Antidysrhythmic Drug Guide: Classes, Medications, & Monitoring
advertisement

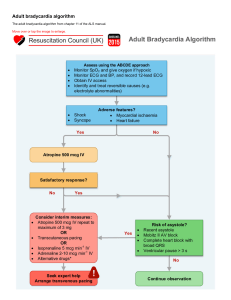
Antidysrhythmic Medication - Drug Therapy Class I: Sodium Channel Blockers Disopyramide Phosphate ● Monitor BP and HR; hypotension and bradycardia can occur Lidocaine ● Monitor for arrhythmias; these agents affect conduction patterns, sometimes increasing the frequency or severity of dysrhythmias. ● Monitor for CNS side effects such as dizziness, anxiety, ataxia, insomnia, confusion, seizures, and GI distress; may require dose reduction or discontinuation ● Monitor for signs of heart failure; can cause HF. Propranolol ● Monitor HR and BP; bradycardia and decreased BP are expected effects. Acebutolol ● Assess for wheezing or shortness of breath; can cause bronchospasm. Esmolol ● Assess for insomnia, fatigue, and dizziness; may require dose reduction or discontinuation Mexiletine hydrochloride Flecainide acetate Propafenone hydrochloride Class II: Beta Blockers Sotalol ● Assess ventricular arrhythmias, can have proarrhythmic effects. Class III: Potassium Channel Blockers - Delays repolarization and prolongs the QT interval. Sotalol ● For all class III potassium channel blockers: atrial and ventricular dysrhythmias. ● Monitor BP and HR. hypotension and bradycardia can occur. ● Monitor for arrhythmias. agents affect conduction patterns, sometimes increasing the frequency or severity of dysrhythmias. ● Continually monitor ECG rhythm during infusion. bradycardia and AV block can occur. ● This drug can cause serious toxicities (lung damage, visual impairment). Approval is limited to use for life-threatening dysrhythmias. However, because of efficacy, use remains very common. ● Corneal pigmentation occurs in most patients, generally does not interfere with vision. ● Teach patient to take with meals and avoid grapefruit juice. better absorbed with food. Grapefruit juice alters the effect. ● Teach patient to notify provider with signs of HF. contraindicated for pts with HF. ● Stop infusion as soon as the dysrhythmia is terminated or in the event of VT. may cause potentially fatal dysrhythmias. ● Assess potassium and magnesium levels before infusion because electrolyte balance must be corrected prior to and during use. ● Teach patient to change positions slowly. Orthostatic hypotension is a side effect. Verapamil ● Monitor HR and BP; bradycardia and hypotension are common side effects. Diltiazem ● Teach patients to change position slowly when receiving oral therapy. orthostatic hypotension can occur. ● Teach patients to report dyspnea, orthopnea, distended neck veins, or swelling of the extremities. HF can occur, necessitating a decrease in dosage or discontinuation. ● Assess apical HR before administration; decreased HR is an expected response. ● Teach patient to report nausea, vomiting, diarrhea, paresthesias, confusion, or visual disturbance. can indicate digoxin toxicity. ● Monitor HR and rhythm after administration. increased heart rate is expected. Adenosine ● paroxysmal SVT ● Be sure to have emergency equipment readily available!. Significant bradycardia with pauses, nausea, and vomiting. Nursing Safety Priority ! ● Facial flushing, shortness of breath, and chest pain are common side effects. Amiodarone ● atrial and ventricular dysrhythmias. Dronedarone ● AF and atrial flutter. Ibutilide ● AF and atrial flutter Dofetilide ● AF and atrial flutter Class IV: Calcium Channel Blockers Class: Other Digoxin ● AF and atrial flutter. Atropine ● Bradycardia