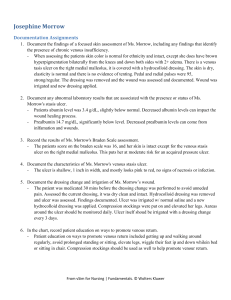
Josephine Morrow Guided Reflection Questions Opening Questions How did the simulated experience of Josephine Morrow’s case make you feel? The simulated experience of Josephine Morrow gave me a better understanding in regards to the proper care that is required for ulcers and whaat to look for in the case of infection. I learned ways to educate the patient on proper ways to promote venous return and methods to take in order to improve circulation. It took me some time to plan how I was going to assess the patient and properly care for her. After planning out what assessments I would do for the patient, I was able to successfully care for the patient. Talk about what went well in the scenario. I started off the simulation by introducing myself, performing hand hygiene and confirming the patient’s ID. I assessed the patient’s legs and her wound, changed the dressing, and provided patient education for wound care and for improving venous return. In this scenario, I feel I provided quality care for the patient and properly assessed her. The patient was able to understand all the information provided to her. Reflecting on Josephine Morrow’s case, were there any actions you would do differently if you were to repeat this scenario? If so, how would your patient care change? What I would do differently in this scenario would be to make sure I maintain proper asepsis regarding the wound procedure. I would make sure that adequate hygiene is performed in order to prevent any further infection. I received a 100% on my simulation which makes me feel like I did a proper assessment and properly educated the patient. Scenario Analysis Questions S What priority problem(s) did you identify for Josephine Morrow? The priority problems for Ms. Morrow were risk for impaired skin integrity, risk of infection, delayed wound healing, and fall risk. PCC Identify in Josephine Morrow’s health history any factors that predisposed her to having chronic venous insufficiency. The Scenario Analysis Questions are correlated to the Quality and Safety Education for Nurses (QSEN) competencies: Patient-Centered Care (PCC), Teamwork and Collaboration (T&C), Evidence-Based Practice (EBP), Quality Improvement (QI), Safety (S), and Informatics (I). Find more information at: http://qsen.org/ From vSim for Nursing | Fundamentals. © Wolters Kluwer. Ms. Morrow’s health history included COPD, DVT, obesity, and lack of mobility. These are all factors that will increase her predisposing to venous insufficiency. Ms. Morrow’s age can also be a factor regarding her mobility and ability to promote venous return. PCC/S Discuss the assessment findings and diagnostic studies that correlate with chronic venous insufficiency and venous stasis ulceration. Provide the reasons behind these findings. Ms. Morrow developed a venous stasis ulcer to the right medial malleolus. She had brown hyperpigmentation bilaterally on both legs with +2 edema. The hyperpigmentation on her lower legs may be due to lack of oxygenated blood flow in her legs. The +2 edema is related to her venous insufficiency due to the fluid. In her legs not moving like it should. Her labs showed she had abnormal prealbumin, albumin, and HCO3 levels. The pressure ulcer from her immobility also correlated to her venous insufficiency. S What is the rationale for the daily dose of ASA? The rationale for the daily dose of ASA is to help promote Ms. Morrow’s circulation and reduce the risk of blood clots. EBP/I What is the rationale for compression therapy? The rationale for compression therapy is to help promote circulation and further venous stasis. The compression therapy helps control leg swelling and discomfort. It is designed to provide support to the veins and legs, assist with circulation, and minimize swelling. EBP/I What is the rationale for performing a Braden scale assessment on Josephine Morrow? The rationale for performing a Braden Scale assessment was to evaluate the chances of the patient developing a pressure ulcer. T&C What other interprofessional team members should be involved in Josephine Morrow’s care? A dietician and the wound care team should be involved in Ms. Morrow’s care. Ms. Morrow maay need a physical therapist and a respiratory specialist. She may potentially need a home health nurse for when she returns to her normal life at home after discharge. Concluding Questions Describe how you would apply the knowledge and skills that you acquired in Josephine Morrow’s case to an actual patient care situation. The simulation helped me learn how to perform a focused assessment on the patient with chronic venous insufficiency. I learned how to educate a patient on preventing venous stasis ulcers and educating them on wound care. I can apply the knowledge I obtained from this simulation by remembering to stay focused on the reason the patient is being treated. I learned to assess the dressing prior to changing and after. I learned to make sure I document all my findings. I can apply the skills acquired in this case to actual patient care by making sure my patient is always comfortable and safe. I will assess ulcer wounds properly and promote ambulation as well as turning the patient every 2 hours. From vSim for Nursing | Fundamentals. © Wolters Kluwer. I will monitor labs to ensure the patient is maintain proper nutrition. I learned to include interprofessional team members to assist the paitent and work together to provide the best high-quality individualized care for the patient. From vSim for Nursing | Fundamentals. © Wolters Kluwer.