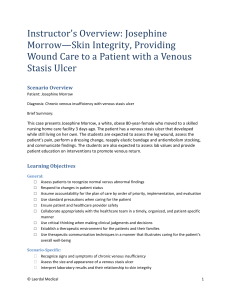
Josephine Morrow Documentation Assignments 1. Document the findings of a focused skin assessment of Ms. Morrow, including any findings that identify the presence of chronic venous insufficiency. - When assessing the patients skin color is normal for ethnicity and intact, except she does have brown hyperpigmentation bilaterally from the knees and down both sides with 2+ edema. There is a venous tasis ulcer on the right medial malleolus, it is covered with a hydrocolloid dressing. The skin is dry, elasticity is normal and there is no evidence of tenting. Pedal and radial pulses were 95, strong/regular. The dressing was removed and the wound was assessed and documented. Wound was irrigated and new dressing applied. 2. Document any abnormal laboratory results that are associated with the presence or status of Ms. Morrow's stasis ulcer. - Patients abumin level was 3.4 g/dL, slightly below normal. Decreased albumin levels can impact the wound healing process. - Prealbumin 14.7 mg/dL, significantly below level. Decreased prealbumin levels can come from inlfamation and wounds. 3. Record the results of Ms. Morrow's Braden Scale assessment. - The patients score on the braden scale was 16, and her skin is intact except for the venous stasis ulcer on the right medial malleolus. This puts her at moderate risk for an acquired pressure ulcer. 4. Document the characteristics of Ms. Morrow's venous stasis ulcer. - The ulcer is shallow, 1 inch in width, and mostly looks pink to red, no signs of necrosis or infection. 5. Document the dressing change and irrigation of Ms. Morrow’s wound. - The patient was medicated 30 mins before the dressing change was performed to avoid unneded pain. Assessed the current dressing, it was dry clean and intact. Hydrocolloid dressing was removed and ulcer was assessed. Findings documented. Ulcer was irrigated w/ normal saline and a new hydrocolloid dressing was applied. Compression stockings were put on and elevated her legs. Aareas around the ulcer should be monitored daily. Ulcer itself shoud be irrigated with a dressing change every 3 days. 6. In the chart, record patient education on ways to promote venous return. - Patient education on ways to promote venous return included getting up and walking around regularly, avoid prolonged standing or sitting, elevate legs, wiggle their feet ip and down whilein bed or sitting in chair. Compression stockings should be used as well to help promote venour return. From vSim for Nursing | Fundamentals. © Wolters Kluwer