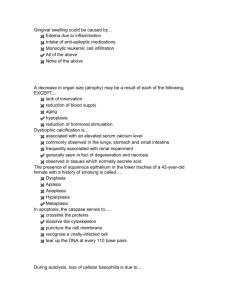
Patho chap 1 - block 1 test Study online at quizlet.com/_6ji3fm 1. Acid reflux from the stomach causes metaplasia to? non-ciliated, mucin-producing columnar cells 18. Carbon tetrachloride (CCL4) will be converted to? CCL3 free radical by P450 system of hepatocytes 2. acute ischemia results in? injury 19. Caseous necrosis 3. After the dying cell shrinks, nucleus will then? condense and fragments in an organized manner soft and friable necrotic tissue with "cottage cheese like" appearance 4. After the nucleus condenses and fragments? apoptotic bodies fall from the cell and are removed by macrophages 20. caseous necrosis is a combination of? coagulative and liquefactive necrosis 21. Alzheimer disease Alpha-beta amyloid deposits in the brain forming amyloid plaques caseous necrosis is characteristic of? granulomatous inflammation due to TB or fungal infection 22. caspases that mediate apoptosis, will activate? 1. proteases 2. endonucleases 23. catalase results in? O2 and H2O 24. causes of hypoxia, include? 1. ischemia 2. hypoxemia 3. decreased O2-carrying capacity of blood 25. Cellular injury, occurs when? stress exceeds the cell's ability to adapt 26. the change of tissue in vitamin A deficiency, is known as? keratomalacia 27. Classic findings of systemic amyloidosis? 1. nephrotic syndrome 2. restrictive cardiomyopathy or arrhythmia 3. tongue enlargement, malabsorption, and hepatosplenomegaly 28. Coagulative necrosis is? necrotic tissue that remains firm and nucleus disappears 5. 6. Amyloid misfolded protein that deposits in the extracellular space, damaging tissues 7. Aplasia failure of cell production during embryogenesis 8. Apoptosis is? genetically programmed, cell death involving single cells or small groups of cell 9. Apoptosis is? energydependent or energyindependent? energy (ATP)-dependent 10. apoptosis is followed by/ not followed by inflammation? not followed by inflammation 11. Apoptosis is mediated by? caspases 12. Atrophy decrease in stress that leads to a decrease in organ size 13. atrophy occurs via? decrease in the size and number of cells 14. autophagic vauoles will fuse with? lysosomes, whose hydrolytic enzymes breakdown cellular components 15. autophagy of cellular components involves? generation of autophagic vacuoles 16. Barrett esophagus is a classic example of? metaplasia Carbon tetrachloride (CCL4) results in? cell injury with swelling of RER 17. cell shape and organ structure are preserved by coagulation of proteins 29. coagulative necrosis is an area of? infarcted tissue that often wedge-shaped and pale 30. common causes of cellular injury, include? 1. inflammation 2. nutritional deficiency/ excess 3. hypoxia 4. trauma 5. genetic mutations 31. cytosolic enzymes leak into the serum, during? cardiac troponin 32. cytosol swelling, results in? 1. loss of microvilli 2. membrane blebbing 33. Cytotoxic CD8+ T cellmediated pathway pathway that activates caspases 51. Elimination of free radicals occurs via? 1. antioxidants 2. enzymes 3. metal carrier proteins 52. Endonucleases break down DNA 53. the end result of liquefaction, of liquefactive necrosis? lysis of cells and proteins 54. the end results of irreversible injury? cell death 55. enzymes that help with the elimination of free radicals? 1. superoxide dismutase 2. glutathione peroxidase 3. catalase 56. esophagus is normally lined with? non-keratinizing squamous epithelium 57. examples of apoptosis include? 1. endometrial shedding during menstrual cycle 2. removal of cells during embryogenesis 3. CD8+ T cell-mediated killing of virally infected cells 58. examples of decreased O2 carrying capacity 1. anemia 2. carbon monoxide poisoning 3. methemoglobinemia 59. examples of localized amyloidosis? 1. senile cardiac amyloidosis 2. familial amyloid cardiomyopathy 3. non insulin dependent diabetes mellitus 4. alzheimer disease 5. dialysis-associated amyloidosis 6. medullary carcinoma of the thyroid lactic acid buildup results in low pH, which denatures proteins and precipitates DNA 60. exception of pathologic hyperplasia? benign prostatic hyperplasia Due to low ATP, what will happen with the Ca2+ pump resulting in Ca2+ buildup in the cytosol of the cell 61. Extrinsic receptorligand pathway pathway that activates caspases 62. Due to low ATP, what will happen with the Na+/K+ pump sodium and water buildup in the cell Familial amyloid cardiomyopathy mutated serum transthyretin deposits in the heart leading to restrictive cardiomyopathy 63. fat necrosis 47. dysplasia disordered cellular growth 48. dysplasia is reversible/irreversible? reversible necrotic adipose tissue with chalkywhite appearance due to deposition of calcium 64. 49. dysplasia most often refers to? proliferation of precancerous cells fat necrosis is characteristics of? trauma to fat and pancreatitismediated damage of peripancreatic fat dysplasia often arises from? longstanding pathologic hyperplasia or metaplasia 65. fibrinoid necrosis 50. necrotic damage to blood vessel wall 34. Cytotoxic CD8+ T cellmediated pathway occurs when? perforins secreted by CD8+T cell creates pores in membrane of target cell and granzyme from CD8+T cell enters pores -> activates caspases 35. decreased apolipoproteins leads to? fatty change in the liver 36. decreased arterial perfusion can occur with? atherosclerosis 37. Decreased O2 carrying capacity arises with? hemoglobin (Hb) loss or dysfunction 38. decreased venous drainage occurs with? budd-chiari syndrome 39. decrease in cell number occurs via? apoptosis 40. decrease in cell size occurs via? 1. ubiquitin-proteosome degradation of the cytoskeleton 2. autophagy of cellular components 41. deposition of amyloidosis can be? systemic or localized 42. Dialysis-associated amyloidosis Beta-2 microglobulin deposits in joints 43. DNA damage is implicated in? aging and oncogenesis 44. Due to low ATP, what will happen with aerobic glycolysis results in a switch to anaerobic glycolysis 45. 46. 66. fibrinoid necrosis is characteristic of? 1. malignant hypertension 2. vasculitis 67. free radicals cause cellular injury via? peroxidation of lipids and oxidation of DNA and proteins 68. Gangrenous necrosis coagulative necrosis that resembles mummified tissue 69. gangrenous necrosis is characteristic of? ischemia of lower limb and GI tract 70. glutathione peroxidase results in? GS-SG and H2O 71. the hallmark of irreversible injury is? membrane damage how are drugs and chemicals associated with free radicals? P450 system of liver metabolite drugs, generating free radicals 73. how are metals associated with free radicals? Fe2+ generates hydroxyl free radicals 74. how is inflammation associated with free radicals? NADPH oxidase generates superoxide ions during oxygendependent killing by neutrophils 75. how is ionizing radiation associated with free radicals? water is hydrolyzed to hydroxyl free radical 76. hyperplasia increase in the number of cells 77. Hyperplasia involves? production of new cells from stem cells 78. hypertrophy increase in the size of cells 79. Hypertrophy involves? gene activation, protein synthesis, production of organelles 80. Hypoplasia decrease in cell production during embryogenesis 81. Hypoplasia usually results in? relatively small organ 82. Hypoxemia low partial pressure of oxygen in the bloos 83. Hypoxemia, arises with? 1. high altitude 2. hypoventilation 3. diffusion defect 4. V/Q mismatch 72. 84. Hypoxia low oxygen delivery to tissue 85. hypoxia impairs? oxidative phosphorylation resulting in decreased ATP 86. if superimposed infection of dead tissue occurs with gangrenous necrosis? then liquefactive necrosis ensues 87. in carbon monoxide poisoning, what happens? CO binds hemoglobin more avidly than oxygen Pao2 normal Sao2 decreased 88. in coagulative necrosis, red infarction arises if? blood re-enters a loosely organized tissue 89. in fat necrosis, fatty acids are released by? trauma or lipase join with calcium via saponification 90. in fibrinoid necrosis, there is leaking of? proteins into vessel walls 91. initial phase of cellular injury? reversible/ irreversible? reversible 92. in methemoglobinemia, what happens? iron in heme is oxidized to Fe3+, which cannot bind oxygen Pao2 normal Sao2 decreased 93. In the extrinsic receptorligand pathway, how does the caspase activate? 1. FAS ligand binds FAS death receptor (CD95) on the target cell -> activates caspases 2. tumor necrosis factor (TNF) binds TNF receptor on the target cell -> activates caspases 94. Intrinsic mitochondrial pathway pathway that activates caspases 95. in vitamin A deficiency, the thin squamous lining of the conjunctiva undergoes? metaplasia into stratified keratinizing squamous epithelium 96. Ischemia arises with? 1. decreased arterial perfusion 2. decreased venous drainage 3. shock 97. Ischemia is? decreased blood flow through an organ 98. is systemic amyloidosis treatable? damaged organs must be transplanted -> amyloid cannot be removed 99. lack of Bcl2 allows? cytochrome c to leak from the inner mitochondrial matrix into the cytoplasm -> activate caspases 116. metastatic calcification occurs when? high serum calcium or phosphate levels lead to calcium deposition in normal tissue 100. the leaking of proteins in fibrinoid necrosis results in? bright pink staining of the wall microscopically 117. mitochondrial membrane damage results in? 1. loss of electron transport chain 2. cytochrome c leaking into cytosol 101. the likelihood of injury depends on? 1. the type of stress 2. severity 3. type of cell affected 118. the morphologic hallmark of cell death is? loss of the nucleus 102. liquefactive necrosis is? necrotic tissue that becomes liquefied 119. Necrosis is? large groups of cells, followed by acute inflammation 103. liquefactive necrosis is a characteristic of? 1. brain infarction 2. abscess 3. pancreatitis 120. Necrosis is divided into? several types, based on gross features 121. Necrosis is due to? liquefactive necrosis occurs with abscess via? proteolytic enzymes from neutrophils liquefy tissue some other underlying pathologic process 105. liquefactive necrosis occurs with brain infarction via? proteolytic enzymes from microglial cells liquefy the brain 106. liquefactive necrosis occurs with pancreatitis via? proteolytic enzymes from neutrophils liquefy parenchyma 107. Localized amyloidosis amyloid deposition usually localized to a single organ 108. loss of the nucleus, occurs via? 1. nuclear condensation = pyknosis 2. fragmentation = karyorrhexis 3. dissolution = karyolysis 109. Low ATP disrupts key cellular functions, including? 1. Na+/K+ pump 2. Ca+ pump 3. Aerobic glycolysis Lysosome membrane damage results in? hydrolytic enzymes leaking into the cytosol -> activated by the high intracellular calcium 111. Medullary carcinoma of the thyroid calcitonin deposits within the tumor 112. mesenchymal tissue can undergo? metaplasia 113. Metaplasia change in stress on an organ that leads to a change in cell type 114. metaplasia most commonly involves? change of one type of surface epithelium to another 115. Metaplasia occurs via? reprogramming of stem cells = produce the new cell type 104. 110. never physiologic 122. neurons are highly susceptible to? ischemic injury 123. Non-insulindependent diabetes mellitus (type 2) amylin deposits in the islets of the pancreas 124. partial reduction of O2 yields to? 1. superoxide (O2) 2. hydrogen peroxide (H2O2) 3. hydroxyl radicals (OH) 125. pathologic generation of free-radicals arises with? 1. ionizing radiation 2. inflammation 3. metals 4. drugs and chemicals 126. pathologic hyperplasia can progress to? dysplasia -> cancer 127. permanent tissues undergo? only hypertrophy 128. physiologic generation of free radicals occurs during? oxidative phosphorylation 129. plasma membrane damage results in? 1. cytosolic enzymes leaking into the serum 2. additional calcium entering the cell 130. Primary amyloidosis systemic deposition of AL amyloid, which is derived from immunoglobulin light chain 131. Primary amyloidosis is associated with? plasma cell dyscrasias 132. Proteases break down the cytoskeleton 133. reperfusion injury is? return of blood to ischemic tissue 149. vitamin A is necessary for? results in production of O2 derived-free radicals 134. reperfusion injury leads to? continued rise in cardiac enzymes after reperfusion of infarcted myocardial tissue 135. Saponification is an example of? dystrophic calcification, in which calcium deposits on dead tissues 136. Senile cardiac amyloidosis non-mutated serum transthyretin deposits in the heart 137. shared features of amyloid, include? 1. beta-pleated sheet configuration 2. congo red staining and applegreen birefringence when viewed microscopically under polarized light differentiation of specialized epithelial surfaces ex: conjunctiva covering the eye 150. What are examples of metal carrier proteins used in the elimination of free radicals transferrin and ceruloplasmin 151. what are free radicals? chemical species with an unpaired electron in their outer orbit 152. what generally occurs together? hyperplasia and hypertrophy 153. What is a characteristics of coagulative necrosis? ischemic infarction of any organ except the brain 154. what is an example of acute ischemia? renal artery embolus 155. what is an example of slow developing ischemia? renal artery atherosclerosis 156. What is the hallmark of reversible injury? cellular swelling 157. what leads to the inactivation of Bcl2? 1. cellular injury 2. DNA damage 3. decreased hormonal stimulation 158. What occurs in ubiquitinproteosome degradation? intermediate filaments of the cytoskeleton are "tagged" with ubiquitin 138. shock occurs with? generalized hypotension, resulting in poor tissue perfusion 139. slow developing ischemia results in? atrophy 140. superoxide dismutase results in? H2O2 141. swelling of the rough endoplasmic reticulum (RER) results in? 1. dissociation of ribosomes 2. decreased protein synthesis 142. Systemic amyloidosis? amyloid deposition in multiple organs 143. Systemic amyloidosis can be divided into? primary amyloidosis secondary amyloidosis 159. the two mechanisms of cell death, are? 1. necrosis 2. apoptosis When a dying cell shrinks, what happens? cytoplasma becomes more eosinophilic 160. Ultimately, what is the end result in ubiquitinproteosome degradation? it is destroyed by proteosomes why does high altitude cause hypoxemia? decreased barometric pressure, results in decreased PAO2 161. why does hypoventilation cause hypoxemia? increased PACO2, results in decreased PAO2 146. ultimately what will happen bc of Carbon tetrachloride (CCL4) ribosomes will detach and impair protein synthesis 162. why does the diffusion defect cause hypoxemia? 147. Under persistent stress, metaplasia can progress to? dysplasia -> cancer PAO2 not able to push as much O2 into the blood due to thicker diffusion barrier 163. why does V/Q mismatch cause hypoxemia? vitamin A deficiency can also result in? metaplasia blood bypasses oxygenated lung or oxygenated air cannot reach the blood 164. why do permanent tissues only undergo hypertrophy? they cannot make new cells 144. 145. 148.