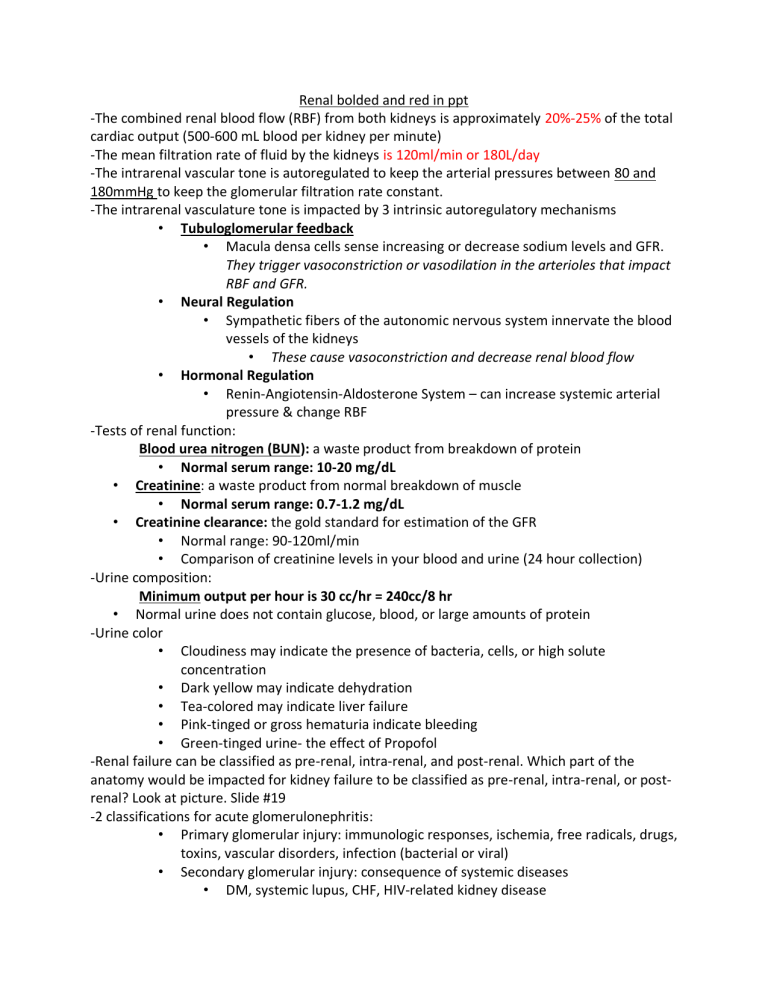
Renal bolded and red in ppt -The combined renal blood flow (RBF) from both kidneys is approximately 20%-25% of the total cardiac output (500-600 mL blood per kidney per minute) -The mean filtration rate of fluid by the kidneys is 120ml/min or 180L/day -The intrarenal vascular tone is autoregulated to keep the arterial pressures between 80 and 180mmHg to keep the glomerular filtration rate constant. -The intrarenal vasculature tone is impacted by 3 intrinsic autoregulatory mechanisms • Tubuloglomerular feedback • Macula densa cells sense increasing or decrease sodium levels and GFR. They trigger vasoconstriction or vasodilation in the arterioles that impact RBF and GFR. • Neural Regulation • Sympathetic fibers of the autonomic nervous system innervate the blood vessels of the kidneys • These cause vasoconstriction and decrease renal blood flow • Hormonal Regulation • Renin-Angiotensin-Aldosterone System – can increase systemic arterial pressure & change RBF -Tests of renal function: Blood urea nitrogen (BUN): a waste product from breakdown of protein • Normal serum range: 10-20 mg/dL • Creatinine: a waste product from normal breakdown of muscle • Normal serum range: 0.7-1.2 mg/dL • Creatinine clearance: the gold standard for estimation of the GFR • Normal range: 90-120ml/min • Comparison of creatinine levels in your blood and urine (24 hour collection) -Urine composition: Minimum output per hour is 30 cc/hr = 240cc/8 hr • Normal urine does not contain glucose, blood, or large amounts of protein -Urine color • Cloudiness may indicate the presence of bacteria, cells, or high solute concentration • Dark yellow may indicate dehydration • Tea-colored may indicate liver failure • Pink-tinged or gross hematuria indicate bleeding • Green-tinged urine- the effect of Propofol -Renal failure can be classified as pre-renal, intra-renal, and post-renal. Which part of the anatomy would be impacted for kidney failure to be classified as pre-renal, intra-renal, or postrenal? Look at picture. Slide #19 -2 classifications for acute glomerulonephritis: • Primary glomerular injury: immunologic responses, ischemia, free radicals, drugs, toxins, vascular disorders, infection (bacterial or viral) • Secondary glomerular injury: consequence of systemic diseases • DM, systemic lupus, CHF, HIV-related kidney disease • S/S: hypoalbunemia/ proteinuria -Chronic glomerulonephritis= progressive glomerular damage leading to chronic kidney disease (CKD) • Patho: Hypercholesterolemia, proteinuria, diabetes, lupus, sclerotic disease, or an inflammatory process causes progressive glomerular injury over many years-> chronic renal insufficiency (CRI)->nephrotic syndrome-> ESRD -Nephrotic syndrome= urinary excretion of 3.5 grams or more of protein/day • Characteristic of a glomerular injury • Patho: Glomerular injury->increased glomerular filtration membrane permeability to protein-> loss of plasma proteins and immunoglobulins->decreased vascular oncontic pressure->interstitial edema. Manifestations: • Hypoalbunemia/Proteinuria of >3.5 grams/day (classic sign) • Peripheral edema • Foamy urine (classic sign) -Nephritic syndrome= proteinuria, but < 3.5 grams in the urine per day, microscopic hematuria, and RBC casts in the urine • Occurs primarily w/ infection-related glomerulonephritis and rapidly progressive crescentic glomerulonephritis, lupus nephropathy, and diabetic nephropathy • Patho: Damage to the glomerulus-> increased glomerular filtration membrane permeability->pores large enough for RBCs and some protein -Acute kidney injury= sudden decline in renal function secondary to ischemic injury w/ a decrease in glomerular filtration and urine output • Classified as: Pre-renal, intrarenal, or post-renal • Patho: Inadequate renal perfusion->decrease in GFR->ischemic cellular injury->acute tubular necrosis (ATN) Manifestations • New onset oliguria (classic sign) • Sharp elevation in BUN/Creatinine (classic sign) • Hyperkalemia (classic sign) -Renal insufficiency=GFR reduced by 25% of the normal • It is a descriptive term, and is not specific to a certain disease process -CKD= Progressive loss of renal function associated w/ chronic systemic diseases • Patho: Chronic injury to the nephrons-> glomerular injury with decreased GFR-> decreased ability to filter out BUN, creatinine, drugs, and increased loss of protein • Manifestations • Generalized edema (classic sign) • Weight gain (classic sign) • Uncontrolled HTN (classic sign) • Chronic anemia (classic sign) -Upper urinary tract obstruction= an anatomical or functional obstruction of the upper urinary tract (kidneys/ureters) that impedes flow of urine, increases the risk for infection, and compromises renal fxn. • Patho: Obstruction->dilation of the ureter, renal pelvis, and kidneys->glomerular damage->decreased filtration->renal failure. -Kidney stones: pH>7 increases the risk for calcium stones • pH<5 increases the risk for uric acid stones Patho: Related to one of 4 mechanisms • Supersaturation of one or more salts in the urine • Precipitation of the salts from a liquid to a solid state • Growth through crystallization (AKA agglomeration) • Absence of stone inhibitor agents Manifestations: • Renal colic (classic sign) Size: • < 5mm → 50% spontaneous passage • 1cm or > → almost NO chance of passage -Renal tumors: Manifestations: • hematuria (classic sign) • flank pain (classic sign) -Lower urinary tract obstructions= an anatomical or functional obstruction of the bladder or urethra -Types of Incontinence • Urge incontinence: Involuntary loss of urine that is abrupt with urgency issues • R/t involuntary contractions or decreased bladder wall compliance. • Stress incontinence: Involuntary loss of urine w/ coughing, sneezing, laughing, or activities that increase abdominal pressure. • Overflow incontinence: Involuntary loss of urine with overdistention of the bladder from a urethral obstruction, or a neurological lesion. • Mixed incontinence: Combination of stress and urge incont. • Functional incontinence: Involuntary loss in patients with dementia or immobility -Acute cystitis: Patho: Retrograde movement of bacteria up the urethra and into the sterile bladder. Bacteria resist flushing and cause inflammation of the bladder wall. -Acute pyelonephritis= acute infection of ureter, renal pelvis, and/or renal parenchyma -Pediatric considerations • GFR does not reach adult rate until 1 to 2 years old • Newborns have decreased ability to efficiently remove excess water and solutes • Narrow margin for fluid and electrolyte balance • Increased risk of drug toxicity -Polycystic kidney disease= an autosomal dominant or autosomal recessive cystic kidney disease -IgA nephropathy= most common form of glomerulonephritis in children • Patho: Immunoglobulin A and complement proteins deposit in the glomerulus->cause inflammation and dysfunction of the nephrons -HUS (hemolytic-uremic syndrome) is the most common cause of acute renal failure in children -Nephroblastoma= a rare embryonic tumor of the kidney • Also known as Wilm’s tumor