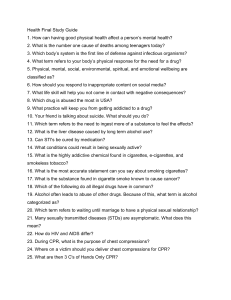
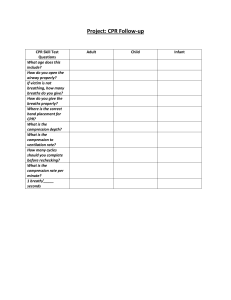
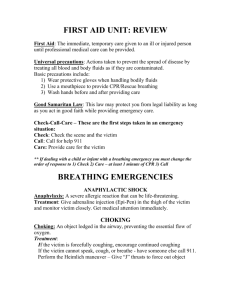
CARDIAC ARREST Sudden cardiac arrest is different from a heart attack, which occurs when blood flow to a portion of the heart is blocked. However, a heart attack can sometimes trigger an electrical disturbance that leads to sudden cardiac arrest. Sudden cardiac arrest is a medical emergency. If not treated immediately, it causes sudden cardiac death. With fast, appropriate medical care, survival is possible. Administering cardiopulmonary resuscitation (CPR) — or even just rapid compressions to the chest — can improve the chances of survival until emergency personnel arrive. Definition Sudden cardiac arrest is the sudden, unexpected loss of heart function, breathing and consciousness. Sudden cardiac arrest usually results from an electrical disturbance in heart that disrupts its pumping action, stopping blood flow to the rest of the body. A cardiac arrest, also known as cardiopulmonary arrest or circulatory arrest, is the abrupt cessation of normal circulation of the blood due to failure of the heart to contract effectively during systole. Causes Hs Hypovolemia caused by bleeding, anaphylaxis, or pregnancy Hypoxia - A lack of oxygen delivery to the heart, brain and other vital organs. Hydrogen ions (Acidosis) - An abnormal pH in the body as a result of lactic acidosis which occurs in prolonged hypoxia and in severe infection Hyperkalemia or Hypokalemia - Both excess and inadequate potassium can be life-threatening. Hypothermia - A low core body temperature, defined clinically as a temperature of less than 35 degrees Celsius (95 degrees Fahrenheit). Hypoglycemia or Hyperglycemia - Low blood glucose from overdose of oral hypoglycemics such as sulfonylureas, or overdose of insulin. Ts Tablets or Toxins Tricyclic antidepressants, phenothiazines, beta blockers, calcium channel blockers, cocaine, digoxin, aspirin, acetominophen. Cardiac Tamponade - Blood or other fluids building up in the pericardium can put pressure on the heart so that it is not able to beat. Tension pneumothorax - The build-up of air into one of the pleural cavities, which causes a mediastinal shift. When this happens, the great vessels (particularly the superior vena cava) become kinked, which limits blood return to the heart. Thrombosis (Myocardial infarction) Thromboembolism (Pulmonary embolism) hemodynamically significant pulmonary emboli are generally massive and typically fatal. Causes Respiratory Cardiac Respiratory failure CAD Neurovascular Myocardial infarction disease Congestive heart failure, Pulmonary embolism, etc etc Drug Mechanical Poisonous drug Obstruction Anti depressant Drowning Relaxant Accident Cardiac drug Burn Drug toxicity Gas and smoke Metabolic and inhalation electrolyte Hypo/Hyper electrolyte Metabolic acidosis Hypo/Hyper glycaemia Risk factors: Scarring from a prior heart attack or other causes Cardiomyopathy Cardiac medications Electrical abnormalities Blood vessel abnormalities Recreational drug use Symptoms Signs of cardiac arrest: It strikes suddenly and without warning. Sudden loss of responsiveness No response to tapping on shoulders Does nothing when you ask if he is okay No normal breathing The victim does not take a normal breath when you tilt the head up Check for at least five seconds Signs and symptoms of Cardiac arrest Late Early -Unresponsiveness Dilation of pupil -Apnoea/gasping Cold and clammy skin -No carotid pulse Cyanosis If these signs of cardiac arrest are present: Call for emergency medical services Get an automated external defibrillator (AED) If one is available Begin CPR immediately Continue until professional emergency medical services arrive Use the AED as soon as it arrives. If two people are available to help, one should begin CPR immediately while the other calls 9-1-1 and finds an AED. Cardiopulmonary resuscitation: Cardiopulmonary resuscitation (CPR) is a procedure to support and maintain breathing and circulation for a person who has stopped breathing (respiratory arrest) and/or whose heart has stopped. It is a method which includes all measures that are applied to revive patients who have stoped breathing suddenly or unexpectedly either due to respiratory or cardiac failure Cardiopulmonary resuscitation (CPR) is an emergency procedure which is performed in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person in cardiac arrest. CPR involves chest compressions at least 5 cm deep and at a rate of at least 100 per minute in an effort to create artificial circulation by manually pumping blood through the heart. Epidemiology: The American Heart Association reports that, in the United states, nearly 250,000 deaths each year are due to heart attacks. Out of these 80% die outside the hospital setting and do not received any medical treatment after suffering heart attack. If CPR is administered within first four minutes after the heart attack, the chances for brain damage are virtually nonexistent. If administered between 4 to 6 minutes the brain damage is probable, 6 to 10 min brain damage is likely, and after 10 min the chances of some type of brain damage are virtually certain. So knowledge of CPR does not only save lives, but also allows victims to recover without sustaining any permanent damage. Purpose: -CPR is performed to restore and maintain breathing and circulation and to provide oxygen and blood flow to the heart, brain, and other vital organs Indication of CPR: There are three general symptoms that warrant immediate administration of CPR: Victim is not Breathing Victim has No Pulse Victim is unconscious. 1. Cardiac arrest: Ventricular Fibrillation(VF) Ventricular tachycardia(VT) Asystole Pulse less electrical activity 2. Respiratory Arrest Drowning Stroke Foreign body in throat Smoke inhalation Drug overdose Epiglottis paralysis Suffocation Accident injury Coma Principles of CPR: To restore effective circulation and ventilation To prevent irreversible cerebral damage due to anoxia. When the heart fails to maintain the cerebral circulation for approximately four minutes the brain may suffer irreversible damage. General Instructions For effective CPR: 1. CPR technique is used in persons whose respiration and circulation of blood have suddenly and unexpectedly stopped. 2. There is no need of attempting CPR techniques in patients in the last of an incurable illness and in persons whose heart beat and respirations have been absent for more than six minutes. 3. The immediate responsibilities of the resuscitator are: o To recognize the signs of cardiac arrest o Protect the patient’s brain from anoxia by immediately starting o Artificial ventilation of the lungs and external cardiac massage. o Call for help 4. The cardio-pulmonary resuscitation must be initiated within three or four minutes in order to prevent permanent brain damage. o Strike the center of the chest sharply with of the clenched first twice. o Call for assistance o Clear the airway of false teech, vomitus, food material etc. o Initiate ventilation and external cardiac massage without wasting time. 5. The CPR techniques should not be discontinued for more than five seconds before normal circulation and ventilation of lungs are established except; o When the patient’s is moved to a hard surface o When endotracheal intubation is being carried out( maximum time allowed for these two procedures is 15 second o Before CPR is attempted in a patient, make sure that the airway is clear. It may be obstructed due to many reasons. So keep the patient’s neck hyper extended after confirming that he is having any cervical injury. Sequence of CPR: CPR consists of three phases; Phase I Phase II Phase III Phase I- Basic life support: I. A-Airway: The first step on CPR is to establish patent airway for the patient. Completely 30 compression and quickly maintain airway. Give head tilt chin lift position (in case of neck injury use jaw thrust position because it reduces neck and spine movement.) Steps to perform head tilt chin lift position: Place one hand on the victim’s forehead and push with your palm to tilt the head back. Place the finger of the other hand under the bony part of the lower jaw near the chin. Lift the jaw to bring the chin forward. Things to avoid with head tilt thin lift: Do not press deeply into the soft tissue under the chin because this might block the airway. Do not use the thumb to lift the chin. Clear the airway if an obstruction is suspected, clear the mouth and upper airway with finger or by suction. Establish an artificial airway if the patient does not breath spontaneously with the positioning of the head and neck. This is done by passing an endo tracheal tube of appropriate size into the trachea. II. B- Breathing: If the spontaneous breathing does not takes place after establishing a patent airway the rescuer should try to ventilate the lungs. This can be done by mouth to mouth breathing bag and mask ventilation or mechanical ventilation. Ventilate the lungs using mouth to mouth or mouth to nose breathing. Keeps the head and neck in the hyper extended position. Pinch the patient nose after taking a deep breath, open the mouth widely and cover the patient mouth around the lips completely to produce a tight seal. Deliver three or four full breaths into patient mouth in quick succession. Look for chest wall to rise with each breath look, listen and feel for patient exhaled breaths. III. C- Circulation:- When cardiac arrest is suspected, verify it by the absent carotid. Steps to locate carotid artery: 1. Locate the trachea using 2 or 3 fingers. 2. Slide this 2 or 3 fingers into groove between the trachea and the muscle at the side of the neck (sternocleido muscle), where you can feel carotid pulse. 3. Feel for pulse for at least 5 sec but not more than 10 sec. If no pulse start CPR with chest compression at a rate of 100/ mints (follow 30:2 compression and respiration). 4. The foundation of CPR is chest compression. Steps to perorm chest compression: 1. Position yourself at the victim’s site. 2. Make sure the victim is lying face up as a firm, flat surface. If the victim is lying face down, carefully roll him face up. If you suspect the victim has head or neck injury try to keep the head, neck and torso in a line when rolling the victim to a face up position. 3. Draw imagery line between 2 nipples. Put the head of one hand on the centre of the victim’s chest on the lower half of the breast bone in between nipple). 4. Put the head of or other hard or top of the 1st hands. 5. Straighten your arms and position or shoulders directly over your hands. 6. Push hard and fast: press down at least 2 inches (5 cm) with each compression, deliver compression in smooth fashion at a rate of at least 100/ mins. 7. At the end of each compression make sure you allow the chest to recoil (re-expand) completely. Chest recoil allows Blood to flow into the heart and is necessary for chest compression to create blood flow. 8. Minimize interruption. Phase II- Advanced Life Support E. ECG: Connect The Patient To Monitor Watch for any abnormal rhythm F- Fibrillation: If monitor shows ventricular tachycardia or ventricular fibrillation, take a rhythm strip Select 200 joules deliver shock if no change again deliver shock needed. Phase-III Prolonged life support:G-Gauging: Identify the cause and treat Do hemodynamic monitoring ECG, cardiac monitoring, vital signs Temporary pacing Intubation H- Human mentation: Save the cerebral circulation initiate CPR within 4 minutes Monitor pupils reaction and changes Check general responses. I- Intensive care : Transfer to intensive care unit Monitor closely and continuously. The American Heart Association guidelines: The 2010 guidelines "strongly recommend" that untrained / lay responders perform "compression-only" CPR, sometimes known as CCR. However, medical professionals and trained lay people are still urged to give the victim two "rescue breaths" in between each series of 30 chest compressions. Points to be remembered if performing Chest Compressions only: 1. Chest compressions should be performed at 100 per minute 2. Increase the depth of chest compressions to at least 2 inches for adults; children and infants 1.5 inches 3. Continue with chest compressions for as long as possible or until help arrives 4. There has been a change in the recommended sequence for the lone rescuer to initiate chest compressions before giving rescue breaths (C-A-B rather than A-B-C). Before proceeding with CPR: Make sure rescuer is not in any danger Make sure that victim is not in danger -Avoid moving the victim unless there is in immediate danger or preparing for CPR Assess the surroundings for any people who can help Determine if the victim is conscious or unconscious by positioning yourself next to the victim, tapping him/her on the shoulder and shouting "Are you OK? Are you OK"" several times If no response, immediately ask someone to call 911 and then have the person report back to you. If no one is available call 911 yourself prior to beginning CPR Basics of CPR: To perform CPR, remember the basic steps of CPR administration called CAB o C for circulation o A for airway o B for breathing C – COMPRESSIONS: External chest compressions provide artificial circulation when rescuer apply rhythmic pressure on the lower half of the victim's breastbone, it force the heart to pump blood. A - CLEAR AIRWAY Place the victim on his/her back on a firm surface. Kneel next to the victim's neck and shoulders. To open the airway, place palm on the forehead to carefully tilt the head back and lift the chin forward with other hand. Then check for signs of life for no longer than 10 second. Place ear over the mouth of the victim, and while counting from 10 to 0 listen if the victim is breathing. There are no signs of life, proceed to B. B – BREATHING : Breathing - refers to rescue breathing, where one person is breathing into other or also commonly referred to as mouth to mouth technique Using the thumb and forefinger of rescuer hand that's on the victim's forehead, pinch the person's nose shut. Keep the heel of rescuer hand in place so the person's head remains tilted. Keep rescuer other hand under the person's chin, lifting it up. As rescuer keep an airtight seal with his mouth, give first breath and watch the victim's chest rise. If rises, give second breath. If not, start from the beginning. Goal is for the victim to receive two full mouth to mouth breaths, 1 second each. CPR Guidelines for the health care provider: A. Chest compressions: Push hard and push fast Compress chest at rate of 100/mt Allow complete chest recoil after each compressions Minimize interruptions in chest compressions B. Compression-to-ventilation ratio: 30:2 for single rescuer for all clients except newborns C.1-second breath: Each rescue breath should be given over 1 second Chest should rise with each breath Avoid delivering too many breaths or breath too large and/ too forceful D. Attemp defibrillation: Deliver one shock followed by immediate CPR beginning with chest compressions Check rhythm after 5 cycles of CPR Basic Life Support: Basic life support is an emergency procedure that consists of recognizing an arrest and initiating proper CPR techniques to maintain life until the victim either or its transported to a medical facility where advanced life support measures are available. CHECK RESPOSIVENESS Shake and Shout OPEN AIRWAY Head tilt-chin lift/jaw thrust CHECK BREATHING Look, listen and feel IF BREATHING Put in recovery position IF NO BREATHING Provide 2 effective breaths and assess for Signs of circulation 10seconds only NO CIRCULATION Compress chest 100/minute in ratio of 30 compression to 2 breaths CIRCULATION PRESENT Continue rescue breathing Check circulation every minute Steps of CPR: Safe implementation of CPR involves the five steps STEP I: Assess level of consciousness: Person who appears to be unconscious may be asleep, deaf, or possibly intoxicated. Unconsciousness is confirmed by shaking the victim’s shoulder and shouting “ Are you Ok? If the person does not responding, the emergency response system is activated Immediately and the victim is cautiously placed in the supine position on a firm surface, remembering the potential for head injury. STEP II: Open the Airway: The tongue is a common cause of airway obstruction in the unconscious person. The head tilt chin lift method and the jaw thrust are the two recommended methods for opening and maintaining the airway. Jaw thrust ( without head tilt) is the safest approach to use with a victim with a suspected neck injury. The head must be carefully supported to avoid turning or tilting it backward. While maintaining an open airway, the rescuer takes 3 to 5 seconds to look, listen and feel for spontaneous breathing. STEP III: Initiate Artificial Ventilation Give mouth to mouth breathing: 1. Hold the victim’s airway open with the head tilt chin lift. 2. Pinch the nose close with your thumb and index finger (using the hand on the forehead). 3. Take a regular (not deep) breath and seal your lip around the victim’s mouth creating an air tight seal. 4. Give one breath (blow for about 1 sec). 5. Watch for the chest to rise as you give the breath. 6. Give a second breathe blow for about 1 sec. Watch for the chest to rise. 7. If you are unable to ventilate the victim after two attempts, promptly return to chest compression. OR Give mouth to mask breathing: 1. Position yourself at the victim side. 2. Place the mask in the victim face using the bridge of the nose as a guide for correct position. 3. Seal the mask against the face : Using the hand that is closer to the top of the victim’s head, place your index finger and thumb along the edge of the mask. Place the thumb of your second hand along the bottom edge of the mask. 4. Place the remaining finger of your second hand along the bony margin of the jaw and lift the jaw. Perform a head tilt chin lift to open the airway. 5. While you lift the jaw, press firmly and completely around the outside edge of the mask to seal the mask against the face. 6. Deliver air over 1 sec to make the victim’s chest rise. Steps to perform bag mask ventilation: Positive pressure ventilation during CPR with bag mask device:1. Position your self directly at the head side off the victim. 2. Place the mask on the victim face using the –bridge of the nose as guide for correct position. 3. Use the ec clamp technique to hold the mask in place while you lift the jaw to hold the airway open: Perform a head tilt. Place the mask on the face with narrow portion at the bridge of the nose. Use the thumb and index finger of one hand to make a “C” on the side of the mask. Use the remaining finger to lift the angle of the jaw (3fingers from an “E”). Open the airway and press the face to the mask. 4. Squeeze the bag to give breath (1 sec each). STEP IV: Check for signs of circulation After you have given the first two breaths, check the victim’s for signs of circulation to see if the heart is beating .If the victim has no signs of circulation, CPR must be started immediately. If the victim’s has signs of circulation but is not breathing, continue rescue breathing at arate of one breath every five seconds, or 12 per minute. Post resuscitation measures: After care of patient who has suffered cardiac arrest is crucial to survival. Typical orders and their rationale are as follows: If not already in the ICU or CCU the patient is admitted there because of the need for constant observation, monitoring equipment, defibrillation and so forth. Monitoring of ECG, CVP, and blood pressure is instituted. Temperature is taken every hours for high temperature. High temperature usually indicates cerebral damage or edema. A hypothermia blanket is used if temperature is over 1010f or 38.50f. Hypothermia helps to lessen cerebral edema e)Blood gas and pH determination are done to detect metabolic acidosis which may have developed owing to poor oxygenation during arrest A chest x-ray film to be obtained using portable equipment, ribs often are accidently fractured during cardiac massage Insert endotracheal tube if not already in place. This maintain as open airway for the unconscious patient who do not clear secretion by coughing Give oxygen continuously for 48hours following resuscitation by endotracheal tube or mask Insert foley’s catheter to measure urine output. Complication of CPR: Trauma ,fractured ribs and sternum Pneumothorax Rupted spleen Skin burns Cervical neck injury Oral, tracheal and larygea; damage Congestive heart failure Anoxic encephalopathy .Surgical management: ͽ Coronary angioplasty ͽ Coronary bypass surgery ͽ Corrective heart surgery ͽ Heart transplantation ͽ Radiofrequency catheter ablation Medications used in CPR Agent and Indications Action Oxygen— Administered to improves tissue all patients with oxygenation and acute cardiac corrects ischemia or hypoxemia suspected hypoxemia, including those with COPD Epinephrine— Given to patients increases in cardiac arrest, systemic especially caused vascular by a systole or resistance and pulse less BP; improves electrical activity; coronary and may be caused by cerebral ventricular perfusion and tachycardia or myocardial ventricular contractility fibrillation Vasopressin (Pitressin) increases systemic vascular resistance and BP An alternative to epinephrine Nursing consideration Use 100% FiO2 during resuscitation. Recognize that lung damage is unlikely when used for short time. Monitor dose by pulse oximeter. Administer 1 mg every 3–5 minutes by IV push or through endotracheal tube. Avoid adding to IV lines that contain alkaline solution (bicarbonate). Give 40 U IV one time only Atropine— blocks parasympathetic action; increases SA node automaticity and AV conduction Given to patients Give rapidly as 0.5 mg with symptomatic IV push; may repeat the bradycardia dose of 3 mg (hemodynamicall Be aware that less than y unstable, 0.5 mg in adult can frequent cause heart rate to premature decrease to a worse ventricular bradycardia. contractions, and Monitor patient for symptoms of reflexive tachycardia ischemia) Sodium bicarbonate (NaHCO3)— corrects metabolic acidosis Given to correct metabolic acidosis Administer initial dose of 1 mEq/kg IV; then administer dose based on base deficit calculated from arterial blood gas values. Recognize that to prevent development of rebound metabolic alkalosis, complete correction of acidosis is not indicated. Magnesium— Given to patients May give 1–2 g diluted promotes with abnormal in 10 mL D5W over 5– adequate rhythm 20 minutes. functioning of Monitor for hypotension, cellular sodium– asystole, bradycardia, potassium pump and respiratory paralysis Follow-up interventions: Diagnostic tests are often made during and after resuscitation to determine precipitating causes, evaluate the effectiveness of resuscitation, and detect complications. Test commonly performed are; 1. Chest radiograph 2. ECG available, apply it and follow the prompts. 3. Hemodynamic monitoring 4. Laboratory studies including arterial blood gas analysis Nursing Consideration of CPR: Clients who survive cardiopulmonary arrest are admitted to a critical care unit, where they receive continuous cardiac monitoring and have vital signs taken every 15 minutes until stable. Nurse who works in the critical care setting should assess for any type of ECG changes in the monitor, if noted should inform immediately and emergency interventions should be done. Post-resuscitation assessment provides important information regarding the effectiveness of the resuscitation. Common disorders include recurrent dysrhythmias, coma, other neurologic disorders, and renal failure. After the client regains consciousness, profound anxiety often appears. The nurse should remember that clients need psychological support when they have undergone such as catastrophic physiologic event. Many clients have a very clear recall if the events surrounding the resuscitation, including the verbal communication that occurred. For this reason, members of the resuscitation team should careful about what they say The nurse should take time to assess the client’s coping mechanisms. The nurse should encourage expression of such feelings and concerns, not only by the client but by significant others who are equally stressed by the sudden, serious nature of the disorder. Clear explanations and clarifications of misconceptions about what has happenedhelp move client forward to optimal physiologic and psychological recovery. Prognosis o If done well, CPR saves life o Normaly is restored in rescued person o CPR can also be ineffective, causing death o In some cases, causes injuries