophylactic treatments to prevent post traumatic joint stiffness. J Orthop Res 2014;32:1520e4. http://dx.doi.org/10.1002/jor.22700. Parvizi J, Tarity T, Steinbeck MJ, Politi R, Joshi A, Purtill J, et al. Management of stiffness following total knee arthroplasty. J Bone Joint Surg Am 2006;88A:175e81. Skutek M, Elsner H-A, Slateva K, Mayr H-O, Weig T-G, van Griensven M, et al. Screening for arthrofibrosis after anterior cruciate ligament reconstruction: analysis of association with human leukocyte antigen. Arthrosc J Arthrosc Relat Surg 2004;20:469e73. http://dx.doi.org/10.1016/j. arthro.2004.03.003.