EKG Rhythm Cheat Sheet: Basics, Interpretation, & Dysrhythmias
advertisement

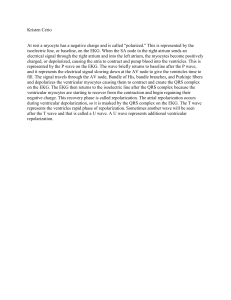
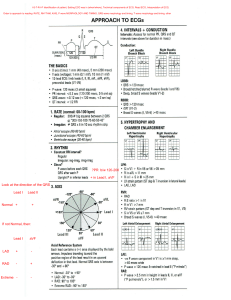
CARDIOVASCULAR EKG BASICS - 1 large box = 0.20 seconds 5 large boxes = 1 second 1 small box = 0.04 seconds WAVEFORMS 1. P wave - upright and rounded; should not be longer than 0.10 seconds - Represents the SA node sending out an electrical impulse & atrial depolarization (squeeze) - P wave present = SA node is working & will have regular rhythm 2. QRS complex - tall and pointy, we DO NOT want a wide QRS (means something is wrong) - Represents ventricular depolarization - Ventricle contraction (squeeze) (in ST segment) 3. T wave - upright and rounded - Represents ventricular repolarization (ventricles relaxing/refilling with blood) - Helpful in monitoring extreme electrolyte imbalances (hypo/hyperkalemia, issues with myocardial oxygen supply, or other cardiac disturbances such as pericarditis or ventricular aneurysm) ABNORMAL: 4. U wave - small, rounded wave after the T wave - Common with drug toxicities (ex. digoxin) & electrolyte imbalances (hypokalemia) INTERPRETING EKG’S 1. 2. Count the HR Is it regular or irregular? - Ensure that the strip is 6 seconds long (30 large boxes) To count HR, count the R’s and multiply by 10 (ex. 6 R’s = 60 bpm) P wave present = regular rhythm One P wave for every QRS complex No wide QRS’s! MEASURING INTERVALS: Measures the amount of time it takes for the impulse to travel from one wave to the next - - - P-R interval - movement of electrical activity from atria → ventricles - Beginning of P wave to beginning of QRS complex - Reflects the time required for atrial depolarization - Should be between 0.1 and 0.2 seconds (not bigger than 1 large box) - Most commonly measured QRS interval - ventricular depolarization - Beginning of Q to top of S (where it begins to flatten) - Should be between 0.06 and 0.10 seconds QT interval - time it takes for the ventricles to depolarize, contract, and repolarize - Beginning of Q to end of T (bottom of hill) - Should be less than 0.52 seconds - Usually measured with magnesium-related issues, not on a regular basis RHYTHMS Normal Sinus Rhythm - Normal sinus rhythm is generated by the SA node (sinus node) HR: 60-100 bpm 1 consistent P wave for every QRS complex SINUS DYSRHYTHMIAS Symptoms: ● Hypotension ● Dizziness ● Lightheadedness ● Fatigue ● Syncope (fainting)/change in LOC ● SOB ● Diaphoresis (sweating) ● Anxiety ● Palpitations/chest pain ● Restlessness *NOTE: only treat symptomatic patients as it may be their normal for some patients and they might just require observation Sinus Bradycardia: the sinus node creates an impulse at a slower-than-normal rate - - HR: < 60 bpm Rhythm: regular P wave: upright and rounded Causes: lower-metabolic needs (sleep, athletic training, hypothyroidism, hypoxia, hypothermia, hypotension, declining towards death) Treatment: - Vitals - 12-lead EKG - Obtain IV access - Oxygen - Eventually may need pacemaker (TCP) if HR remains too low after medication & Pt can’t tolerate Meds: - Atropine → 0.5 mg IV push - Works on SA node - After administration, get another BP, watch the HR, and maybe another EKG *REMEMBER: medication is the LAST treatment option! Need vitals first in order to determine pulse ox for necessary oxygen, etc. Sinus Tachycardia: the sinus node creates an impulse at a faster-than-normal rate - - HR: > 100 bpm Rhythm: regular P wave: upright and rounded Causes: anemia, fever, hypovolemic shock, hypotension, PE, MI, pain, anxiety, illicit drugs, caffeine/stimulants, dehydration, hemorrhaging, sepsis/infection, electrolyte imbalances, stress, HF, physical activity, fear, cardiac tamponade Treatment: treat the cause! (tachycardia is a secondary issue from something else) Meds: - Maybe beta blockers to slow the HR ATRIAL DYSRHYTHMIAS Premature Atrial Contraction (PAC): abnormal contractions caused by pacemaker cells firing too early - Rhythm: irregular P wave: appears prematurely Treatment: - Vitals, 12 lead EKG, IV access, oxygen - Document - Treat the cause (decrease stress, avoid alcohol and caffeine) *Not really a whole lot to do Afib: SA node not working, causing uncoordinated electrical activity in the atria, which causes rapid & disorganized “fibbing” or “quivering” of the muscles, instead of fully squeezing → decreased cardiac output *NOTE: this causes blood to collect in the atria, placing the patient at HIGH RISK FOR CLOTS & STROKE *MEMORY TRICK: when you fib, your lip quivers - HR: 300-600 bpm (unmeasurable) - Rhythm: irregular - P wave: absent (just see waves/quivering) - Causes: other cardiac/pulmonary conditions (cardiomyopathy, pericarditis, HTN, CAD, HF, open heart surgery), obesity, CKD, hyperthyroidism, diabetes - Symptoms: all due to low O2 → fatigue, dizziness, lightheadedness, SOB, chest pain, tachycardia, palpitations, anxiety, diaphoresis (depending on how high HR is) - Treatment: - Controlled (60-80 bpm): vitals, EKG, etc. & continue with their meds - Uncontrolled (> 140 bpm): - Vitals, 12 lead EKG, IV access, oxygen - Meds - Cardiac ablation (rhythm control) - Cardioversion → synchronized administration of shock to R wave; stops heart for about 6 seconds via SA node to restart and get a new, normal rhythm. - This is NOT defibrillation *NOTE: VERY UNCOMFORTABLE FOR PATIENT → GIVE PAIN MEDS PRIOR - Meds: - Control the HR (PRIORITY after vitals): - Beta blockers - Calcium channel blockers - Digoxin - Control the rhythm: (antiarrhythmics) - Amiodarone - Nicardipine (Cardene) - ??? - Anticoagulants (for life or until resolved) - Apixaban (Eliquis) Aflutter: similar to Afib, but not produced by the SA node. The atria are beating too quickly but at a regular rhythm - HR: 250-350 bpm Rhythm: regular P wave: not distinct, P & T run together; “sawtooth” Causes: same as Afib Symptoms: same as Afib Treatment: same as Afib Meds: same as Afib SVT: abnormally fast HR that originates above the ventricles, typically in the atria. Very narrow QRS complex *MEMORY TRICK: supra=above - HR: > 100 bpm (typically 150-250) - Rhythm: regular - P wave: typically not visible (may be hidden in preceding T wave, check T wave for change in shape) - Causes: caffeine, stimulants, drugs, sometimes cause is just unknown - Symptoms: dizzy, lightheadedness, SOB, chest pain, palpitations, anxiety, sweating, “my heart is flopping like a fish”, hypotensive (BP drops with high HR bc body doesn’t like that your heart is so fast) - Treatment: - PRIORITY → vitals, 12 lead EKG, IV access, oxygen - Vagal maneuvers (bearing down like BM, blow through occluded straw, or bucket of ice in face) → want to initiate gasp to restart SA node - Meds - Cardiovert - Meds: - Adenosine → 6mg, 12mg, 12mg (STOPS THE HEART AND RESTARTS SA NODE = FLATLINE) - MUST GET BP BEFORE ADMINISTERING -- drops BP very quickly - Do not give more than 3 times - Most ideal because it works very quickly (< 6 seconds) - *NOTE: if Pt is hypotensive (< 100), CANNOT give Adenosine; MUST CARDIOVERT - If Adenosine doesn’t work → cardioversion - If cardioversion doesn’t work → Amiodarone (works slower than Adenosine) - Beta blockers/calcium channel blockers VENTRICULAR RHYTHMS Premature Ventricular Contractions (PVC’s): wide and atypical (or bizarre-looking) QRS complexes that fire earlier than expected. Could be upright or inverted, followed by a short pause *NOTE: PVC’s can turn into Vtach (> 150 bpm) = deadly → watch for chest pain (notify HCP) - Rhythm: irregular (or “regular except” with PVC) - Unifocal: PVC coming from 1 ventricular pacemaker - Bifocal (or multifocal): PVC coming from 2 (or more) different parts of the ventricle - Bigeminy: PVC that occurs every other beat (beat, PVC, beat, PVC) - Trigeminy: PVC falling every third beat (beat, beat, PVC) - P wave: normal except PVC (no P wave with PVC) - Causes: increased workload on the heart -- hypoxia, electrolyte imbalances, MI, cardiomyopathy, excessive stimulant ingestion, HTN, recreational drug use/drug toxicity - Symptoms: may be asymptomatic - Treatment: - Vitals, 12 lead EKG, IV access, oxygen - Treat the underlying cause (have to figure out why they’re getting PVC’s) - Stimulant/caffeine → wait until it wears off - May need to ask -- How big was your coffee? How many cups did you drink? Did you have chocolate? Sudafed? Etc. Vtach: three or more PVC’s in a row; wide, consistent, QRS complexes. Can have a pulse or be pulseless. No cardiac output (= low oxygen) or contractions which may be fatal! *MEMORY TRICK: looks like tombstones - HR: > 150 bpm - Rhythm: regular - P wave: not visible - Causes: multiple PVC’s, drug toxicities, caffeine/stimulants, hypoxia, acidosis, hypo/hyperkalemia, hypothermia, hypoglycemia, cardiac tamponade, PE, MI - Symptoms: - PULSE: - Awake (Vfib is always pulseless) - C/O chest pain, SOB, palpitations, sweaty, anxious, maybe hypotensive or maybe normal BP (depending on how long you’re in it) - PULSELESS: - Dead, need to be resuscitated - Treatment: - PULSE: - Vitals, 12 lead EKG, IV access, oxygen - Need to change rhythm → vagal maneuvers, cardioversion, Amiodarone - PULSELESS: - CPR + defibrillation - Epinephrine, Amiodarone Vfib: rapid, disorganized pattern of multiple sources of electrical activity in the ventricles. Prevents ventricles from pushing blood out of the heart (no cardiac output = no oxygen in the body). Shaky/quivering line. A lethal dysrhythmia requiring immediate treatment -- LIFE-THREATENING - HR: ALWAYS PULSELESS - Rhythm: cannot assess - P wave: no P waves, QRS complexes, or T waves - Causes: illicit drug use, MI (most common rhythm seen with MI’s), same as Vtach - Symptoms: loss of consciousness, pulseless - Treatment: CPR + defibrillation *MEMORY TRICK: defib Vfib - Meds: - Vasopressor → epinephrine - Antiarrhythmic → amiodarone Idioventricular Rhythm: occurs when the SA and AV nodes fail to function and the rhythm is generated from the ventricles - HR: < 40 bpm - Rhythm: regular - P wave: no P or T waves; wide QRS - Causes: MI, post-cardiac arrest, drug toxicity (cocaine, digoxin, anesthetics), severe electrolyte imbalances, myocarditis, cardiomyopathy, congenital heart disease - Symptoms: - Dizzy/lightheadedness - SOB - Syncopal episode - Sweaty - Anxiety - Hypotension - Decreased LOC - Treatment: - Vitals, 12 lead EKG, IV access, oxygen - Treat the cause - Prepare for pacemaker Asystole: FLATLINE - no electrical activity in the heart - Symptoms: no response from patient, pulseless Treatment: 1. See flatline on monitor → check for pulse (to ensure flatline is not caused by loose ECG patch/wire) 2. No pulse? → immediately start CPR *NOTE: NO defibrillation (nothing to defibrillate) 3. Pause compressions briefly (< 10 seconds) to rule out a fine line VFib by placing a second monitor lead. ONLY if it is VFib → THEN defibrillate - 4. Meds: - Ensure IV access for epi Epinephrine HEART BLOCKS - Caused by the delay or blockage of electrical conduction at the AV node When identifying heart blocks, look at the P-R interval pattern First Degree: prolonged atrial depolarization in the AV node. Every atrial impulse gets through the AV node; it just takes longer. It is the same interval each time *MEMORY TRICK: If the R is far from the P, then you have FIRST DEGREE - Looks very similar to NSR - only difference is P-R interval is > 0.20 seconds (1 large box) - Rhythm: regular - P wave: upright & rounded - Symptoms: typically asymptomatic - Treatment: not typically required - Vitals, 12 lead EKG, IV access, oxygen - Find/treat underlying cause Second Degree - Type I (AKA Wenckebach or Mobitz I): occurs when not all atrial impulses get through the AV node to the ventricles. There are more P waves than QRS complexes *MEMORY TRICK: longer, longer, longer, DROP. Then you have a WENCKEBACH - Rhythm: regular - P wave: upright & rounded; P-R interval gets progressively longer until a QRS is dropped - Symptoms: dizzy, lightheadedness, diaphoresis, syncope, anxiety, hypotension, SOB - Treatment: - Asymptomatic: - Vitals, 12 lead EKG, IV access, oxygen - Symptomatic: - Atropine → stimulates heart to beat faster - Prepare for temporary pacemaker → Transcutaneous pacing (TCP) Second Degree - Type II (AKA Mobitz II): sudden failure of impulse conduction from atria to ventricles. Also drops QRS complexes, however, the P-R intervals are exactly the same length with each complex *MEMORY TRICK: if some P’s don’t get through, then you have MOBITZ II - Rhythm: regular - P wave: upright & rounded; P-R interval stays the same length until QRS is dropped - Symptoms: same as type I - Treatment: same as type I Third Degree (complete heart block): occurs when the AV node is completely blocked and prevents any impulses from entering or exiting. There is no communication between the atria and ventricles (atria is working independently). P wave to P wave will be same length apart *MEMORY TRICK: if P’s and Q’s don’t agree, then you have THIRD DEGREE - HR: atrial = 60-100 bpm; ventricular = < 60 bpm - Rhythm: regular P wave: upright & rounded; P waves are NOT associated with QRS complexes (independent); P waves may be hidden in T waves or QRS complexes → have to find them Symptoms: same as type I Treatment: - Asymptomatic: very rare - Vitals, 12 lead EKG, IV access, oxygen - Figure out cause - Symptomatic: - Vitals, 12 lead EKG, IV access, oxygen - Atropine - TCP - If above do not work → permanent pacemaker TEMPORARY PACEMAKERS - The energy source is an external battery pack Transcutaneous (TCP): electrical stimulation used for emergent situations to increase HR - Pads placed externally on the skin with one pad on the chest and one on the back (like AED pads) Sends electrical stimulation through the thoracic musculature to the heart → VERY PAINFUL Pacer spikes seen prior to QRS CONTINUOUS VITAL SIGNS AND MONITORING REQUIRED Transvenous (TVP): pacing lead wires are inserted via central line through subclavian vein so that they are in direct contact with the right atrium (atrial pacing), right ventricle (ventricular pacing), or both chambers (dual chamber pacing) - Wire connects to external box where the desired rate is set - More invasive = increased infection risk (vs. TCP) but lasts longer than TCP - May be used temporarily until Pt can go to OR for permanent pacemaker & for emergent situations - Pacer spike seen prior to QRS - CONTINUOUS VITAL SIGNS AND MONITORING REQUIRED + monitor central venous site for signs of infection Transthoracic (TTP): pacer wire is surgically placed in the atrium or ventricle and fed out through the skin to connect to external box/pacemaker (bascially same as TVP except wires are surgically placed) CONTINUOUS VITAL SIGNS AND MONITORING REQUIRED PERMANENT PACEMAKERS - Wires are placed in the atria, ventricle, or both and the wires are placed in an internal pacing unit housed under the skin near the clavicle Atrial: wire in atria - Pacer spike prior to P wave Used with SA node failure Ventricular: wire in ventricle - Pacer spike prior to QRS complex Used with a complete AV block Biventricular: pacer lead in each ventricle - Two pacer spikes prior to QRS Dual Chamber: one wire in atria, one wire in ventricle - Two pacer spikes: one before P wave and one before QRS CARDIAC DISORDERS Infective Endocarditis (IE): infection/inflammation of the endometrium (innermost layer of the heart), typically affecting heart valves - Platelet and fibrin deposit onto the injured area, forming a nonbacterial thrombotic endocardial lesion, then microogransims get stuck under lesions, forming vegetation (looks like plaque build up), which can severely damage the valves - Common microorganisms: streptococcus, staph aureus (MRSA) - Risk factors: - Age (> 60) - Immunodeficiency (can’t fight off bacteria) - IV drug use (creating a port of entry!) - Diabetes mellitus - Prosthetic heart valves - Prior history of IE - Congenital or structural heart disease - Presence of IV access or an implanted cardiac device - Symptoms: - Osler’s nodes (lymph nodes) - red, painful nodes in pads of finger & toes - Janeway lesions - painless spots on palms and soles - Splinter hemorrhages - vertical red lines under nail beds - - - - - - ELDERLY: confusion, fever, fatigue (think S/S of infection) Labs & Diagnostics: - LABS: CBC (elevated WBCs), BMP, BNP, sed rate, blood cultures (two sets from different sites) - DX: transthoracic echocardiogram (TTE) or transesophageal echocardiogram (TEE) → these show what the heart/valves look like and can identify any growth or abscesses Treatment/INT: - IV antibiotics for 4-6 weeks → will need PICC line - Valve repair/replacement - Assessments: cardiac history (previous valve replacement or invasive procedures), IV drug user, neuro, skin, lab/dx results Teaching: - Will be in hospital for a longer period of time because of abx - Once you have a valve replacement → MUST INFORM DENTIST! Bacteria will go straight to valves - Don’t create new portal of entry → be careful with brushing teeth, use soft toothbrush - Finish full course of abx *MEMORY TRICK: think endo(carditis) like endodontist Nursing Diagnosis: - Ineffective tissue perfusion - Decreased cardiac output Complications: - Embolization: those thrombotic lesions can break off and will likely travel to brain → HF & dysrhythmias Pericarditis: inflammation of the pericardium; common following an MI - - - Causes: can be infectious (viral, bacterial, fungal, or parasitic) or noninfectious (MI, drug-related, autoimmune, trauma) Symptoms: - Radiating chest pain that is relieved by sitting up and leaning forward - SOB - Palpitations - Fatigue/low energy - Abnormal EKG (ST-segment elevations or PR-segment depression) - Friction rub upon auscultation (best heard @ left sternal border at the end of expiration. Have Pt lean forward) - Decreased appetite Labs & Diagnostics: - LABS: CBC (elevated WBC’s), blood cultures (+), C-reactive protein (+), sed rate - DX: EKG, TEE or TTE, chest x-ray, cardiac CT scan - Assessments: ABC’s, vitals, heart/lungs auscultation, I&O/daily weights, lab results *Rule out MI Treatment/INT: - Elevate HOB to 30-45 degrees to relieve pressure on organs and decrease orthopnea (SOB when lying down) - Meds (pain is usually associated with inflammation) - Emotional support (may have anxiety bc of fear that pain is r/t MI) - - - - Meds: - Antiinflammatory → NSAIDs or ASA; maybe corticosteroids - Diuretic - Nitro - Calcium channel blockers (depending on BP) Nursing Diagnosis: - Acute pain - Risk for decreased cardiac output Teaching: - Med compliance! - S/S of MI vs. S/S of worsening pericarditis → if symptoms continue to get worse or chest pain is unrelieved with rest, call 911 and get to the hospital Complications: - Pericardial effusion: fluid builds and builds in chest putting too much pressure on the heart → requires pericardiocentesis to drain fluid - S/S: hypotensive, poor cardiac output - May need repeat pericardiocentesis as it can come back - Fluid is sent to lab to be cultured to ensure it’s not infectious - Can lead to cardiac tamponade - Cardiac tamponade: worsening of the effusion, too much pressure on the heart - S/S: Beck’s triad - hypotensive, muffled heart sounds, jugular vein distention (JVD) - Requires emergency bedside pericardiocentesis - If pericardiocentesis doesn’t work, they go to OR for pericardial window surgery VASCULAR DISORDERS Hypertensive Crisis: - - Hypertensive urgency: - Diastolic BP > or = 120 mmHg - No obvious organ damage Hypertensive emergency: MOST SERIOUS - Organ damage to VITAL organs - brain, kidneys, heart, lungs - Symptoms will appear depending on where organ damage is - Kidneys → renal failure - Lungs → acute respiratory failure - Brain → brain damage - Need to immediately lower their BP in order to prevent total organ damage - Check albumin levels - Precipitating factors may include noncompliance with meds - If it is not treated, they will die Aortic Artery Disease (aneurysms): - Permanent localized dilation of an artery that forms when the layers/walls are weakened. This is due to plaque build up (high cholesterol), which leads to the aorta getting wider/bulging and weaker Abdominal Aortic Aneurysms (AAA): - More common in men and Caucasians - Below diaphragm Thoracic Aortic Aneurysms (TAA): - More common in men (age 40-70) - Most common site for a dissecting aneurysm (tear in aorta) → HIGH MORTALITY RATE - want to catch before - Above diaphragm *Both AAA and TAA carry high mortality rates Risk factors: - Genetics → Marfan’s syndrome is the hereditary disease most closely linked - Increases with age - Smoking → important because this a change a patient can control - Atherosclerosis - Treated & untreated HTN - CAD - High cholesterol - Blunt trauma (MVA) Symptoms: Thoracic Aortic Aneurysms (TAA): - Constant, severe back/chest pain - Heart failure - Dyspnea - Cough/coarseness in voice - Dysphasia Abdominal Aortic Aneurysms (AAA): - Constant, throbbing pain in abdomen - Back pain - Cyanosis - Pulsating mass in abdomen → DO NOT PALPATE - RISK FOR RUPTURE Diagnostics: - CT scan with IV contrast ASAP → GOLD STANDARD. Will show exact location of aneurysm and its size - Abdominal ultrasound or TTE (issue with ultrasound is that they have to press on abdomen) - EKG (to rule out MI because of chest pain) - Cardiac CT Treatment/INT: - HTN leads to rupture → need to constantly manage BP w/meds - Keep them CALM → do not want to increase sympathetic response - Meds - If the aneurysm is small (< 5 cm), they will manage it outpatient from home (antiHTN meds, q 6 month CT scans) If the aneurysm is bad, they may need IV antiHTN meds Surgical management: - Resection & repair - patch the wall with a mesh graft/lining - RISK FACTORS: infection, mesh issues (tearing, body rejecting it), puncturing of aorta (hemorrhage, death) - Can also have an MI as a result of surgery or go into renal failure Meds: - antiHTN → probably beta blockers - Statins → lower cholesterol - Tetracyclines & macrolides → abx to inhibit AAA progression - Stool softeners (prevent strain) Assessments: - #1 → VITALS (HTN = increased risk of rupture) - Peripheral pulses, skin color, temperature - lack of flow may indicate dissection - Abdominal - very gentle abdominal assessment (not anywhere near mass). Will hear bruit with mass Nursing Diagnosis: - Risk for aspiration - Risk for bleeding - Fear - Risk for ineffective peripheral tissue perfusion - Acute pain Teaching: Managing from home: - Monitoring BP - Low-sodium diet - Med compliance - No bearing down (stool softeners, laxatives) - Regular follow-up (routine CT & ultrasound to assess growth) - Knowing risks for surgery (given by surgeon) - Maintain healthy weight/healthy lifestyle (regular exercise) - Avoid crossing/elevating legs to decrease pressure on aorta - Smoking cessation if possible - S/S of aortic dissection Complication: aortic dissection Aortic Dissection: sudden tear in aorta that creates a false lumen which could allow blood into the aortic wall. Can lead to rupture of aortic aneurysm → LIFE-THREATENING - Primary cause: degeneration of aortic media. HTN is also relevant - Most common sites: ascending and descending thoracic - Symptoms: - Sudden onset of severe and persistent pain - Feels like someone is tearing/ripping apart inside of your chest or back and extending to the shoulders, epigastric area, or abdomen - - Anything distal to dissection will lose blood flow Diaphoresis, nausea, vomiting, faintness, and tachycardia BP is differing from one arm to the other → frequent, MANUAL BP - Do not delegate BP! Want good, accurate measurements Symptoms of ruptured aortic aneurysm: - Similar to dissection - Pain and then loss of consciousness due to hypovolemic shock from massive blood loss - Can die if not treated quickly enough -- a lot of patient’s don’t make it to hospital in time CARDIOVASCULAR DYSFUNCTION Cardiac Output: total amount of blood pumped per minute - Dependent upon the HR and stroke volume Normally, we pump about 4-8 liters/minute Stroke Volume: amount of blood pumped out of the left ventricle with each heartbeat - Dependent on 3 factors: preload, afterload, and contractility Preload: the end diastolic pressure or volume that stretches the right or left ventricle. It reflects fluid volume status (pressure in the heart before it pumps) - Can be affected by… - Body position (different lying down vs. sitting up) - Meds - Amount of overall blood volume Afterload: the force or resistance the ventricles must overcome to eject blood into the aorta or pulmonary circuit (the resistance it must overcome to circulate blood) Contractility: force/strength of contraction of heart muscle - There are meds that affect this (dobutamine, epinephrine) Hemodynamic Monitoring Systems: provides direct measurement of pressures in the heart and great vessels (invasive) - Central venous pressure (CVP) - Arterial (A-line) Central Venous Pressure (CVP): measuring pressure from blood returning to right atrium from SVC - Transducer is secured at the phlebostatic axis, which is the external reference point that ensures accurate readings - Pt lays in supine position in order to get to right atrium - Pressure bag holds saline flush bag to prevent backup of blood - At risk for infection, hemorrhage - If this doesn’t work → A-line for accurate BP Arterial line: inserted into radial artery to ensure accurate BP - MAP of 65 mmHg is necessary for end-organ perfusion Can also draw blood from it so we’re not sticking them again Prior to insertion → Allen’s test to confirm good blood flow in the ulnar artery in case the radial artery is damaged as a result of cannulation (color should return in 7-10 seconds) Complications: bleeding, infection, dislodged line leading to further complications Central Venous Monitoring: can measure preload & CVP - Sits in either right atrium or right above it → HUGE INFECTION RISK Has multiple ports → can give multiple drugs/fluid at one time or TPN Complications: infection, dislodgment Myocardial Infarction (MI): destruction of heart muscle from lack of oxygenated blood supply - Atherosclerosis that ruptures and forms a thrombus in the coronary artery (and occlusion of blood flow to the heart) No blood flow → ischemia to the heart muscle which will eventually cause it to die and will not be able to regenerate → decreased CO Stable angina: episodes of intermittent chest pain with exercise but is relieved by rest - Warning sign of potential heart muscle damage - Can take nitro, but typically don’t - Nitro: take it first then call 911 Acute Coronary Syndrome: kind of like unstable angina - NSTEMI: a partial occlusion of a major coronary vessel or a complete occlusion of a minor coronary vessel causing reversible partial thickness heart muscle damage - STEMI: a complete occlusion of a major coronary vessel resulting in irreversible full thickness heart muscle damage *Will see elevated troponin - Occlusion of the right coronary artery → HF symptoms - Left Anterior Descending (LAD) coronary artery: occlusion of this = “widow maker” - TO DO: look at 12 lead EKG to see where the MI is occurring Risk factors: - Males > females - Female - postmenopausal - Smoking - Diabetes - HTN - High cholesterol - Afib - Stress - Trauma - CAD - Obesity - Family history *Identify modifiable risk factors Symptoms: - Stable angina (predictable) - Unstable angina (sudden) - MEN: - Jaw pain - Left arm pain radiating from upper shoulder - WOMEN: - Back pain - GI - Anxiety - Diaphoretic - Fatigue - ELDERLY: - Change in mental status *Depending on which vessel is affected, you may see other symptoms such as hypotension, bradycardia, JVD, HTN, CHF, tachypnea Labs & Diagnostics: - LABS: troponin, CK, CKMP, BMP, BNP (CK is released from the brain, skeletal tissue, and cardiac tissue; CKMP is specific to the cardiac muscle) - CKMP is increased at 3 hours and remains elevated for up to 36 hours and then starts to return to normal - Troponin elevates within 4 hours and stays elevated for 10 days - DX: echo, vitals Treatment: - Coronary angiography → GOLD STANDARD (thread catheter up through right radial and inject dye to see what the heart looks like to see where the occlusion is. Once they find it, they can put a stent in and open it up) - Oxygen - Meds - Reperfusion therapy - Coronary Artery Bypass Graft (CABG) - surgical Meds: - Nitroglycerin → preferred drug. Can give up to 3 times - TAKE BP Q 5 MIN! CANNOT GIVE UNLESS YOU HAVE BP (BP → NITRO) - Aspirin - Morphine → vasodilates - DON’T give right away - - Beta Blocker → given sometimes to bring HR down bc you don’t want heart working too hard. Metoprolol has antidysrhythmic and antiHTN properties but slow the HR - HOLD med & notify HCP if apical pulse <60/min Heparin → given before cath lab to prevent anything from occurring Coronary Artery Bypass Graft (CABG): surgical revascularization that bypasses blockages in the coronary arteries that are causing heart muscle damage - Done when there are multiple vessels (3+) that have blockages - If a patient is not a candidate for a PCI, sometimes they will go straight to OR for this - They take a healthy vein or artery, typically the internal thoracic artery (mammary) or saphenous vein, and it is grafted to the blocked coronary artery so blood can bypass the blockage - COMPLICATIONS: - Dysrhythmias (specifically Afib) - may need meds to maintain - Bleeding - MI - Stroke - Nonunion of sternum - Sternal infection - Renal failure (because of bypass machine used during surgery) - Heart failure - long-term, not curable - Systemic inflammatory response Nursing Management: - Nursing Diagnosis: - Decreased cardiac output - Assessments: - Pain - Vitals - Peripheral pulses AFTER CABG: - Monitor urine output - They will be on a hemodynamic monitoring system (R-line) - Chest tubes for drainage - Hourly I&O - Skin color, temp - Interventions: - Oxygen - IV fluids - Meds - If femoral approach for PCI → bedrest - Monitor both sites for bleeding - Heart-healthy diet - Up and walk ASAP following surgery - may be just side of bed, chair, etc. but want them up - Monitor for infection in their incision - Teaching: - Med compliance Worsening symptoms (MI) Diet PT No lifting > 10 lbs Do not raise arms above head No bending at waist No vigorous activity until cleared by your physician Cardiac rehab (like PT but for your heart) Cardiogenic Shock: occurs when the heart muscle is unable to pump adequate CO to meet the body’s needs to maintain adequate tissue perfusion. Leads to decreased cardiac output (decreased ejection fraction) - Causes: - Most common cause → MI Compensatory mechanisms kick in to try and help but eventually they’re going to stop working because they need help and if they’re not fixed, you will die. Leads to increased HR - - - Symptoms: similar to MI - SOB/chest pain - Crackles upon auscultation - Decreased peripheral pulses - Cool, pale skin/diaphoresis - Bowel sounds/N/V - Decreased urine output - Restlessness - Confusion - Increased HR - Increased lactic acid build up - ABG’s - metabolic acidosis - Inadequate organ perfusion → eventually lead to multiple organ systems fail Labs & Diagnostics: - LABS: CBC, BMP (assess organ function), cardiac enzymes, lactic level (assess tissue perfusion), ABG analysis (metabolic acidosis) Treatment: - PRIORITY → Oxygen - 100% via non rebreather mask (want to decrease the work of breathing and improve oxygenation) - Meds - PCI - Intra-aortic balloon pump → used when initial medical management doesn’t improve cardiac output; goal is to increase oxygen supply and decrease the myocardial oxygen demand - Mechanical Circulatory Support (MCS) Devices: - Mechanical pumps to help decrease the workload on the heart - - LVAD: in left ventricle. Used in HF or cardiogenic shock as a bridge to recovery or to transplantation while they’re waiting. Medically controlled on meds while they’re waiting Extracorporeal membrane oxygenator (ECMO) → used at the bedside for those with severe acute respiratory and/or cardiac failure who have a high mortality risk Heart transplant → eventually this may be the only option Meds: WANT TO INCREASE BP & CARDIAC OUTPUT AND DECREASE CARDIAC WORKLOAD - Inotropics → dobutamine and epinephrine (improve CO) - Vasopressors → dopamine, norepinephrine (Levophed), or phenylephrine (support BP & maintain adequate MAP) - likely will have an A-line - Nitroglycerin → decreases preload through venous dilation & afterload through arterial dilation (*NOTE: it will decrease BP - use with caution) - Nitroprusside → decrease afterload - also decreases BP - CAUTION - Diuretics → decrease filling volumes by increasing urine output - Morphine sulfate → may relieve pain due to an MI and decrease venous return & preload through its action as a venous dilator Nursing Management: - Nursing Diagnosis: - Decreased cardiac output - Assessments: - Hemodynamic monitoring - BP on each arm - Interventions: - 100% oxygen non-rebreather mask - Diet low in sodium - LVAD - can get up for small periods but with frequent rest periods in between - Teaching: - S/S of heart failure - When to call 911/when to notify physician