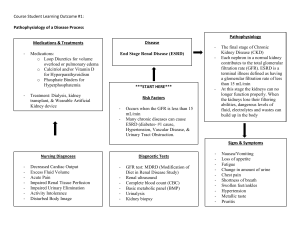
Module 1 Study Guide Nursing 210 Renal Failure: pg 397 Define Acute Renal Failure. ARF (or Acute Kidney Injury/AKI) is a rapid decline in renal function, particularly the glomerular filtrations rate (GFR), due to a decrease in the excretion function of the kidneys with concurrent increases in creatinine and urea levels. Sudden interruption of kidney function resulting from obstruction, reduced circulation, or disease of the renal tissue. Results in retention of toxins, fluids, and end products of metabolism. Usually reversible with medical treatment. May progress to end stage renal disease, uremic syndrome, and death without treatment Affects 13–18% of admitted patients. Most common causes: ischemia, falls in BP or blood volume can cause kidney tissue ischemia; exposure to nephrotoxins damaging nerves or nerve tissue; other causes: major surgery, sepsis, severe pneumonia Causes of Acute Kidney Injury Cause Prerenal most common; affects renal blood flow and perfusion Intrarenal acute damage to renal parenchyma and nephrons Postrenal least common; obstructive causes Examples Hypovolemia Low Cardiac Output Altered vascular resistance -Hemorrhage, dehydration, excess fluid loss from GI tract, burns, wounds -Heart failure, cardiogenic shock -Sepsis, anaphylaxis, vasoactive drugs Glomerular/microvascular injury Interstitial nephritis -Glomerulonephritis, disseminated intravascular coagulation, vasculitis, hypertension, toxemia of pregnancy, hemolytic uremic syndrome -Ischemia from conditions associated with prerenal failure; toxins, such as heavy metal drugs; hemolysis (RBC breakdown); rhabdomyolysis (muscle cell breakdown) -Acute pyelonephritis, toxins, metabolic imbalances, idiopathic Ureteral obstruction Urethral obstruction -Calculi, cancer, external compression -Prostatic enlargement, calculi, cancer, stricture, blood clot Acute tubular necrosis Identify the shifts in electrolytes usually present with acute renal failure. During maintenance phase, salt and water retention cause edema, increasing heart failure and pulmonary edema risks. Hyponatremia is a common cause from water excess. Impaired potassium excretion leads to hyperkalemia. When higher than 6.0–6.5 mEq/L, manifestations include muscle weakness, nausea and diarrhea, electrocardiographic changes, and possible cardiac arrest. Hyperphosphatemia and hypocalcemia also included with AKI. Metabolic acidosis results from impaired hydrogen ion elimination by the kidneys Normal sodium level = 135–145 mEq/L Normal potassium level = 3.5–5.3 mEq/L Normal GFR = > 90 mL/min in adults Identify risk factors for acute renal failure. Major trauma or surgery, infection, hemorrhage, severe heart failure, severe liver disease, and lower urinary tract obstruction. Drugs and radiologic contrast media that are toxic to the kidney also increase the risk for AKI. Older adults develop AKI more frequently due to higher incidence of serious illness, hypotension, major surgeries, diagnostic procedures, and treatment with nephrotoxic drugs. Kidney function decreases with age also put older adults at greater risk Children with renal insufficiency (decrease in ability to conserve sodium and concentrate the urine) at greater risk for fluid loss with illness. In cases of acute GI illness, children at greater risk for dehydration and AKI. Explain the meaning of GFR and BUN/Creatinine. GFR = glomerular filtration rate, the rate which fluid is filtered through the kidneys. GFR helps determine the stage of kidney damage or disease. Stage Description pg 416 GFR Kidney damage (i.e. protein in urine) with normal GFR 1 90 or above Kidney damage with mild decrease in GFR 2 60 – 89 Kidney damage with moderate decrease in GFR 3 30 – 59 Kidney damage with severe decrease in GFR 4 15 – 29 Kidney failure 5 below 15 BUN/creatinine = blood urea nitrogen, the end product of protein metabolism / product of creatinine phosphate breakdown from muscle and protein metabolism. Used to evaluate renal function. In AKI, serum BUN/creatinine levels increase rapidly, within 24–48 hours from onset, due to the kidneys inability to filter adequately. Creatinine levels generally peak within 5–10 days. BUN/creatinine levels tend to increase more slowly when urine output is maintained. Onset of recovery marked by a halt in the rise of serum creatinine and BUN. Normal BUN = 7–20 mg/dL. Normal creatinine = 0.8 – 1.2 mg/dL. Give an example of pre-renal, intra-renal and post-renal failure. Prerenal: hypovolemia from hemorrhage Intrarenal: acute tubular necrosis from rhabdomyolysis Postrenal: urethral obstruction via calculi List and describe the 3 stages of Acute Kidney Injury. 1. Initiation: may last hours to days. Begins with initiating event (i.e. hemorrhage) and ends when tubular injury occurs. If AKI is recognized and initiating event is treated effectively in this phase, prognosis is good. Often asymptomatic phase making AKI identification difficult before going into maintenance phase. 2. Maintenance: found with significant fall in GFR and tubular necrosis. Oliguria may develop, although many patients continue to produce normal/near normal urine amounts (nonoliguric AKI). Even though urine may be produced, the kidney cannot efficiently eliminate metabolic wastes, water, electrolytes, and acids from the body in this phase of AKI. Azotemia, fluid retention, electrolyte imbalances, and metabolic acidosis develop. Greater negative prognosis with oliguria. salt and water retention cause edema, increasing heart failure and pulmonary edema risks. Hyponatremia is a common cause from water excess? Impaired potassium excretion leads to hyperkalemia. When higher than 6.0–6.5 mEq/L, manifestations include muscle weakness, nausea and diarrhea, electrocardiographic changes, and possible cardiac arrest. Hyperphosphatemia and hypocalcemia also included with AKI. Metabolic acidosis results from impaired hydrogen ion elimination by the kidneys. Anemia develops after several days of AKI from suppressed renal erythropoietin production. Immune function may be impaired, increasing risk for infection. Other s/sx include: confusion, disorientation, agitation, lethargy; hyperreflexia; possible seizures or coma from azotemia and electrolyte imbalances. Anorexia, nausea, vomiting, decreased or absent bowel sounds. Uremic syndrome if AKI is prolonged. 3. Recovery: tubule cell repair and regeneration and gradual return of the normal GFR or pre-AKI levels. Diuresis may occur with recovering renal function but serum creatinine, BUN, potassium, and phosphate levels may remain high or continue to rise. Renal function improves rapidly during the first 5–25 days and continues for up to 1 year. Explain the rationale for using Kayexalate (sodium polystyrene sulfonate) with renal failure. Not used to replace an electrolyte but to remove excess potassium from the body by exchanging sodium for potassium in the large intestine, since hyperkalemia is seen in AKI patients. Explain the rationale for using calcium acetate with renal failure. Binds to dietary phosphate to form an insoluble calcium phosphate complex, which is excreted in the feces, resulting in decreased serum phosphorus concentrations, since hyperphosphatemia is seen in AKI patients. Explain the rationale for avoiding salt substitutes with renal failure. Many salt substitutes contain high levels of potassium and, if the AKI patient is already experiencing hyperkalemia, your continuing to increase your serum potassium dietarily which will further advance kidney damage or disease. Explain the rationale for using IV regular insulin with renal failure. If the AKI patient is experiencing hyperkalemia, IV regular insulin has properties to shift extracellular potassium into the cells to reducing the serum potassium. Identify the types of diuretics and explain the differences. Loop diuretics are the most potent diuretics as they increase the elimination of sodium and chloride by primarily preventing reabsorption of sodium and chloride. The high efficacy of loop diuretics is due to the unique site of action involving the loop of Henle (a portion of the renal tubule) in the kidneys. Thiazide diuretics increase the elimination of sodium and chloride in approximately equivalent amounts. They do this by inhibiting the reabsorption of sodium and chloride in the distal convoluted tubules in the kidneys. In the distal tubule, potassium is excreted into the forming urine coupled with the reabsorption of sodium. Potassium-sparing diuretics reduce sodium reabsorption at the distal tubule, thus decreasing potassium secretion. Potassium-sparing diuretics when used alone are rather weak, hence they are used most commonly in combination therapy with thiazide and loop diuretics. Carbonic anhydrase inhibitors work by increasing the excretion of sodium, potassium, bicarbonate, and water from the renal tubules Osmotic diuretics are low-molecular-weight substances that are filtered out of the blood and into the tubules where they are present in high concentrations. They work by preventing the reabsorption of water, sodium, and chloride. Explain how renal failure affects RBC production. The kidneys normally produce erythropoietin, a hormone necessary for RBC production. If the kidneys are damaged erythropoietin may decrease, thus decreasing RBC production. List the most common causes of chronic kidney disease. Cause Diabetic nephropathy #1 Hypertensive nephrosclerosis #2 Chronic glomerulonephritis Chronic pyelonephritis Polycystic kidney disease Systemic lupus erythematosus Examples Initial increases in GFR lead to hyperfiltration with eventual glomerular damage with thickening and sclerosis of the glomeruli; gradual destruction of the nephrons lead to GFR fall Chronic HTN leads to sclerosis and narrowing of renal arterioles & small arteries, reducing blood flow, leading to ischemia, glomerular destruction, and tubular atrophy. Chronic interstitial inflammation of parenchyma leads to tubule and capillary obstruction and damage, affecting GFR and tubular secretion and reabsorption, with gradual loss of entire nephrons. Chronic infection leads to scarring and deformity of renal calyces and pelvis. Multiple bilateral cysts gradually compress renal tissue, impairing renal perfusion and leading to ischemia, renal vascular remodeling, and release of inflammatory mediators, which damage and destroy normal renal tissue. Immune complexes form in capillaries leading to inflammation and sclerosis, creating glomerulonephritis List the clinical manifestations of chronic kidney disease. Etiology Manifestations Uremia: syndrome or group of symptoms related to ESRD. - hyperparathyroidism - glucose intolerance - pulmonary edema - pleuritis - Kussmaul respirations - proteinuria, hematuria, oliguria, nocturia - fixed specific gravity - anorexia, N/V, gastroenteritis - hiccups - ABD px, peptic ulcer, GI bleeding - Uremic factor/urine-like breath - osteodystrophy, bone pain, spontaneous fx - apathy, lethargy, headache, impaired cognition, insomnia, restless leg syndrome, gait disturbances - HTN, edema, CAD or failure - Anemias, impaired clotting - Pallor, uremic skin color, poor turgor Anemia - fatigue - pallor - dizziness, confusion, lethargy - tachycardia, tachypnea, hypotension Therapies - Serum electrolytes, BUN, creatinine, arterial blood gas (pH), lipid level monitoring - Cardiorespiratory monitoring - Accurate I&O - Diuretic administration - Fluid restriction - Dietary consult to improve nutrition status - Dialysis (often the only option) - Iron supplementation - Epoetin administration - Blood transfusion - Treating underlying cause of renal failure Fluid volume excess - dependent pitting edema - respiratory crackles - dyspnea, pulmonary edema, hypoxemia - weight gain - tachycardia - jugular vein distension - Fluid restriction - Sodium-restricted diet - Diuretics - Dialysis Hyperkalemia - ventricular arrhythmias - tall, peaked T waves; widened QRS - cardiac arrest - smooth muscle hyperactivity - nausea, vomiting, diarrhea - abdominal cramping - muscle weakness, paresthesias, flaccid paralysis - Removal of all potassium from IV solutions - Low potassium diet - Admin. glucose and insulin - K+ absorbing enemas - Dialysis Explain the rational for prescribing RAS suppressing medications to someone with chronic kidney disease. Patients with chronic kidney disease, especially that undergoing dialysis and having secondary hyperparathyroidism, have a high risk of bone fracture. The renin-angiotensin system (RAS) is associated with osteoclastic bone resorption, reducing fracture-related hospitalizations of dialysis patients. Explain how peritoneal dialysis works. A cleansing fluid flows through a tube (catheter) into part of your abdomen. The lining of your abdomen (peritoneum) acts as a filter and removes waste products from your blood. After a set period of time, the fluid with the filtered waste products flows out of your abdomen and is discarded. Discuss how to assess a dialysis shunt. Examine the integrity of the skin overlying the fistula, which should appear normal without erythema, focal masses, or focal swelling. Cannulation sites should be well healed with minimal to no scabbing and no evidence of inflammation. Palpate the vascular access to feel for a thrill or vibration that indicates arterial and venous blood flow and patency. Auscultate the vascular access with a stethoscope to detect a bruit or "swishing" sound that indicates patency. Patency should be checked every 8 hours. List foods high in potassium. Bananas, avocados, raisins, prunes and prune juice, oranges and orange juice, tomatoes, tomato juice, and tomato sauce, lentils, spinach. List foods high in sodium. Processed meats, chicken, burritos, pizza. Infectious Lung Disease and Sepsis: pg 606-612, 622-636, 636-642 Explain the pathophysiology of septic shock. Systemic inflammatory response syndrome (SIRS, sepsis precursor) describes the body’s response to a critical illness, that can result from infectious or non-infectious cause, precipitating a whole-body inflammatory process. Infection-related SIRS triggers a systemic inflammatory response that leads to a series of adverse events, including vasodilation, increased capillary permeability, and hypercoagulability. Also, it triggers many immune/inflammatory cells like platelets, neutrophils, macrophages, and endothelial on a body-wide scale; where, during SIRS, those cell’s functions are exaggerated and the uncontrolled cellular release of chemical mediators is global. When the SIRS response is severe, sepsis can develop. Sepsis is a SIRS resulting from an infection. Disseminated intravascular coagulation (DIC) is associated with sepsis and is a state of simultaneous bleeding and clotting throughout the vasculature. Sepsis injures blood cells, causing platelet aggregation and decreased blood flow, resulting blood clots form throughout the microcirculation. The clotting slows circulation further while stimulating excess fibrinolysis. As the body’s stores of clotting factors are depleted, generalized bleeding begins. Further sepsis progression may lead to severe sepsis, where organ perfusion is reduced can cause multiple-organ dysfunction (MOD), and eventually death. Septic shock is a persistently low mean arterial pressure (MAP) from overwhelming infection despite fluid resuscitation. Blood pools in the extremities, blood flow becomes sluggish, and amounts of oxygen received by the tissues are inadequate for cell metabolism. Manifestations of Septic Shock Early (warm) Septic Shock - Blood pressure: normal to hypotension - Pulse: increased, thread - Respirations: rapid and deep - Skin: warm, flushed - Mental status: alert, oriented, nervous - Urine output: normal - Other: increased body temp; chills; weakness; N/V/D; decreased central venous pressure (CVP) Late (cold) Septic Shock - Blood pressure: hypotension - Pulse: tachycardia, arrhythmias - Respirations: rapid, shallow, dyspneic - Skin: cool, pale, edematous - Mental status: lethargic to comatose - Urine output: oliguric to anuria - Other: normal to decreased body temp; decreased central venous pressure (CVP) Discuss the effects of sepsis upon metabolism. Sepsis is associated with a state of simultaneous bleeding and clotting (DIC) which ultimately leads to injured RBC’s, generalized bleeding, clot forming, sluggish blood flow and blood pooling. This leads to a significant decrease in amounts of oxygen received by the tissues inadequate for cell metabolism. Discuss signs of systemic infection vs. local infection. Local: redness, swelling, pain, possible purulent exudate and/or tissue necrosis Systemic: fever or hypothermia, shaking or chills; warm or clammy/diaphoretic skin; fatigue, headache, N/V/D, decreased LOC, lethargic; hyperventilation; tachycardic Describe the clinical picture of sepsis. Fever or hypothermia, shaking or chills; warm or clammy/diaphoretic skin; fatigue, headache, N/V/D, decreased LOC, lethargic; hyperventilation; tachycardic; peripheral vasodilation; septic shock Increase in cardiac output Abnormal CBC (leukocytosis or leukopenia) and alteration in clotting factors (thrombocytosis or thrombopenia) results in DIC. Elevated liver enzyme C-reactive protein and creatinine likely. Hypophosphatemia and positive blood cultures anticipated. Discuss the ways in which one can develop pneumonia. The pathogenic process, anatomical location, and manifestations vary depending on infecting organism. Can be viral, bacterial, fungal, protozoan, or noninfectious. Bacterial pathogens circulate through bloodstream to the lungs and damage cells, where cellular debris and mucus cause airway obstruction. Bacteria tend to be distributed evenly throughout one or more lobes of a single lung (unilateral lobar pneumonia). Pneumococcal is most common Viral pathogens frequently enter from the upper respiratory tract, infiltrating the alveoli nearest the bronchi of one or both lungs. There, they invade cells, replicate, and burst out forcefully, killing the host cells and sending out cell debris. They rapidly invade adjacent areas, distributing themselves in a scattered/patchy pattern (bronchopneumonia) Patterns of Lung Involvement pg 623 Pattern Lobar pneumonia Description Typically involves entire lobe as bacteria rapidly spreads throughout evenly (diffuse). An immune response ultimately creates consolidation/solidification of lung tissue and purulent exudate creating excessive edema and congestion. Bronchopneumonia Involves dependent lung portions/patchy pattern(s). Exudate found in bronchi/bronchioles, with less edema and congestion than lobar pneumonia. Interstitial pneumonia Involves interstitium (alveolar walls and connecting tissue supporting bronchial tree). May be patchy or diffuse. Less exudate but increased amount of protein-rich hyaline membranes may line alveoli, interfering with gas exchange. Miliary pneumonia Spread to the lungs via bloodstream causes numerous discrete inflammatory lesions. Primarily seen in severely immunocompromised patients, thus pleural tissue damage may be severe. Explain the reasons children are more susceptible to pneumonia. Immature airway and lungs make children more susceptible due to smaller size of airways, less number of alveoli, differential use of muscles for breathing. Higher oxygen consumption since children have a greater metabolic rate, and increases further under respiratory distress. They have fewer muscle glycogen reserves which lead to more rapid muscle fatigue when using accessory muscle for breathing (bad sign). Both result in quicker hypoxia in children than adults. Nasal flaring, tachypnea, retractions, and increased breathing effort may tire an infant or young child and result in periods of apnea (oh shit). Explain the reasons the elderly are more susceptible to pneumonia. Decreased number of cilia, gag and cough reflex diminishes. Greater risk for dehydration, leading to thickened mucus that’s difficult to expel. Declining immune function Other: polypharmacy, immobility, health history/surgeries, malnutrition, comorbidities. Discuss methods of preventing pneumonia. Early identification of vulnerable populations and instituting preventative measures Early identification of infecting organism, appropriate treatments Vaccines if possible. Yearly vaccines if possible Standard precautions if possible. Avoid sick family/friends Explain the “shift to the left.” When the CBC with differential shows many immature neutrophils (bands) created by the bone marrow quickly in response to infection or inflammation. The body is now producing large amounts of new neutrophils in preparation to fight off a newly discovered bacterial infection. List nonpharmacological therapy that might benefit someone with pneumonia. Incentive spirometry Suctioning Chest physiotherapy Promote fluid intake to at least 2500–3000 mL/day minimize fatigue, take breaks Optimize nutrition Discuss methods of preventing the spread of influenza. Vaccines if possible. Yearly vaccines if possible Standard precautions if possible. Avoid sick family/friends Who should/should not be vaccinated against influenza? Should At risk patients/people o People 65 and older. o Nursing home residents. o Adults/children with cardiopulmonary disorders (asthma) or metabolic diseases (diabetes). o Healthcare workers. o Family of at-risk patients. Shouldn’t Children younger than 6 months. People with severe, life-threatening allergies to any ingredient in the flu vaccine (egg and anything else in it). People who’ve had a severe allergic reaction to the flu vaccine prior. Talk with Doc if experienced Guillain-Barre syndrome from previous dose. List the clinical manifestations of influenza. Rapid onset, profound malaise may develop in a matter of minutes Chills, fever, muscle aches, headache Cough, sore throat, runny nose Identify the expected outcome of WBC count in viral vs. bacterial infection. WBC count commonly decreased with viral infection WBC count commonly increased with bacterial infection Teaching and Learning & P,P,P: pg 2661 Discuss each learning theory and describe how a nurse can utilize it. Learning theory Adult learning theory Behaviorist theory Cognitive theory Constructivist theory Social learning theory Summary Implications for Teaching In contrast to children, Adults: - need to know why they should learn something - prefer being treated as capable of self-direction - have life experiences that enhance current learning - ready to learn what they must to take care of themselves Learning occurs when a person’s response to a stimulus is positive or negative, and it’s possible to alter the stimulus condition or the result after the stimulus. Providing positive reinforcement is helpful Learning involves three mental processes: acquiring, processing, and using information. A person’s learning capacity is shaped by her developmental level and by social, emotional, and physical contexts in learning. With adults, communicate how/why they need to learn something. Respect their independence, competency. Use their previous experiences to build on new info Learning is based on one’s personal experiences. Learning is on ongoing buildup and accommodation of new experiences and interpretations. Cooperative learning and problem solving is helpful. Learning from instruction and observation of others. Process focuses on imitation and modeling. Acknowledge importance of and build on the learner’s experiences. Encourage the learner to engage with the RN and others in the learning process. Instruct the learners how to do something and ask them to repeat it. Provide praise or encouragement after each phase of the learning process. Allow sufficient time for the learner to practice new skills. Develop strategies to meet each learner’s unique learning style and preferences. Assess each of their developmental stage, emotional readiness to learn, and adapt teach style to accommodate. List general guidelines for teaching. Effective teaching: - holds the learner’s interest - involves the learner - is age, condition, ability appropriate - sets realistic goals - foster’s a positive self-concept in feeling that learning is possible - supports with positive reinforcement and feedback - uses evidence-based information - uses several methods for learning accommodation and evaluation - is cost effective Discuss documentation that should occur following teaching. Document in patient chart using ADPIE format? Discuss the types of learning styles and how to reach target each style. Define the term “nursing diagnosis”. List and explain different frameworks that may be used with prioritizing problems. Informatics: Explain how the nurse uses a clinical decision support system and what it can provide. Discuss device integration and its benefits. Give an example. Managing Care: Discuss each framework for nursing care delivery. Discuss the role of a case manager. Care Coordination and Cost Effective Care: Describe the role of a case manager. Define care coordination. Define collaboration. Discuss barriers to effective care coordination. List health care values in the US that differ from other developed countries. Discuss what is meant by: nursing shortages are cyclic in nature. List examples of ways that nurses can provide cost conscious nursing.