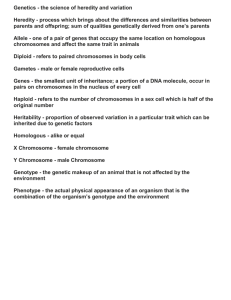
lOMoARcPSD|10466586 Fetal Development and Genetics CH10 Concepts Of Maternal-Child Nursing And Families (Nova Southeastern University) StuDocu is not sponsored or endorsed by any college or university Downloaded by Jill Sapp (peachprincess712@gmail.com) lOMoARcPSD|10466586 Fetal Development and Genetics CH 10 Stages of Fetal Development Preembryonic Stage “Conception” o Begins with fertilization which typically occurs around 2 weeks after the last normal menstrual period in a 28 day cycle Fertilization takes place in the outer third of the ampulla of the fallopian tube o Mitosis (cleavage) occurs as the zygote is slowly transported into the uterine cavity o After four cleavages, appears as a solid ball of cells called Morula o Blastocyst forms as fluid from the uterine cavity enters the morula Inner surface of blastocyst forms the embryo an amnion Trophoblast is the outer layer of cells surrounding the blastocyst Develops into the chorion and helps form the placenta Trophoblast attaches itself to the surface of the endometrium for further nourishment o Normally, implantation occurs in the upper uterus (fundus), where a rich blood supply is available o Process of attachment and placental formation is termed implantation o From a medical prospective, a pregnancy has not occurred until successful implantation has taken place o Three embryonic layers of cells formed: Ectoderm: forms the CNS, Special senses, Skin, and Glands Mesoderm: forms the Skeletal, Urinary, Circulatory, and Reproductive organs Endoderm: forms the Respiratory system, Liver, Pancreas, and Digestive system o Many women are unaware that pregnancy has begun at this point and several weeks will pass until signs of pregnancy start Embryonic Stage o Begins at day 15 after conception and continues through week 8 o Basic structures of all major body organs and the main external features are completed during this time period o Critical period of differentiation o Growing embryo is most susceptible to damage in this stage from external sources including Teratogens (substances that cause birth defects like alcohol/drugs), Infections (rubella or cytomegalovirus), Radiation, and Nutritional deficiencies. o Amnion is thin protective membrane that contains amniotic fluid o As the embryo grows, the amnion expands until it touches the chorion These two fetal membranes form the fluid-filled amniotic sac that protect the embryo o Amniotic sac increases in volume as the pregnancy progresses Amniotic fluid is derived from two sources: Fluid transported from the maternal blood across the amnion Fetal urine Roles of Amniotic Fluid: Helps maintain a constant body temperature for the fetus Permit symmetric growth and development Cushion the fetus from trauma Allow the umbilical cord to be free from compression Promote fetal movement to enhance musculoskeletal development Downloaded by Jill Sapp (peachprincess712@gmail.com) lOMoARcPSD|10466586 Adequate fluid volume is necessary for proper fetal growth and development Normal volume is 1 Liter at term Too little amniotic fluid (Oligohydramnios) o <500 mL at term Too much amniotic fluid (Polyhdramnios) o >2000 mL at term o While the placenta is developing (end of the 2nd week), the umbilical cord is also formed from the amnion o Average umbilical cord is 22 inches long and about 1 inch wide at term o Functions of the Placenta: Serves as the interface between the mother and the developing fetus Acts as a pass-through between mother and fetus, not a barrier Protects fetus from immune attack by the mother Removes waste products from the fetus Induces the mother to bring more food to the placenta Near time of childbirth, it produces hormones that ready fetal organs for life outside the uterus o Hormones Produced by the Placenta: Human Chorionic Gonadotropin (hCG) Basis for pregnancy tests Preserves the corpus luteum and its progesterone production so that the endometrial lining of the uterus is maintained Human Placental Lactogen (hPL) Modulates fetal and maternal metabolism Participates in the development of maternal breasts for lactation Decreases maternal insulin sensitivity to increase its availability for fetal nutrition Estrogen (estriol) Enlargement of a woman’s breasts, uterus, and external genitalia Stimulates myometrial contractility Relaxin Acts synergistically with progesterone to maintain pregnancy Relaxation of the pelvic ligaments Softens the cervix in preparation for birth o As early as 3 days after conception, the trophoblasts make hCG that ensures that the endometrium will be receptive to the implanting embryo o Placenta function depends on the maternal blood pressure supplying circulation Fetal Stage o From the end of the 8th week until birth o Average pregnancy lasts 280 days from the 1st day of the last menstrual period o Longest period of prenatal development o The conceptus is mature enough to be called a fetus o Dramatic growth and refinement of all organ systems take place in this stage Downloaded by Jill Sapp (peachprincess712@gmail.com) lOMoARcPSD|10466586 Fetal Circulation Differs from adult circulation due to the presence of certain vessels and shunts Function of the shunts are to direct oxygen-rich venous blood to the systemic circulation and to ensure that oxygen-depleted venous blood bypasses the underdeveloped pulmonary circulation Prior to birth, the lungs function is taken over by the placenta during fetal life o Lungs finish developing after birth Fetal circulation involves the circulation of blood from the placenta to and through the fetus, and back to the placenta o Oxygenated blood is carried from the placenta to the fetus via the umbilical vein The fetal liver does not perform the metabolic functions that it will after birth because the mother’s body performs these functions Three shunts present during fetal life: o Ductus venosus: Connects the umbilical vein to the inferior vena cava o Ductus arteriosus: Connects the main pulmonary artery to the aorta o Foramen ovale: Anatomic opening between the right and left atrium At birth the foramen ovale, ductus arteriosus, ductus venosus, and umbilical vessels are no longer needed Genetics Genome: the entire hereditary information encoded in the DNA Each chromosome is made up of genes Genes: individual units of heredity of all traits and are organized into long segments of DNA Any change in gene structure or location leads to a mutation, which may alter the type and amount of protein produced Genotype: specific genetic makeup of an individual, usually in the form of DNA, is the internally coded inheritable information Allele: one of two or more alternative versions of gene at a given position or locus on a chromosome that imparts the same characteristic of that gene o One allele comes from the mother and one from the father o May be homozygous or heterozygous Phenotype: the observed, outward characteristics of an individual Homozygous (WW) is dominant Heterozygous (ww) is recessive o Can be Ww if the two alleles differ Humans typically have 46 chromosomes o 22 pairs of non-sex chromosomes (autosomes) and 1 pair of sex chromosomes o XX – Female and XY – Male Karyotype: Pictorial analysis of the number, form, and size of an individual’s chromosomes o Commonly uses WBCs and fetal cells in amniotic fluid o Chromosomes are numbered from the largest to the smallest, 1-22 Some mutations have no significant effect, whereas other can have a tremendous impact on health Patterns of Inheritance for Genetic Disorders o Demonstrate how genetic abnormalities can be passed on to offspring o Diagnosis of genetic disorder is usually based on clinical signs and symptoms or on laboratory confirmation of an altered gene associated with the disorder o Accurate diagnosis can be aided by the recognition of the pattern of inheritance within a family o Mendelian or Monogenic Laws of Inheritance Downloaded by Jill Sapp (peachprincess712@gmail.com) lOMoARcPSD|10466586 Autosomal Dominant Inherited Disorders A single gene in the heterozygous state is capable of producing the phenotype The abnormal gene overshadows the normal gene and person will show S/S of disorder Generally has one affected parent and the other parent is normal There also may be no history of an affected family member Offspring will have 50% chance of being affected Females and males are equally affected Examples of disorders are Neurofibromatosis, Huntington’s disease, Achondroplasia, and Polycystic kidney disease Autosomal Recessive Inheritance Disorders Two copies of the abnormal gene (mutant) in the homozygous state are necessary to produce the phenotype Two abnormal genes are needed for the individual to show S/S of disorder Both parents must be heterozygous carries of the gene (clinically normal but are carriers) Offspring have a 25% chance of being affected, 25% chance of having two normal genes, and a 50% chance of becoming a carrier Females and males are equally affected Examples of disorders are Cystic fibrosis, Phenylketonuria, Tay-Sachs disease, and Sickle cells disease X-Linked Recessive Inheritance Disorders More affected males than females If a male inherits an X-linked altered gene, he will express the condition because a male only has one X chromosome o Any man who is affected with an X-linked recessive disorder will have carrier daughters Females normally need two abnormal X chromosomes to exhibit the disease o And one normal and one abnormal to be a carrier o A woman carrier will have 25% chance of an affected son, 25% chance of a carrier daughter, 25% chance of an unaffected son, and 25% chance of a noncarrier daughter Examples of disorders are Hemophilia, Color blindiness, and Duchenne muscular dystrophy X-Linked Dominant Inheritance Disorders When a male has an abnormal X chromosome or a female has one abnormal X chromosome All of the daughters and none of the sons of an affected male will inherit the condition Both female and male offspring of an affected woman have a 50% chance of inheriting the condition Many X-linked dominant disorders have lethal results in males Males are more severely affected than females These disorders are rare Downloaded by Jill Sapp (peachprincess712@gmail.com) lOMoARcPSD|10466586 Examples of disorders are Hypophosphatemic (vitamin D-resistant) rickets and Fragile X syndrome Multifactorial Inheritance Disorders Examples are Cleft lip, Cleft palate, Spina bifida, Pyloric Stenosis (more common in males), Clubfoot, Congenital hip dysplasia (more common in females), and Cardiac defects Caused by multiple gene and environmental factors Runs in families but the pattern of inheritance is not as predictable with single-gene disorders o Nontraditional Inheritance Patterns Mitochondrial Inheritance Mutations in the mitochondrial DNA Inherited almost exclusively from the mother Mutations are often seen in one or more organs such has the brain, eye, and skeletal muscle Often associated with energy deficits in cells with high energy requirements, such as nerve and muscle cells These disorders tend to be progressive and the age of onset can vary from infancy to adult hood Examples are Kearns-Sayre syndrome and Leber’s hereditary optic neuropathy Genomic Imprinting Plays a critical role in fetal growth and development and placental functioning Does not alter the genetic sequence but affects the phenotype Disruption of imprinting usually involve a growth phenotype and include varying degrees of developmental problems Examples are Prader-Willi syndrome, Angelman syndrome, and BeckwithWiedemann syndrome Chromosomal Abnormalities o Do not follow straightforward patterns of inheritance o Some can be inherited but most occur due to random events during the formation of reproductive cells or in early fetal development o Abnormalities of Chromosome Number Often result due to nondisjunction (failure of separation of the chromosome pair during cell division) Most result in spontaneous abortion Monosomy: there is only one copy of a particular chromosome instead of the usual pair (an entire single chromosome is missing) In these cases, all fetuses spontaneously abort in early pregnancy Survival is only seen in mosaic forms Trisomy: there are three of a particular chromosome instead of the usual two (an entire single chromosome is added) Most common trisomies include Trisomy 21 (down syndrome), Trisomy 18, and Trisomy 13 o Abnormalities in Chromosome Structure Occur when there is a breakage and loss of a portion of one or more chromosomes, and during the repair process the broken ends are rejoined incorrectly Usually lead to having too much or too little genetic material Portions of chromosomes can be deleted or duplicated o Downloaded by Jill Sapp (peachprincess712@gmail.com) lOMoARcPSD|10466586 Examples are Cri du chat syndrome and Fragile X syndrome (males) Inversions: portion of the chromosome breaks off at two points and is turned upside down and reattached Ring chromosomes: portion of chromosome has broken off in two places and formed a circle Translocation: most clinically significant Portion of one chromosome is transferred to another chromosome and an abnormal rearrangement is present o Sex Chromosome Abnormalities Usually less severe in their clinical effects than autosomal chromosomal abnormalities Gender-specific and involve a missing or extra sex chromosome Affect sexual development and may cause infertility, growth abnormalities, and possibly behavioral and learning problems Examples are Turner syndrome (females) and Klinefelter syndrome (males) Genetic Evaluation and Counseling o Genetic consultation involves evaluation of an individual or a family o Purpose of genetic counseling: Confirm, diagnose, or rule out genetic conditions Identify medical management issues Calculate and communicate genetic risks to a family Discuss ethical and legal issues Assist in providing and arranging psychosocial support o Ideal time for counseling is before conception o Preconception counseling allows couples to identify and reduce potential pregnancy risks, plan for known risks, and establish early prenatal care o Involves extensive information gathering about birth history, past medical history, and current health status as well as a family history of congenital abnormalities, mental retardation, genetic disease, reproductive history, general health, and causes of death o Information is usually on three generation but if the family history is complicated then information is needed from more distant relatives Nursing Roles and Responsibilities Take family history, Schedule genetic testing, Explain the purpose of all screening and diagnostic tests, Answer questions, and Addressing concerns raised by family members Play an important role in beginning the preconception counseling process and referring women and their partners for further genetic testing when indicated Family medical history helps identify those at risk for genetic conditions and help initiate a referral when appropriate Downloaded by Jill Sapp (peachprincess712@gmail.com)