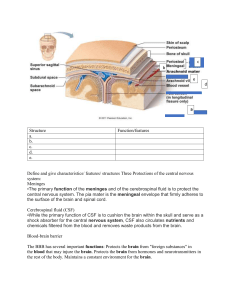
The nervous system is one of the most complex systems. It controls all the body’s activities. Having a general understanding of the nervous system is critical to your being able to analyze and interpret clinical findings. This chapter reviews the structures and functions, assessment, and diagnostic studies of the nervous system. Structures and Functions of Nervous System The nervous system is responsible for the control and integration of the body’s many activities. It is divided into the central nervous system and peripheral nervous system. The central nervous system (CNS) consists of the brain, spinal cord, and cranial nerves I and II. The peripheral nervous system (PNS) consists of cranial nerves III to XII, spinal nerves, and peripheral components of the autonomic nervous system (ANS). Cells of Nervous System The nervous system is made up of 2 types of cells: neurons and supportive glial cells. Neurons Neurons are the primary functional unit of the nervous system. Although neurons come in many shapes and sizes, they share 3 characteristics: (1) excitability, or the ability to generate a nerve impulse; (2) conductivity, or the ability to transmit an impulse; and (3) influence, or the ability to influence other neurons, muscle cells, or glandular cells. A typical neuron consists of a cell body, multiple dendrites, and an axon (Fig. 55.1). The cell body contains the nucleus and cytoplasm. It is the metabolic center of the neuron. Dendrites are short processes extending from the cell body. They receive impulses or signals from other neurons and conduct them toward the cell body. The axon projects varying distances from the cell body. The axon carries nerve impulses to other neurons or to end organs, such as smooth and striated muscles and glands. FIG. 55.1 Structural features of neurons: dendrites, cell body, and axons. Modified from Thibodeau GA, Patton KT: Anatomy and physiology, ed 8, St Louis, 2013, Mosby. Many axons in the CNS and PNS are covered by a myelin sheath, a white, lipid protein substance that acts as an insulator for the conduction of impulses. Axons may be myelinated or unmyelinated, as in the case of smaller fibers. Glial Cells Glial cells (glia or neuroglia) provide support, nourishment, and protection to neurons. Glial cells make up about half of the brain and spinal cord mass. Glial cells are divided into microglia and macroglia. Microglia, specialized macrophages capable of phagocytosis, protect the neurons. These cells are mobile within the brain and multiply when the brain is damaged. Macroglial cells include astrocytes, oligodendrocytes, and ependymal cells. Astrocytes are found mainly in gray matter. They provide structural support to neurons. Their delicate processes form the blood-brain barrier with the endothelium of the blood vessels. They also play a role in synaptic transmission (conduction of impulses between neurons). When the brain is injured, astrocytes act as phagocytes for cleaning up neuronal debris. They help restore the neurochemical milieu and provide support for repair. Proliferation of astrocytes contributes to the formation of scar tissue (gliosis) in the CNS. Oligodendrocytes are specialized cells that produce the myelin sheath of nerve fibers in the CNS. They are found mainly in the white matter of the CNS. Ependymal cells line the brain ventricles and aid in the secretion of cerebrospinal fluid (CSF). Neuroglia are mitotic and can replicate. In general, when neurons are destroyed, the tissue is replaced by the proliferation of neuroglial cells. Most primary CNS tumors involve glial cells. Primary cancers involving neurons are rare. Nerve Regeneration If the axon of the nerve cell is damaged, the cell tries to repair itself. Damaged nerve cells try to grow back to their original destinations by sprouting many branches from the damaged ends of their axons. Axons in the CNS are generally less successful than peripheral axons in regeneration.1 Schwann cells myelinate the nerve fibers in the PNS. Injured nerve fibers in the PNS can regenerate by growing within the protective myelin sheath of the Schwann cells if the cell body is intact and the environment is optimal.2 The final result of nerve regeneration depends on the number of axon sprouts that join with the appropriate Schwann cell columns and reinnervate appropriate end organs. Neurons have long been thought to be nonmitotic. That is, after being damaged, neurons could not be replaced. Recent research shows a subset of glial cells (astrocytes) proliferate after certain injuries in the CNS, and neurogenesis may occur from stem cells.3 These findings support the expectation that the patient will have a certain amount of recovery after injury involving the neurons. Nerve Impulse The purpose of a neuron is to initiate, receive, and process messages about events both within and outside the body. The initiation of a neuronal message (nerve impulse) involves the generation of an action potential. A series of action potentials travel along the axon. When the impulse reaches the end of the nerve fiber, a chemical interaction involving neurotransmitters transmits the impulse across the junction (synapse) between nerve cells by. This chemical interaction generates another set of action potentials in the next neuron. These events are repeated until the nerve impulse reaches its destination. Because of its insulating capacity, myelination of nerve axons speeds the conduction of an action potential. Many peripheral nerve axons have nodes of Ranvier (gaps in the myelin sheath) that allow an action potential to travel much faster by jumping from node to node. We call this saltatory (hopping) conduction. In an unmyelinated fiber, conduction is slower. The wave of depolarization travels the entire length of the axon, with each part of the membrane becoming depolarized in turn. Synapse A synapse is the structural and functional junction between 2 neurons. It is where the nerve impulse is transmitted from 1 neuron to another. The nerve impulse also can be transmitted from neurons to glands or muscles. The essential structures of synaptic transmission are a presynaptic terminal, synaptic cleft, and receptor site on the postsynaptic cell (Fig. 55.2). Neurotransmitters Neurotransmitters are chemicals that affect the transmission of impulses across the synaptic cleft. Excitatory neurotransmitters (e.g., epinephrine, norepinephrine, glutamate) activate postsynaptic receptors that increase the chance that an action potential will be generated. Inhibitory neurotransmitters (e.g., serotonin, γ-aminobutyric acid [GABA], dopamine) activate postsynaptic receptors to decrease the chance that an action potential will be generated. For example, endorphins block pain transmission while substance P makes nerves more sensitive to pain. FIG. 55.2 Impulse generation between neurons. Synapse shown with neurotransmitters and receptors. In general, the net effect (excitatory or inhibitory) depends on the number of presynaptic neurons releasing neurotransmitters on the postsynaptic cell. A presynaptic cell that releases an excitatory neurotransmitter does not always cause the postsynaptic cell to depolarize enough to generate an action potential. When many presynaptic cells release excitatory neurotransmitters on a single neuron, the sum of their input is enough to generate an action potential. Neurotransmitters continue to combine with the receptor sites at the postsynaptic membrane until they are inactivated by enzymes, are taken up by the presynaptic endings, or diffuse away from the synaptic region. Drugs and toxins can affect neurotransmitters by changing their function or blocking their attachment to receptor sites on the postsynaptic membrane. We can use cerebral microdialysis to measure neurotransmitter levels in the cerebral cortex (see Chapter 56). Central Nervous System The components of the CNS include the cerebrum (cerebral hemispheres), brainstem, cerebellum, and spinal cord. Spinal Cord The spinal cord is continuous with the brainstem and exits from the cranial cavity through the foramen magnum. A cross section of the spinal cord reveals gray matter that is centrally located in an H shape and surrounded by white matter. The gray matter contains the cell bodies of voluntary motor neurons, preganglionic autonomic motor neurons, and association neurons (interneurons). The white matter contains the axons of the ascending sensory and descending motor fibers. The myelin surrounding these fibers gives them their white appearance. The spinal pathways or tracts are named for the point of origin and the point of destination (e.g., spinocerebellar tract [ascending], corticospinal tract [descending]). Ascending Tracts In general, the ascending tracts carry specific sensory information to higher levels of the CNS. This information comes from special sensory receptors in the skin, muscles and joints, viscera, and blood vessels and enters the spinal cord by way of the dorsal roots of the spinal nerves. The ascending tracts are organized by sensory modality and anatomy. The fasciculus gracilis and the fasciculus cuneatus (often called the dorsal or posterior columns) carry information about touch, deep pressure, vibration, position sense, and kinesthesia (appreciation of movement, weight, and body parts). The spinocerebellar tracts carry information about muscle tension and body position to the cerebellum for coordination of movement. The spinothalamic tracts carry pain and temperature sensations. Other ascending tracts may also carry sensory modalities. The signs and symptoms of various neurologic diseases suggest there are additional pathways for touch, position sense, and vibration. Descending Tracts Descending tracts carry impulses that are responsible for muscle movement. Among the most important descending tracts are the corticobulbar and corticospinal tracts, collectively termed the pyramidal tract. These tracts carry voluntary impulses from the cerebral cortex to the cranial and peripheral nerves. Another group of descending motor tracts carries impulses from the extrapyramidal system (all motor systems except the pyramidal) concerned with voluntary movement. It includes pathways originating in the brainstem, basal ganglia, and cerebellum. The motor output exits the spinal cord by way of the ventral roots of the spinal nerves. Reflex Arc A reflex is an involuntary response to stimuli. In the spinal cord, reflex arcs play an important role in maintaining muscle tone, which is essential for body posture. The components of a monosynaptic reflex arc (Fig. 55.3) are a receptor organ, afferent neuron, effector neuron, and effector organ (e.g., skeletal muscle). The afferent neuron synapses with the efferent neurons in the gray matter of the spinal cord. More complex reflex arcs have other neurons (interneurons) in addition to the afferent neuron influencing the effector neuron. Lower and Upper Motor Neurons Upper motor neurons (UMNs) originate in the cerebral cortex and project downward. The corticobulbar tract ends in the brainstem, and the corticospinal tract descends into the spinal cord. These neurons influence skeletal muscle movement. UMN lesions generally cause weakness or paralysis, disuse atrophy, hyperreflexia, and increased muscle tone (spasticity). Lower motor neurons (LMNs) are the final common pathway through which descending motor tracts influence skeletal muscle. The cell bodies of LMNs, which send axons to innervate the skeletal muscles of the arms, trunk, and legs, are found in the anterior horn of the corresponding segments of the spinal cord (e.g., cervical segments contain LMNs for the arms). LMNs for skeletal muscles of the eyes, face, mouth, and throat are found in the corresponding segments of the brainstem. These cell bodies and their axons make up the somatic motor components of the cranial nerves. LMN lesions generally cause weakness or paralysis, denervation atrophy, hyporeflexia or areflexia, and decreased muscle tone (flaccidity). Brain The brain has 3 major intracranial components: cerebrum, brainstem, and cerebellum. Cerebrum The cerebrum is composed of the right and left cerebral hemispheres. It is divided into 4 lobes: frontal, temporal, parietal, and occipital (Fig. 55.4). The functions of the cerebrum are multiple and complex (Table 55.1). The frontal lobe controls higher cognitive function, memory retention, voluntary eye movements, voluntary motor movement, and motor functions involved in speech production (Broca’s area). The temporal lobe integrates somatic, visual, and auditory data and contains Wernicke’s receptive speech area. (Language and potential functional deficits are described with strokes in Chapter 57 [see Table 57.4]). The parietal lobe interprets spatial information and contains the sensory cortex. Processing of sight takes place in the occipital lobe. The division of the cerebrum into lobes is useful to delineate portions of the neocortex (gray matter), which makes up the outer layer of the cerebral hemispheres. Neurons in specific parts of the neocortex are essential for various highly complex and sophisticated functions, such as language, memory, and appreciation of visual-spatial relationships. The basal ganglia, thalamus, hypothalamus, and limbic system are also in the cerebrum. The basal ganglia are a group of structures found centrally in the cerebrum and midbrain. Most of them are on both sides of the thalamus. The function of the basal ganglia includes the initiation, execution, and completion of voluntary movements, learning, emotional response, and automatic movements associated with skeletal muscle activity (e.g., swallowing saliva, blinking, swinging the arms while walking). The thalamus lies directly above the brainstem (Fig. 55.5). It is the major relay center for sensory input from the body, face, retina, and cochlear and taste receptors. Motor relay nuclei in the thalamus connect the cerebellum and basal ganglia to the frontal cortex. The hypothalamus is just below the thalamus and slightly in front of the midbrain. It exerts a direct influence on release of hormones from the anterior pituitary gland. It has a rich capillary connection to the pituitary gland to aid in the transport of hormones. These hormones include thyroid- stimulating hormone, growth hormone, luteinizing hormone, and prolactinreleasing hormone, which play a role in regulating reproductive function. In contrast, the supraoptic and paraventricular neurons travel directly through the pituitary stalk to the posterior pituitary, where they release vasopressin and oxytocin. The hypothalamus contains the satiety center that regulates appetite. With input from the limbic system, it also regulates body temperature, water balance (through influence on vasopressin secretion), circadian rhythm, and expression of emotion. The limbic system is found near the inner surfaces of the cerebral hemispheres. It is concerned with emotion, aggression, feeding behavior, and sexual response. Brainstem The brainstem includes the midbrain, pons, and medulla (Fig. 55.5). Ascending and descending fibers to and from the cerebrum and cerebellum pass through the brainstem. The nuclei of cranial nerves III through XII are in the brainstem. The vital centers concerned with respiratory, vasomotor, and heart function are in the medulla. Also in the brainstem is the reticular formation, a diffusely arranged group of neurons and their axons that extends from the medulla to the thalamus and hypothalamus. The functions of the reticular formation include relaying sensory information, influencing excitatory and inhibitory control of spinal motor neurons, and controlling vasomotor and respiratory activity. The reticular activating system (RAS) is a complex system that requires communication among the brainstem, reticular formation, and cerebral cortex. The RAS regulates arousal and sleep-wake transitions. The brainstem also contains the centers for sneezing, coughing, hiccupping, vomiting, sucking, and swallowing. Cerebellum The cerebellum is in the posterior cranial fossa below the occipital lobe. It coordinates voluntary movement and maintains trunk stability and equilibrium. The cerebellum receives information from the cerebral cortex, muscles, joints, and inner ear. It influences motor activity through axonal connections to the thalamus, motor cortex, and brainstem nuclei and their descending pathways. FIG. 55.5 Major divisions of the CNS. Ventricles and Cerebrospinal Fluid The ventricles are 4 interconnected fluid-filled cavities. The lower part of the fourth ventricle becomes the central canal in the lower part of the brainstem. The spinal canal extends centrally through the full length of the spinal cord. Cerebrospinal fluid (CSF) is made largely in the choroid plexuses of the brain within the ventricles. It circulates within the subarachnoid space that surrounds the brain, brainstem, and spinal cord, cushioning the brain and spinal cord. CSF flows from the cranial cavity to the spinal cavity, carrying nutrients through both passive diffusion and active transport. We make CSF at an average rate of about 500 mL/day. The ventricles and central canal are filled with an average of 150 mL at any given time. Changes in the rate of CSF production or absorption can occur, leading to a change in the volume within the ventricles and central canal. Excessive buildup of CSF results in a condition known as hydrocephalus. CSF circulates throughout the ventricles and seeps into the subarachnoid space surrounding the brain and spinal cord. It is absorbed primarily through the arachnoid villi (tiny projections into the subarachnoid space) into the intradural venous sinuses and eventually into the venous system. The analysis of CSF composition provides useful diagnostic information related to certain nervous system diseases. We often measure CSF pressure in patients with actual or suspected intracranial injury. Increased intracranial pressure, indicated by increased CSF pressure, can force downward (central) herniation of the brain and brainstem. The signs marking this event are part of the herniation syndrome (see Chapter 56). Peripheral Nervous System The PNS includes all the neuronal structures that lie outside the CNS. It consists of the spinal and cranial nerves, their associated ganglia (groupings of cell bodies), and portions of the ANS. Spinal Nerves The spinal cord can be seen as a series of spinal segments, each on top of another with no visible boundaries. In addition to the cell bodies, each segment has a pair of dorsal (afferent) sensory nerve fibers or roots and ventral (efferent) motor fibers or roots. They innervate a specific region of the body. This combined motor-sensory nerve is called a spinal nerve (Fig. 55.6). The cell bodies of the voluntary motor system are in the anterior horn of the spinal cord gray matter. The cell bodies of the autonomic (involuntary) motor system are in the anterolateral part of the spinal cord gray matter. The cell bodies of sensory fibers are in the dorsal root ganglia just outside the spinal cord. On exiting the spinal column, each spinal nerve divides into ventral and dorsal rami, a collection of motor and sensory fibers that eventually goes to peripheral structures (e.g., skin, muscles, viscera). FIG. 55.6 Cross section of spinal cord showing attachments of spinal nerves and coverings of the spinal cord. A dermatome is the area of skin innervated by the sensory fibers of a single dorsal root of a spinal nerve (Fig. 55.7). The dermatomes give a general picture of somatic sensory innervation by spinal segments. A myotome is a muscle group innervated by the primary motor neurons of a single ventral root. The dermatomes and myotomes of a given spinal segment overlap with those of adjacent segments because of the development of ascending and descending collateral branches of nerve fibers. Cranial Nerves The cranial nerves (CNs) are the 12 paired nerves composed of cell bodies with fibers that exit from the cranial cavity. Unlike the spinal nerves, which always have both afferent sensory and efferent motor fibers, some CNs are only sensory, some only motor, and some both. Table 55.4 (later in this chapter) outlines the motor and sensory components of the CNs. Fig. 55.8 shows the position of the CNs in relation to the brain and spinal cord. Just as the cell bodies of the spinal nerves are found in specific segments of the spinal cord, cell bodies (nuclei) of the CNs found in specific segments of the brainstem. Exceptions are the nuclei of the olfactory and optic nerves. The primary cell bodies of the olfactory nerve are in the nasal epithelium. The cell bodies of the optic nerve are in the retina. Autonomic Nervous System The autonomic nervous system (ANS) is divided into the sympathetic and parasympathetic systems. The ANS governs involuntary functions of heart muscle, smooth muscle, and glands through both efferent and afferent pathways. The 2 systems function together to maintain a relatively balanced internal environment. The preganglionic cell bodies of the sympathetic nervous system (SNS) are found in spinal segments T1 through L2. The major neurotransmitter released by the postganglionic fibers of the SNS is norepinephrine. The neurotransmitter released by the preganglionic fibers is acetylcholine. FIG. 55.7 Dermatomes of the body. From Herlihy B: The human body in health and illness, ed 4, St Louis, 2011, Saunders. The preganglionic cell bodies of the parasympathetic nervous system (PSNS) are found in the brainstem and sacral spinal segments (S2 through S4). Acetylcholine is the neurotransmitter released at both preganglionic and postganglionic nerve endings. SNS stimulation activates the mechanisms required for the “fight-orflight” response that occurs throughout the body (Fig. 55.9). In contrast, the PSNS is geared to act in localized and discrete regions. It conserves and restores the body’s energy stores. The ANS provides dual and often reciprocal innervation to many structures. For example, the SNS increases the rate and force of heart contraction and the PSNS decreases the rate and force. Cerebral Circulation Knowing the distribution of the brain’s major arteries is essential for understanding and evaluating the signs and symptoms of cerebrovascular disease and trauma. The brain’s blood supply arises from the internal carotid arteries (anterior circulation) and the vertebral arteries (posterior circulation). They are shown in Fig. 55.10. The internal carotid arteries provide blood flow to the anterior and middle portions of the cerebrum. The vertebral arteries join to form the basilar artery, which branches to supply the middle and lower parts of the temporal lobes, occipital lobes, cerebellum, brainstem, and part of the diencephalon. The main branch of the basilar artery is the posterior cerebral artery. The circle of Willis is formed by communicating arteries that join the basilar and internal carotid arteries (Fig. 55.11). The circle of Willis plays a key role in cerebral blood flow. Interestingly, only 40% of us have a well-formed, complete circle of Willis. Everyone else has a degree of variation.4 Superior to the circle of Willis, 3 pairs of arteries supply blood to the left and right hemispheres. The anterior cerebral artery feeds the medial and anterior portions of the frontal lobes. The middle cerebral artery feeds the outer portions of the frontal, parietal, and superior temporal lobes. The posterior cerebral artery feeds the medial portions of the occipital and inferior temporal lobes. Venous blood drains from the brain through the dural sinuses, which form channels that drain into the 2 jugular veins. Blood-Brain Barrier The blood-brain barrier is a physiologic barrier between blood capillaries and brain tissue. This barrier protects the brain from harmful agents, while allowing nutrients and gases to enter. The structure of brain capillaries differs from that of other capillaries, so substances that normally pass into most tissues are prevented from entering brain tissue. Lipid-soluble compounds enter the brain easily. Water-soluble and ionized drugs enter the brain and the spinal cord slowly. Thus the blood-brain barrier affects the penetration of drugs. Only certain drugs can enter the CNS from the bloodstream. Protective Structures Meninges The meninges consist of 3 protective membranes that surround the brain and spinal cord: the dura mater, arachnoid, and pia mater (Fig. 55.12). The thick dura mater forms the outermost layer. The falx cerebri is a fold of the dura that separates the 2 cerebral hemispheres. It slows expansion of brain tissue in conditions such as a rapidly growing tumor or acute hemorrhage. The tentorium cerebelli is a fold of dura that separates the cerebral hemispheres from the posterior fossa (which contains the brainstem and cerebellum). The arachnoid layer is a fragile, web-like membrane that lies between the dura mater and pia mater (the vascular innermost layer of the meninges). The area between the arachnoid layer and pia mater (subarachnoid space) is filled with CSF. Structures such as arteries, veins, and cranial nerves passing to and from the brain and skull must pass through the subarachnoid space. A larger subarachnoid space in the region of the third and fourth lumbar vertebrae is the area used to obtain CSF during a lumbar puncture. Skull The skull protects the brain from external trauma. It is composed of 8 cranial bones and 14 facial bones. Although the top and sides of the inside of the skull are fairly smooth, the bottom surface is uneven. It has many ridges, prominences, and foramina (holes through which blood vessels and nerves enter the intracranial vault). The largest hole is the foramen magnum, through which the brainstem extends to the spinal cord. The foramen magnum is the only major space for the expansion of brain contents when increased intracranial pressure occurs. Vertebral Column The vertebral column protects the spinal cord, supports the head, and provides flexibility. The vertebral column is made up of 33 individual vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 sacral (fused into 1), and 4 coccygeal (fused into 1). Each vertebra has a central opening through which the spinal cord passes. A series of ligaments holds the vertebrae together. Intervertebral discs occupy the spaces between vertebrae, allowing movement of the column. Fig. 55.13 shows the natural curvature of the spinal column and its relation to the trunk. Gerontologic Considerations: Effects of Aging on Nervous System Aging affects several parts of the nervous system. In the CNS, the gradual loss of neurons in certain areas of the brainstem, cerebellum, and cerebral cortex begins in early adulthood. With loss of neurons, the ventricles widen or enlarge, brain weight decreases, cerebral blood flow decreases, and CSF production declines. In the PNS, degenerative changes in myelin cause a decrease in nerve conduction. Coordinated neuromuscular activity, such as maintaining BP in response to changing from a lying to a standing position, is altered with aging. As a result, older adults are more likely to have orthostatic hypotension. Similarly, coordination of neuromuscular activity to maintain body temperature becomes less efficient with aging. Older adults are less able to adapt to extremes in environmental temperature and are more vulnerable to both hypothermia and hyperthermia. Other relevant changes associated with aging include decreases in memory, vision, hearing, taste, smell, vibration, position sense, muscle strength, and reaction time. Sensory changes, including decreases in taste and smell perception, may result in decreased dietary intake in the older adult. Reduced hearing and vision can result in perceptual confusion.5Problems with balance and coordination can put the older adult at risk for falls.6 Changes in assessment findings result from age-related changes in the nervous system (Table 55.2). Changes should not be attributed to aging without considering other underlying causes. Assessment of Nervous System Subjective Data Important Health Information Past Health History When performing a neurologic examination, first determine if an emergency exists. For example, does the patient have decreasing level of consciousness? The neurologic assessment is done when an abnormality is identified during screening or can be expected based on patient history. Is the patient a reliable historian and able to give detailed information? If not, interview someone with first-hand knowledge of the patient’s history and current problem. Avoid suggesting symptoms or asking leading questions. Second, the mode of onset and course of the illness are especially important aspects of the history. Often these facts alone can reveal the nature of a neurologic disease process. Obtain all pertinent data in the history of the present illness, especially data related to the characteristics and progression of the symptoms. In some cases, the history may include birth injury (e.g., cerebral palsy from hypoxia) and/or other neurologic insults, such as a traumatic brain injury, stroke, or degenerative disease. Growth and developmental history can be important in determining if nervous system dysfunction was present at an early age. Specifically, ask about major developmental tasks, such as walking and talking. Medications Obtain a careful medication history, especially the use of sedatives, opioids, tranquilizers, and mood-elevating drugs. Many other drugs can cause neurologic side effects. Ask the patient to describe the medication regimen to determine adherence to prescribed therapies. Surgery or Other Treatments Ask about any surgery involving any part of the nervous system, such as head, spine, or sensory organs. If a patient had surgery, determine the date, cause, procedure, recovery, and current status. Note any history of eye surgery to determine the relevance of abnormal pupil assessment. Functional Health Patterns Key questions to ask a patient with a neurologic problem are outlined in Table 55.3. Health Perception–Health Management Pattern Ask about the patient’s health practices that affect the nervous system, such as substance use, smoking, adequate nutrition, BP management, safe participation in physical and recreational activities, and use of seat belts or helmets. Ask about hospitalizations for neurologic problems. If the patient has an existing neurologic problem, assess how it affects daily living and the ability to perform self-care. After a careful review of information, ask someone who knows the patient well whether they notice any mental or physical changes in the patient. The patient with a neurologic problem may not be aware of it or may be a poor historian. Nutritional-Metabolic Pattern Neurologic problems can result in poor nutrition. Problems related to chewing, swallowing, facial nerve paralysis, and muscle coordination could make it difficult for the patient to ingest adequate nutrients. Certain vitamins, such as thiamine (B1), niacin, and pyridoxine (B6), are essential for the health of the CNS. Deficiencies in any of these can result in nonspecific problems, such as depression, apathy, neuritis, weakness, mental confusion, and irritability. Cobalamin (vitamin B12) deficiency can occur in older adults, who may have problems with vitamin absorption from supplements as well as natural food sources, such as meat, fish, and poultry. Untreated, cobalamin deficiency can cause mental function decline. In the patient with brain injury, early nutritional support can markedly improve outcomes.7 Elimination Pattern Bowel and bladder problems often are associated with neurologic problems, such as stroke, head injury, spinal cord injury, MS, and dementia. To plan appropriate interventions, determine if the bowel or bladder problem was present before or after the current neurologic event. Urinary retention and incontinence of urine and feces are the most common elimination problems associated with a neurologic problem or its treatment. For example, nerve root compression (as occurs in cauda equina conditions) leads to a sudden onset of incontinence. Record key details, such as number of episodes, accompanying sensations or lack of sensations, and measures to control the problem. Activity-Exercise Pattern Many neurologic disorders can cause problems in the patient’s mobility, strength, and coordination. These problems can affect the patient’s usual activity and exercise patterns and can increase the risk for falls.6 Assess the person’s activities of daily living because neurologic diseases can affect the ability to perform motor tasks, which increases the risk for injury. Sleep-Rest Pattern Sleep pattern changes can be both a cause and a response to neurologic problems. Pain and reduced ability to change position because of muscle weakness and paralysis could interfere with sleep quality. Hallucinations resulting from dementia or drugs can interrupt sleep. Carefully assess and record the patient’s sleep pattern and bedtime routines. Cognitive-Perceptual Pattern Because the nervous system controls cognition and sensory integration, many neurologic problems affect these functions. Consider culture, age, and education when assessing communication because they play a role in our interaction with others. Assess memory, language, calculation ability, problem-solving ability, insight, and judgment. Ask the patient hypothetical questions such as, “What is a reasonable price for a cup of coffee?” or “What would you do if you saw a car crash outside your house?” Consider if the patient’s plans and goals match the physical and mental capabilities. Note the presence of factors affecting intellectual capacity, such as cognitive impairment, hallucinations, delusions, and dementia. Assess a person’s ability to use and understand language. Appropriateness of responses is a useful indicator of cognitive and perceptual ability. Determine the patient’s understanding and ability to carry out needed treatments. Neurologic-related cognitive changes can interfere with the patient’s understanding of the disease and adherence to related treatment. Pain is common with many neurologic problems and is often the reason a patient seeks care. Carefully assess the patient’s pain. (Pain and pain assessment are discussed in Chapter 8.) Self-Perception–Self-Concept Pattern Neurologic diseases can drastically change a patient’s control over life and create dependency on others for meeting daily needs. The patient’s physical appearance and emotional control can be affected. Sensitively ask about the patient’s evaluation of self-worth, perception of abilities, body image, and general emotional pattern. Role-Relationship Pattern Physical impairments, such as weakness and paralysis, can alter or limit participation in usual roles and activities. Cognitive changes can permanently alter a person’s ability to maintain previous roles. These changes can dramatically affect the patient and caregiver. Ask the patient if a role change has occurred (e.g., spouse or breadwinner) because of neurologic problems and determine how long it has lasted. Caregivers should take part in decision making when neurologic deficits prevent the patient from decisions that will affect the role. Sexuality-Reproductive Pattern Assess the person’s ability to take part in sexual activity. Many neurologic disorders can affect sexual response. Cerebral lesions may inhibit the desire phase or the reflex responses of the excitement phase. The hypothalamus stimulates the pituitary gland to release hormones that influence sexual desire. Brainstem and spinal cord lesions may partially or completely interrupt the desire or ability to have intercourse. Neuropathies and spinal cord lesions may prevent reflex activities of the sexual response or affect sensation and decrease desire. Despite neurologically related changes in sexual function, many persons can achieve satisfying expression of intimacy and affection. Coping–Stress Tolerance Pattern The physical sequelae of a neurologic problem can strain a patient’s coping ability. Often the problem is chronic, and the patient must learn new coping skills. Assess if the patient’s coping skills are adequate to deal with the stress of this problem. Also assess the patient’s support system. Value-Belief Pattern Many neurologic problems have serious, long-term, life-changing effects. Determine what these effects are because they can strain the patient’s belief system. Assess if any religious or cultural beliefs could affect the treatment plan. Objective Data Physical Examination The standard neurologic examination helps determine the presence, location, and nature of nervous system disease (Fig. 55.14). The examination assesses 6 categories of function: mental status, cranial nerve function, motor function, sensory function, cerebellar function, and reflexes.8 Develop a consistent pattern of completing the neurologic examination to remember to include each element for every patient examination. Mental Status Assessment of mental status (cerebral function) gives a general impression of how the patient is functioning. It involves determining complex and highlevel cerebral functions governed by many areas of the cerebral cortex. Complete most of the mental status examination during your interaction with the patient. For example, assess language and memory when asking the patient for details of the illness and significant past events. Consider the patient’s age, cultural background, and level of education when evaluating mental status. The components of the mental status examination include: • General appearance and behavior: This includes level of consciousness (awake, asleep, comatose), motor activity, body posture, dress and hygiene, facial expression, and speech pattern. This assessment begins when you first see the patient. A patient who has deficits in self-care as shown by poor grooming is more likely to have other cognitive deficits. • Cognition: Note orientation to time, place, person, and situation, as well as memory, general knowledge, insight, judgment, problem solving, and calculation. Common questions are “Who were the last 3 presidents?” “What do people use to cut paper?” “Can you count backward from 100 by 7s?”8 Often a structured mental status questionnaire is used to evaluate these functions and provide baseline data for evaluating changes over time. Common tools include the Mini-Mental State Examination (MMSE) (see Table 59.10) and Montreal Cognitive Assessment (MoCA).9 Delirium is an acute and transient disorder of cognition that can be seen at any time during a patient’s illness. As discussed in Chapter 59, delirium is often an early indicator of various illnesses (see Table 59.16). The Confusion Assessment Method tool is used to assess for delirium (see Table 59.18). • Mood and affect: Note any agitation, anger, depression, or euphoria, and the appropriateness of these states. Use suitable questions to reveal the patient’s feelings. Cranial Nerves Olfactory nerve Chronic rhinitis, sinusitis, and heavy smoking may decrease the sense of smell. Problems with the ability to smell may be associated with a tumor involving the olfactory bulb or the result of a basilar skull fracture that has damaged the olfactory fibers as they pass through the delicate cribriform plate of the skull. Anosmia (loss of sense of smell) is an early sign in Parkinson’s disease and Alzheimer’s disease.10 Optic nerve Visual field defects may arise from lesions of the optic nerve, optic chiasm, or tracts that extend through the temporal, parietal, or occipital lobes. Visual field changes resulting from brain lesions include hemianopsia (half of the visual field is affected), quadrantanopia (one fourth of the visual field is affected), bitemporal hemianopsia (bilateral peripheral vision is affected), or monocular vision. It may be hard to test acuity if the patient does not read English or is aphasic. Oculomotor, trochlear, and abducens nerves Because the oculomotor (CN III), trochlear (CN IV), and abducens (CN VI) nerves help move the eye, they are tested together (Table 55.4). With weakness or paralysis of an eye muscle, the eyes do not move together, and the patient has a disconjugate gaze. Note the presence and direction of nystagmus (fine, rapid jerking movements of the eyes), even though this condition most often indicates vestibulocerebellar problems. Because the oculomotor nerve exits at the top of the brainstem at the tentorial notch, it can be compressed easily by expanding mass lesions. When this occurs, sympathetic input to the pupil is unopposed; the pupil changes shape and becomes dilated. The lack of pupillary constriction is an early sign of central herniation (see Chapter 56). Two abbreviations we often used to record the reaction of the pupils are PERRL (Pupils are Equal [in size], Round, and Reactive to Light) and PERRLA (Pupils are Equal, Round, and Reactive to Light and Accommodation). The PERRLabbreviation is appropriate when accommodation cannot be assessed, as in an unconscious patient. Convergence and accommodation are tested by having the patient focus on the examiner’s finger as it moves toward the patient’s nose. Another function of the oculomotor nerve is to keep the eyelid open. Damage to the nerve can cause ptosis (drooping eyelid), pupillary abnormalities, and eye muscle weakness. Motor System The motor system examination includes assessment of strength, tone, coordination, and symmetry of the major muscle groups. Test muscle strength by asking the patient to push and pull against the resistance of your arm as it opposes flexion and extension of the patient’s muscle. Ask the patient to offer resistance at the shoulders, elbows, wrists, hips, knees, and ankles. Mild weakness of the arm is demonstrated by downward drifting of the arm or pronation of the palm (pronator drift). The pronator drift test is especially sensitive when the patient has a potential for vasospasm or increasing edema in 1 hemisphere of the cerebrum. Ask the patient to close the eyes and hold the arms out with palms facing up (like they are holding a large pizza). The patient should hold this position for 30 seconds. Downward drift with palm pronation indicates a problem in the opposite motor cortex. Note any weakness or asymmetry of strength between the same muscle groups of the right and left sides. Test muscle tone by passively moving the limbs through their range of motion. You should identify a slight resistance to these movements. Abnormal tone is described as hypotonia (flaccidity) or hypertonia (spasticity). Note any involuntary movements, such as tics, tremor, myoclonus (spasm of muscles), athetosis (slow, writhing, involuntary movements of extremities), chorea (involuntary, purposeless, rapid motions), and dystonia (impairment of muscle tone). Test cerebellar function by assessing balance and coordination. A good screening test for both balance and muscle strength is to observe the patient’s stature (posture while standing) and gait. Note the pace and rhythm of the gait. Observe for normal symmetric and oppositional arm swing. The patient’s ability to ambulate helps to determine the level of nursing care needed and the risk for falling. The finger-to-nose test (having the patient alternately touch the nose, then touch the examiner’s finger) and the heel-to-shin test (having the patient stroke the heel of 1 foot up and down the shin of the opposite leg) assess coordination and cerebellar function. Reposition your finger while the patient is touching the nose so that the patient must adjust to a new distance each time your finger is touched. These movements should be performed smoothly and accurately. Other tests include asking the patient to pronate and supinate both hands rapidly and to do a shallow knee bend, first on 1 leg and then on the other. Note dysarthria or slurred speech because it is a sign of incoordination of the speech muscles. Sensory System In the somatic sensory examination, several modalities are tested. Each modality is carried by a specific ascending pathway in the spinal cord before it reaches the sensory cortex. As a rule, perform the examination with the patient’s eyes closed and avoid providing the patient with clues. Ask “How does this feel?” rather than “Is this sharp?” In the routine neurologic examination, sensory testing of the anterior torso, posterior torso, and all extremities is sufficient. However, if a problem is identified in sensory function, the boundaries of that dysfunction should be carefully delineated along the dermatome. Touch, pain, and temperature Light touch is usually tested first using a cotton wisp or light pinprick. Gently touch each extremity and ask the patient to indicate when they feel the stimulus. Test pain by alternately touching the skin with the sharp and dull end of a pin. Tell the patient to respond “sharp” or “dull.” Evaluate each limb separately. Extinction is assessed by simultaneously touching both sides of the body symmetrically. Normally, the simultaneous stimuli are both perceived (sensed). An abnormal response occurs when the patient perceives the stimulus on only 1 side. The other stimulus is extinguished. Test the sensation of temperature by applying tubes of warm and cold water to the skin and asking the patient to identify the stimuli with the eyes closed. If pain sensation is intact, you do not have to assess temperature sensation because the same ascending pathways carry both sensations. Vibration sense Assess vibration sense by applying a vibrating tuning fork to the fingernails and bony prominences of the hands, legs, and feet. Ask the patient if the vibration or “buzz” is felt. Then ask the patient to indicate when the vibration ceases. Position sense Assess position sense (proprioception) by placing your thumb and forefinger on either side of the patient’s forefinger or great toe and gently moving his or her digit up or down. Ask the patient to close the eyes and state the direction in which the digit is moved. Another test of proprioception is the Romberg test. Ask the patient to stand with feet together and then close his or her eyes. If the patient can maintain balance with the eyes open but sways or falls with the eyes closed (i.e., a positive Romberg test), vestibulocochlear dysfunction or disease in the posterior columns of the spinal cord may be present. Be aware of patient safety during this test. Cortical sensory functions Several tests evaluate cortical integration of sensory perceptions (which occurs in the parietal lobes). Explain these tests to the patient before performing them, while his or her eyes are still open. Assess two-point discrimination by placing the 2 points of a calibrated compass on the tips of the fingers and toes. The minimum recognizable separation is 4 to 5 mm in the fingertips and a greater degree of separation elsewhere. This test is important in diagnosing diseases of the sensory cortex and PNS. FIG. 55.16 The examiner strikes a swift blow over a stretched tendon to elicit a stretch reflex. A, Biceps reflex. B, Patellar reflex. Test graphesthesia (ability to feel writing on skin) by having the patient identify numbers traced on the palm of the hands. Test stereognosis (ability to perceive the form and nature of objects) by having the patient close the eyes and identify the size and shape of easily recognized objects (e.g., coins, keys, safety pin) placed in the hands. Reflexes Tendons have receptors that are sensitive to stretch. A reflex contraction of the skeletal muscle occurs when the tendon is stretched. In general, we test the biceps, triceps, brachioradialis, patellar, and Achilles tendon reflexes. Initiate a simple muscle stretch reflex by briskly tapping the tendon of a stretched muscle, usually with a reflex hammer (Fig. 55.16). Measure the response (muscle contraction of the corresponding muscle) on a 0 to 5 scale as follows: 0 = absent reflex; 1 = weak response, seen only with reinforcement; 2 = normal response; 3 = brisk response; 4 = hyperreflexia with nonsustained clonus; and 5 = hyperreflexia with sustained clonus. Clonus, an abnormal response, is a continued rhythmic contraction of the muscle with continuous application of the stimulus. Elicit the biceps reflex, with the patient’s arm partially flexed and palm up, by placing your thumb over the biceps tendon in the antecubital space and striking the thumb with a hammer. The normal response is flexion of the arm at the elbow or contraction of the biceps muscle that you can feel with your thumb. Elicit the triceps reflex by striking the triceps tendon above the elbow while the patient’s arm is flexed. The normal response is extension of the arm or visible contraction of the triceps. Elicit the brachioradialis reflex by striking the radius 3 to 5 cm above the wrist while the patient’s arm is relaxed. The normal response is flexion and supination at the elbow or visible contraction of the brachioradialis muscle. Elicit the patellar reflex by striking the patellar tendon just below the patella. The patient can be sitting or lying as long as the leg being tested hangs freely. The normal response is extension of the leg with contraction of the quadriceps. Gently dorsiflex the patient’s foot at the ankle. Elicit the Achilles tendon reflex by striking the Achilles tendon while the patient’s leg is flexed at the knee. The normal response is plantar flexion at the ankle. A focused assessment is used to evaluate the status of previously identified neurologic problems and to monitor for signs of new problems. A focused assessment of the neurologic system is shown in the box on p. 1294. Diagnostic Studies of Nervous System Many diagnostic studies are available to assess the nervous system (Tables 55.7, 55.8, 55.9, and 55.10). CSF analysis provides information about a variety of CNS diseases. Normal CSF is clear, colorless, odorless, and free of red blood cells. It contains little protein. Normal CSF values are listed in Table 55.7. CSF may be obtained through lumbar puncture (LP) or, on occasion, ventriculostomy. During LP, the HCP aspirates CSF through a needle inserted into the L3-4 or L4-5 interspace. A manometer attached to the needle is used to obtain CSF pressure. CSF is withdrawn in a series of tubes and sent for analysis. LP is contraindicated in the presence of increased intracranial pressure because of the risk for downward herniation from CSF removal or if there is infection at the intended puncture site. Nursing care of the patient undergoing LP is outlined in Table 55.8. Biopsies of nerve, muscle, brain, and arterial tissues are useful in diagnosing several disorders (e.g., tumors, infectious disease, degenerative diseases, temporal artery for arteritis). A brain biopsy is usually done using a stereotactic procedure. CNS, Central nervous system; LMN, lower motor neuron.