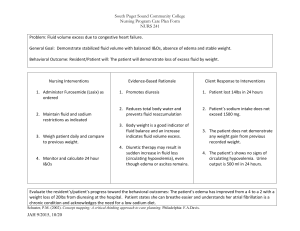
Normal O2 saturation range for adult Vital Sign:vital signs for adults, normal Normal: Abnormal: Blood Pressure 120/80 mmHg Heart Rate 60-100 bpm Tachycardia >100 bpm Bradycardia < 59 bpm Temperature 37 C 98.6 F (can range 97-99) Hypothermia: 95 or less Low grade Fever: 99-100.4 Fever: 100.4-103 High Fever: 103+ Hyperthermia: 104+ Respiratory rate 12-16 breaths per minute SpO2 95%-100% Tachypnea: > 20 bpm Bradypnea: < 12 bpm COPD pts: 88%-92% Hypoxia in adults: 85%-94% What is the nursing process? What is the nursing process? o A series of organized systematic steps for nurses to provide excellent care o Core of nursing What is ADPIE? Try to critically think and apply this to patients with variable medical diagnoses o *Assessment: RN collects data; includes physiology, psychologic, sociocultural, economic, and lifestyle o Includes subjective & objective data o 3 parts of assessment: • Interview of health history (subjective) ** MOST important part of health history** The purpose is to obtain info about client’s health based on their perception o Identifying data ▪ Name, DOB, age, birthplace sex, marital status, race, insurance, source & reliability o Chief Complaint (CC) ▪ Complaint X duration • E.g., back pain x 3 months • It is 1 symptom o History of present illness (HPI) ▪ OLDCART ▪ A more detailed explanation of CC ▪ PQRST for pain ▪ o Past medical History ▪ Allergies, current meds (dose, route, frequency), medical history, surgical history, immunizations o Social history ▪ Occupation, education, finances, ethnicity, spirituality, ADLs, nutrition, sx use, environment o Family history ▪ Must state +/- of CA, CVA, DM, HTN, CAD o Review of body systems (ROS) ▪ An interview, NOT a physical exam ▪ Interview pt about each body system and document if present/absent and describe if present ▪ General, derm/hair/nails, HEENT, respiratory, cardiac, gastrointestinal, reproductive, musculoskeletal, neuro, psyh • Physical assessment (objective) o Hands on examination to include vitals, and surveying the body systems o These data are seen, felt, heard, • Documentation o Diagnose/analyze: nurse’s judgment about the health conditions or needs; formulation of nursing diagnosis which serves as the base for the care plan o Planning/outcomes: create measurable and achievable (SMART) goals for patient. Create interventions, objectives, and put in care plan so all professionals have access o Implementation: carry out the plan according to the care plan; care needs to be documented o Evaluation: both the pt’s status and the effectiveness of the nursing care needs to be reviewed and the care plan should be modified as needed after collecting objective data to evaluate o Anytime we implement something, you must revise plan of care When the pt is confused, who can the nurse obtain a health history/status from? Who are secondary sources for health history? o The primary source is the patient and they can be reliable, or non reliable (confused, intubated, sedated, non responsive, psych emergency) o Secondary sources include parent, next of kin, family, paramedics, EMT, client records/charts o If there is no secondary, & you don’t know if pt is reliable, proceed to physical assessment and document no reliable source Review difference between subjective/objective data o Subjective: patient’s perception, it cant be measured, such as pain, dizziness, itchiness o Objective: data that can be measured/validated, such as pulse rate, temperature, weight, skin conditions Difference between focused vs comprehensive/admission assessment o Comprehensive: include full assessment, vitals, and interview with patient (subject +objective). Depending on the CC, the nurse would then conduct a focused assessment, which is in greater detail depending on patient’s condition, and the comprehensive exam has been completed. What do positive or negative findings signify in physical assessments? o A positive finding would indicate the patient is showing signs/symptoms for that assessment/test. A negative test can indicate that the patient does not have the findings for that assessment o E.g. positive Babinski, negative murphy’s sign S/Sx/Assessment findings of: Left-sided Heart Failure o The problem is with the ventricles! Blood in the left side of heart just LEFT the lungs, so if there is heart failure it is going to pool back into the lungs. o Causes Include: o HTN, valve disease, myocardial disease, ischemic heart disease o Assessment findings include: o Pulmonary edema: excess fluids in lungs, causing: dyspnea/SOB, orthopnea (can’t lay flat d/t fluid in lungs so ask pt how many pillows they sleep on), chest pain, fatigue (d/t low O2 supply), shallow breathing/wheezing, crackles • Pink frothy sputum! o Peripheral Cyanosis (due to lack of oxygen being distributed) • Low perfusion of organs o Systemic resistance: hypoxic environment to systems/organs kills organs, causing confusion o Tachycardia o o S/Sx/Assessment findings of: Right-sided Heart Failure o The most common cause of right sided heart failure is left sided heart failure, d/t so much fluid building up, it causes pressure in the right side so you can have both at the same time. RHF is seen in cor pulmonale, which is related to chronic lung disease o Blood goes RIGHT back to the body and pools in veins o The IVC is in the liver so it causes hepatomegaly o Assessment findings: o Increased Jugular venous distention (JVD): blood is pooling back into the veins and can push fluid out of veins, into surrounding tissue ▪ o o o o *note: JVD is seen in everyone when supine, must elevate HOB to 30 degrees in order to assess Hepatomegaly *Peripheral dependent edema: pedal edema often present, weight gain, pitting edema (if NOT pitting, it’s lymphedema), large neck vein, a-fib, ▪ If lower extremity edema is unilateral, its NOT cardiac (may be DVT, or lymphedema) Fatigue: very lethargic because of all the fluid they’re carrying, and the heart can’t pump efficiently to get that blood everywhere Ascites: abdomen distention d/t hepatomegaly, this causes problems with breathing since it pushes on lungs, and anorexia d/t fluid pushing on stomach o o S/Sx/Assessment findings of: Myocardial Infarction o o TRUE cardiac pain hurts regardless of position, if pt reports pain when breathing, then its pulmonary o Treatment of an M.I. o Morphine, O2, nitroglycerin, Aspirin/Plavix o Vital signs may include: o Increased HR o Irregular pulse (a-fib, ventricular tachycardia) o Low BP (may be high at first in response to pain) What is syncope? Nursing precautions with syncope & fall precautions o Syncope: dizziness/fainting; ask patient what they were doing: o Emotional distress, micturition (holding breath while defecating), postural, o If dizziness is present while laying down & is aggravated by head movements, its neurological o Syncopal & fall precautions interventions: o Immediately check ABC’s o Have pt use walking aid o Have pt demonstrate they can use call light, lower bed all the way down o Have side rails up x4 o Adequate lighting o Pt to always use wheelchair o Remove excess equipment o Fall risk arm band and place sign in pt room, fall risk sticker on chart o Remain with pt while using bathroom What is the apical pulse? What is the significance? o Apical pulse, aka apex beat, is the point of maximal impulse. If pt has cardiomegaly then there can be an inferior or lateral displacement of PMI o In some medication administrations (digoxin, beta blockers) PMI is assed pre/post o In children up to 5, apex beat is more reliable d/t radial pulse are hard to palpate o In obese pts, apical pulse is preferred d/t peripheral pulses being hard to palpate o Used in pronouncing death o o Basics of S1, S2, S3, S4. What makes these sounds? o S1 Sound is made by the AV valves (tricuspid & Mitral) closing o Start of systole o Heard at APEX (bottom of heart) o S2 sound is made by the semilunar valves (pulmonic & aortic) closing o Start of diastole o Heard at base (top of heart) o o S3 is heard after S2 and sounds like a gallop (LUB-DUB-TA) o S4 is heard before S1 and sounds like TA-LUB-DUB o Both are irregular extra sounds we don’t want What is a carotid bruit? How do we assess? Is it concerning? o Often confused with tracheal breath sounds because it is auscultated in the neck, so the patient has to hold their breath while we assess o A bruit is similar to murmur, except a murmur is exclusive to heart valve, whereas a bruit is blood pooling in the carotid arteries and indicates turbulent blood flow o If pt has atherosclerosis, or plaque buildup, then the artery becomes narrow and blood struggles to pass, thus creating a ‘swooshing’ sound o Auscultate with the bell o Carotid bruit can indicate carotid stenosis, vascular disease, and can point to underlying disease that can cause stroke Location to assess Aortic, pulmonic, tricuspid, & mitral valve. o Stenosis vs. Regurgitation (heart valve diseases) o Stenosis is constriction/narrowing of heart valve opening or surface area—fixed and rigid o its narrow and doesn’t open all the way o low-pitched murmur best heard at mitral valve with bell o Regurgitation is incomplete closure of valve leaflets—backward flow of blood o It’s a loose valve, there isn’t a good ‘snap’ & it doesn’t close all the way o Best heard at mitral valve with diaphragm o o Basics of Myocardial Infarction o Heart attack, caused by lack of blood flow to the heart, usually d/t a blockage in one of the heart’s arteries o Heart muscle dies without blood, thus causing the heart to stop pumping which stops flow to the rest of the body o Most common cause is atherosclerosis o Heart ranges of: Sinus rhythm, bradycardia, and tachycardia o Sinus rhythm is the rhythm of a healthy heart. o 60-100 bpm o Sinus tachycardia is when your heart beats faster because of the electrical nodes sending signals. o 100-150 bpm o Can be normal in hard exercise, drugs, fever, anxiety o Sinus bradycardia is at type of bradycardia that originates in the SA node. o 50-60 bpm What is capillary refill time? What is being assessed? Significance of abnormal findings? o When pressure is applied to peripheral tissue, the amount of time it takes for distal blood flow to restore is called crt, or capillary refill time o Normal crt is < 3 seconds o If abnormal, can indicate dehydration or poor blood perfusion to that tissue o Note: be aware of pt condition, a crt of > 3 seconds is not always abnormal, if pt had surgery, expect crt to be delayed a few seconds What is dysphagia? What are aspiration precautions? nursing interventions for aspiration precautions? o Dysphagia: difficulty in swallowing; higher incidence in the elderly o can be due to neurological problems (after a stroke, Parkinson’s disease, Myasthenia gravis) or tumors in the mouth o Aspiration precautions: interventions to reduce the risk of aspiration of food, liquids, or secretions during the swallowing process o Foreign substances entering the airways may lead to pneumonia or suffocation o Always have suction tubing within reach o Aspiration interventions: o Feed small amounts of food: reduces risk of choking o Seat pt fully upright: opens up esophagus o Do not force feed o Provide oral care before and after meals: prevents pneumonias; bacteria can enter lungs if not cleaned properly, some people pocket food so always inspect the mouth o If pt not fully alert, do not put anything in mouth o Crush pills and put in soft food (pudding, applesauce) for those on soft food diets ▪ Check if pills can be crushed What is conjunctivitis? What are physical assessment findings for this infection? o Infection/inflammation of the conjunctiva (white part that lines the inner eye) of the eye o Assessment findings include: o Redness, eye crust, purulent discharge, itchiness, yellow/thick discharge o What is Exophthalmos? o “bulging of the eyes” o Some conditions, such as Grave’s disease, can cause this o Nursing interventions can include applying prescribed lubricants, provide emotional support, apply warm compress What is retinal detachment? S/Sx? o *an emergency!! It is loss of peripheral vision d/t retina detaching from supportive tissue o “curtains closing” o S/Sx: o Sudden onset of ‘floaters’ that are black** o Persistent painless blurred vision o Curtain like shadow o Flashes of light What is glaucoma? S/Sx? o Loss of peripheral vision with central vision lost last, o o The result of inadequate drainage of aqueous humor, it gets worse over time and causes blindness by damaging optic nerve o Usually no symptoms, but some experience pain and headaches What are cataracts? S/Sx? o An eye disease where the lens of the eye become opaque, causing vision to be blurred and unclear o What are nystagmus, ptosis, strabismus, myopia? o Nystagmus: involuntary flickering of the eye when held in a lateral position; EOM dependent on CN 3, 4, 6 o Ptosis: falling/drooping of the eyelid; can happen in disease where the CN’s are damaged, muscle strength is weak (myasthenia gravis), or welling o Strabismus: abnormal alignment of the eyes, the eyes don’t look in the same direction at the same time; causes include nerve injury, dysfunction in eye muscles o Myopia: being nearsighted, close things are clear but far objects are blurry, having to squint, causing headaches; may occur gradually and usually has no symptoms What is sinusitis, mastoiditis, and chronic allergies? o Sinusitis: inflammation of the sinuses that causes them to get blocked or filled with fluid o green/yellow discharge o Mastoiditis: infection affecting the mastoid bone that can occur if ear infection is untreated o Symptoms include: redness, swelling of mastoid process, fever, ear pain, ear discharge, headache, hearing loss in affected ear, o o Physical assessment findings of chronic allergies may include frequent sniffling, nasal discharge, sneezing, mouth breathing, watery eyes, pain on percussion Clinical assessment findings of Otitis media, Otitis externa, & presbycusis o Otitis media: infection of the middle ear; occurs primarily in children because their eustachian tube is shorter, making it harder to drain fluid from ear o o Otitis externa: inflammation/infection of external ear, “swimmers ear”, ear is red and edematous, itchy, painful, and can have hearing loss, o Interventions: cleansing outer canal, instill ear drops, adequate forms of communication since hearing loss can occur o o Presbycusis: age related hearing loss, gradual & in both ears; nursing interventions include patient education and emotional support, helping patient with hearing aid What is a gag reflex, its significance, and how is it a patient safety concern? o CN 9, 10 is responsible for this reflex, the medulla controls it o It is a contraction of the throat when something touches the top of it, or back of tongue o This reflex prevents us from choking or ingesting harmful substances o A patient can choke, aspirate without the gag reflex Causes, signs, symptoms, care of Bell’s Palsy. *(compare it to a TIA) o Causes include: tumors, nerve damage to CN 7, strokes, virus o Onset is acute/sudden and temporary, causing unilateral facial paralysis, pts cannot close L eye or raise L corner of mouth, will demonstrate loss of lower facial movement on side opposite stroke o Treatment should be fast because damage may be permanent, full function of face usually comes back within 3 months o o Nursing care includes protecting the eye that does not close, help patient do face exercises, keeping affected eye moist Neurological deficits of CN 1, 3, 4, 5, o o o o CN1 olfactory: loss of taste/smell (anosmia) CN 3 oculomotor: Diplopia, ptosis CN 4 trochlear: strabismus, diplopia CN 5 trigeminal: loss of facial sensation, decreased ability to chew, decreased blinking What is paralysis, hemiplegia, hemiparesis, flaccidity, and ataxia? o Ataxia: degenerative neurological condition that involves impaired balance and coordination. It resembles being drunk—slurred speech, stumbling, falling, lack of muscle control o o Flaccidity: neurological disorder that affects the grey matter of the spine which muscles and reflexes to become weak—loose and floppy limbs o adults can still get AFM, it is very rare o Hemiplegia vs hemiparesis: hemiplegia is total or severe loss of strength on one side (paralysis), and hemiparesis is mild/partial weakness in one side of body o Common cause is a stroke How would you document an abnormal gait? o Gait is not smooth and unsteady, balance is not maintained, patient not able to ambulate independently. Can be ataxic gait, parkinsonian gait, movements are not smooth or coordinated What is a Glasgow coma scale & significance? How does a nurse calculate? What to the scores mean? o Is an assessment tool used to assess LOC in patients with neurological deficits or following a traumatic injury o Nurse calculates score based on 3 main assessments: eye, verbal, and motor o Brain injury is classified as: o Severe if score is < 8 o Moderate if score is 9-12 o Mild if score is > 13 o o When applying painful stimulus, avoid ocular pressure or nipple twists, do a trapezius pinch, sternal rub, or nail pressure How II?nerve What is this CN? o do CNyou II istest the CN Optic and visual acuity is tested by using a Rozenbaum chart at a distance (14 ft) o Direct and consensual pupillary responses are tested o Direct: when direct light is applied to the eye, pupil should constrict equally and promptly o Consensual: when light is directed at the other pupil, they should both constrict What is PERRLA? Normal vs abnormal pupillary responses. What CN test this? o CN II, III test for PERRLA o Pupils equal round reactive to light and Accommodation ▪ Pupils should constrict with light ▪ Normal finding would be Positive perrla ▪ Abnormal finding would be dilated pupils (compressed CN III), bilateral dilated, fixed pupils (could be d/t brain injury, unconscious) o Having abnormal PERRLA is not a condition, but it does prompt for further testing by provider Assessment S/Sx of Respiratory Distress. Nursing Interventions o It is an EMERGENCY and is life threatening condition where a person cannot get enough oxygen into the body o Causes: o Direct lung injury: ▪ Pneumonia ▪ Aspiration ▪ Near-drowning ▪ Inhalation injury o Indirect lung injury: ▪ Sepsis ▪ Fat embolism ▪ OD o S/Sx of distress: ▪ Change in SpO2, BP, tachycardia/bradycardia, cyanosis (turning blue), retraction of lungs (intercostal, diaphragmatic), nasal flaring, confusion o Interventions: HIGH FOWLERS, apply O2, NPO, bed rest and energy conservation o Cyanosis is the skin turning blue d/t lack of oxygen; can be central or peripheral o Central: bluish discoloration of skin or mucous Mb d/t tissue near the skin having low O2 saturation o Peripheral: distal extremities discoloration d/t low O2 saturation (seen in LHF) o acute respiratory distress syndrome Respiratory Patterns: o Dyspnea: Shortness of breath o Rate dysfunction o Tachypnea: rapid & shallow breathing; occurs d/t imbalance of gas exchange, less O2 in body and higher CO2 o Higher than normal respiratory rate o Rate dysfunction o Bradypnea: slow & regular respirations; can happen in alcohol or drug OD, asthma, COPD, CO poisoning o Rate dysfunction o Hyperventilation: rapid & deep respirations; respiratory failure, fever, sepsis, exercise, anxiety o NOT higher than normal respiratory rate o It is an excessive ventilation than is needed to maintain a normal PaCo2—TOO much ventilation o Volume dysfunction o Hypoventilation: irregular & shallow respirations; insufficient ventilation to maintain a normal PaCo2, results in inadequate Oxygen supply o Volume dysfunction o Obstructive breathing: in obstructive lung disease, expiration is prolonged d/t narrowed airways increasing resistance to air flow. Causes are asthma, COPD, bronchitis o Cheyne-Stokes: periods of deep breathing alternating with apnea. Causes include heart failure, drug induced distress, brain damage o Percussion/Auscultation sounds with: pneumonia, atelectasis, COPD, pleural effusion o o Percussion is to determine if the underlying tissue is filled with air, solid, or is fluid o In pneumonia (infection of alveoli): would be flat & dull d/t the fluid in lungs o Atelectasis (collapse of lung/obstruction of airflow where alveoli can’t expand): would be dull over affected area o COPD: hyperresonance would be noted d/t being unable to fully exhale o Pleural effusion (fluid in pleural space): would be flat & full Auscultation o Pneumonia would present as crackles & rhonchi o Atelectasis: absent breathe sounds o COPD: rhonchi o Pleural effusion: diminished breath sounds, poor inspiratory effort Breath Sounds: Crackles, Wheezes, Rhonchi, Stridor o o o o o o CRACKLES: (aka rales) o Caused by opening of collapsed alveoli or when smaller airways have fluid, they are short/intermittent, fine, high pitched sounds as a result of air passing through fluid or mucous o Pneumonia, CHF, atelectasis, pulmonary edema o Wood burning in a fireplace RHONCHI: o Caused by secretions in large airways (bronchi); continuous lower pitch sounds, ▪ COPD, pneumonia, CF, bronchitis ▪ Rumbling rhonchi, it is turbulent but constant ▪ Can clear with coughing STRIDOR: EMERGENCY!! o Obstruction of larynx or trachea (‘choking’) o High pitched, loud during inspiration as result of foreign body aspirations or narrowing of upper airway after intubation WHEEZE: “musical” o Continuous sounds caused by narrowing of the airways, longer than crackles o Produced when air flows through narrow airways d/t mucous or bronchoconstriction o More on expiration ▪ Heard in COPD, asthma Assessment S/Sx of end stage liver failure. What is jaundice & ascites? o o o ESLD: most often the result of liver cirrhosis, where scar tissue replaces healthy liver tissue, and ascites and renal impairment are signs of end stage liver disease Ascites is a collection of fluid (edema) in the abdomen, causing less room for food, and can cause life threatening infection (peritonitis) S/Sx of ESLD: o Ascites, jaundice (high levels of bilirubin), edema, splenomegaly, gallstones, vomiting, weight loss, pain in stomach, nausea, bleeding varices that cause black tarry stool, Sequence of abdominal assessment and significance o o Inspection, auscultation, percussion, and palpation last If you palpate prior to auscultation you may move or create bowel sounds that are inaccurate 4 abdominal quadrants o o Xiphoid process is in epigastric region, umbilicus is in the center, iliac crests are in lower quadrants Clinical signs of constipation, appendicitis, cholecystitis, small bowel obstruction o o o Constipation: hard/lumpy stools, fewer than 3 stools a week Appendicitis o Pain when releasing palpation of LRQ abdomen (rebound tenderness) o Fever, loss of appetite, diarrhea Cholecystitis o o Pain when releasing palpation to RUQ (+ murphy’s sign) during inspiration o Fever, jaundice, bulging stomach, shoulder pain Small bowel obstruction: severe constipation, dehydration, malaise, bloating, vomiting, nausea, hypoactive bowel sounds Gastroenteritis: what is it? Nursing interventions? Assessment findings? o o o Acute gastritis is the irritation and inflammation of the stomach’s mucous lining. It may be caused by thermal, chemical, bacterial insult “food poisoning” o Drugs, alcohol, aspirin, chemotherapeutic agents o Hot, spicy, rough or contaminated foods Nursing interventions: o Assess vitals, pain, analgesic, o Watch for orthostatic hypotension (FALL risk), hypokalemia, o Fluid/electrolyte replacement, protective cream barrier recommended S/Sx include diarrhea, nausea, fever, vomiting, poor skin turgor, low BP, cramping, oliguria Normal intake/output? Assessment findings for: fluid excess, fluid deficit? o o o o Normal I/O in 24 hours is 1-2 L Physical assessment of someone with fluid volume excess (hypervolemia): o Swelling in extremities, discomfort, cramping, HTN caused by fluid in bloodstream o Bounding pulse, crackles, altered LOC, impaired urine output (decreased output if KD’s are the reason), pitting edema, pale/cool skin, weight gain, ascites, decreased sodium, BUN, hematocrit Physical assessment of someone with fluid volume deficit (hypovolemia): o Increased pulse, orthostatic bp, diminished pulses, dyspnea, lethargy, decreased urine output, dry skin, poor turgor, constipation Skin turgor: the skin’s elasticity, it is the ability of skin to change shape and bounce back to normal—if the skin doesn’t bounce back, it means dehydration Define: o o o o o o o Nocturia: frequent urination at night Hematuria: blood in urine Dysuria: pain with urination Polyuria: a LOT of urine > 3-4 L in 24 hours Oliguria: too LITTLE urine < 700 mL in 24 hours (less than 30 mL in 1 hour) Urgency: having to go right away and being unable to hold it Anuria: no urine (dialysis) What is an AV fistula? How do nurses assess function? o During hemodialysis, the dialyzer need ‘access’ and an AV (arteriovenous) fistula is an access point o o o o it is the creation of a super highway (connection of an artery and vein made by surgery) and is the most common access site for hemodialysis patients Arteriovenous point is an access point needed for the dyalisis machine Nurses can assess an AV fistula by ‘hearing the bruit’ & feeling the thrill o A bruit will sound like a whistle or hight pitched noise, you DONT want this because it means the vein got narrow o You should feel the thrill thought because that means that the thrill/vibration is the blood flowing NO BP, NO IV, BLOOD DRAWS R/L ARM o Nursing interventions: o Don’t sleep on that arm o o o No tight clothing Monitor diet and fluids No HTN meds What is creatinine level? Normal range? Significance of elevation? o Creatinine is protein waste product that is excreted by the kidneys. Values of creatinine tell us how well the kidney is working. It is indicative of kidney function! o Normal is 0.5-1.2 mg/dL o An elevation in creatinine would mean impaired kidney function since there is more in the bloodstream o If creatinine is high, so is K+ because the kidneys are impaired and cant secrete them properly, body would then be in metabolic acidosis What is urethral stricture, paraphimosis, urethritis, phimosis. Assessment findings of each? o o Urethral stricture: this can cause urinary retention; it is a narrowing of the urethra that restricts flow or urine from bladder & can cause inflammation or infection o Catheter can be inserted to drain urine is the usual first step, then surgery o Findings would be fluid retention, UTI (infection, fever, pain) Paraphimosis: The foreskin becomes trapped behind the glans and can’t be pulled forward anymore. This leads to a lack of blood flow resulting in gangrene (EMERGENCY) o This can be avoided if nurse remembers to pull the skin forward at the end! Would require surgical intervention o o o o Phimosis: condition of the foreskin of uncircumcised men can’t be pulled back, this can lead to inflammation—not a medical emergency but there is great risk for inflammation Urethritis: inflammation of the urethra; can be caused by STI, & prsents as swelling, irritation, dysuria, frequent urination, discharge, Hydrocele Vs Varicocele: findings & significance o Hydrocele is when the scrotal area has a lot of fluid o o o Can be associated with underlying condition that can cause serious complications, such as infection or tumor Varicocele is a collection of small veins in the scrotum that feels like a ‘bean bag’ o Common cause of low sperm count, infertility, and can cause testicles to fail to develop normally or shrink o ▪ Orchitis vs prostatitis o o Orchitis: inflammation of one of both testicles. Bacterial or viral infection can cause this or STI o Acute infection of the testis o Complication of a systemic disease (mumps) or related to epididymitis Prostatitis: prostate gland disorder (prostate inflammation) o Inflamed prostate which narrows the urethra, symptoms include difficulty urinating, pain in the groin, pelvic area, or genitals, and sometimes flu-like symptoms . o What is Gravida and para? o o o Gravidity is the number of times a woman has been pregnant Parity is the number of times a woman has given birth to a fetus over 20 weeks E.g., G6 P6; pregnant female currently 10 weeks pregnant, has 3 living children, hx of 2 abortions Breast examination: what is included? Documentation x inspection/palpation? o o o Gown should be own backwards for access Inspection: arms relaxed, arms raised, hands on hips, and bending over; assess breast symmetry , skin changes (any dimpling, edema, ulceration), inspect nipples for symmetry and retractions, discharge Palpation: breast, axilla, ENTIRE chest wall o Pain, masses, lymph nodes o Tail of spence o o o Documentation: breasts are rounded, symmetric, color is consistent, skin uniform in color, smooth, intact, no visible lesions, masses or lymphadenopathy to axilla or supraclavicular areas to document a mass: axis of breast as if looking at a clock, location relative to nipple, quadrant, size of mass, location, characteristics (firm, mobile, defined) Examination of breast cancer: nursing care after mastectomy (IV/BP) o Have patient stand the assessment positions and inspect then palpate (press down, circular motions, steady pressure to chest wall) o Palpate nipple also o Always palpate the area NOT of complaint to get a baseline o 3 methods of palpation: ▪ Up and down, 4 quadrants, or circular o If nipple is inverted it’s a sign of malignancy o Palpate into the axilla and have the patient ‘flex’, forming a teacup o o Palpation: feeling for masses, fixed, stuck, firm masses are more malignant After care of mastectomy: removal of breast tissue and lymph nodes (men too) if patient had a mastectomy done, the nurse should: ▪ NOT take BP, vitals or IV in that arm, if both breasts removed, then BP on leg ▪ Arm should be elevated to promote fluid return ▪ Encourage compression garments What is a macule, papule, vesicle? How to document abnormal findings? o o o o o macule < 1cm, (MacBook is flat) patch is flat > 1 cm papule is solid and elevated > 1cm plaque elevation > 1cm vesicles elevation with clear fluid ABCDE and the significance of the findings o use the abcde technique to assess for melanoma/malignancies o o Melanomas kill & are not benign, the best way to prevent them is to wear SPF What is lymphedema o Tissue swelling resulting from excessive retention of lymphatic fluid in the interstitial compartment and by impaired drainage. o o Assessment should include visual examination of skin, palpation and feeling for pitting edema, firmness, induration, and warmth, determine ROM What is a hernia? Common locations and names for hernias? How would they present? o o o o A hernia is when an organ or fatty tissue squeezes or bulges through an area surrounded by muscle (fascia) With Valsalva means that the patient is holding down their breath and bearing down, you can see the hernia more Men get more inguinal hernias, women get more umbilical hernias S/Sx for fractures, subcutaneous emphysema, crepitation and joint dislocation o o o o With a fracture, patient can lose up to 1.5 L of blood. With fractured bones there is BLOOD LOSS. If the patient is in shock from acute hemorrhage, patient will be hypotensive and tachycardic Crepitation is a sensation you can hear or feel when you move a joint. Common cause can be arthritis of joint injury Subcutaneous emphysema: when air travels under the skin o Sx include wheezing, limited ROM, swelling Joint dislocation: abnormal separation in the joint where 2 bones meet