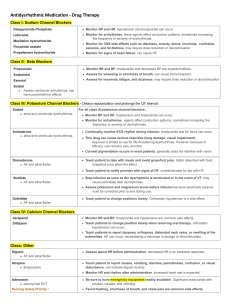
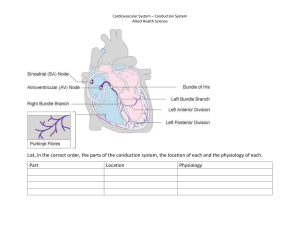
PATH 222 Cardiac Dysrhythmias (Arrhythmias) VanMeter and Hubert Chapter 12; LeMone et al. p. 895-897; Adams, Chapter 55 Week 2 Review the cardiac conduction system. Figure 55.1 Adams et al. (2nd Canadian ed.) p. 697 a) sino-atrial node (pacemaker) in the right atrium generates impulses at approximately 70/minute (automaticity = the ability to spontaneously generate an action potential without direction from the nervous system called sinus rhythm can be affected by the autonomic nervous system and by hormones such as epinephrine b) impulses spread through the atrial pathways and the atria contract c) atrio-ventricular node located on the floor of the right atrium d) impulses continue into the ventricles through the Bundle of His, right and left bundle branches and Purkinje fibers, resulting in ventricular contraction Review the cardiac cycle in VanMeter and Hubert 5th ed. page 227 - 228. Cardiac output the volume of blood ejected by a ventricle in one minute depends on heart rate and stroke volume stroke volume varies with sympathetic stimulation and venous return, eg. increased venous return leads to increased force of contraction Define arrhythmia/dysrhythmia. Classification of dysrhythmias according to the type of rhythm abnormality produced and its’ location those that originate in the atria – supraventricular most common type of dysrhythmia is called atrial fibrillation – a complete disorganization of rhythm, resulting in a heart rate of > 350 beats per minute dysrhythmias originating in the ventricles are the most serious – explain why Causes of arrhythmias damage to the conduction system of the heart – what could cause this? electrolyte imbalances (review the effects of hypo and hyperkalemia) fever hypoxia stress infection drug toxicity, such as occurs with digoxin Effects of arrhythmias reduced efficiency of the heart’s pumping cycle A slight increase in heart rate can be compensatory and increases cardiac output What is the effect of a very rapid heart rate on the cardiac output and explain why this occurs? What is the effect of a very slow heart rate on cardiac output and oxygen perfusion to the tissues? What is the effect of irregular contractions on the normal functioning of the heart? Sinoatrial node abnormalities include: bradycardia vagal stimulation tachycardia normal response to sympathetic stimulation compensatory response to decreased blood volume Atrial Conduction Abnormalities the most common dysrhythmias atrial fibrillation – atrial heart rate of over 350 beats per minute; causes pooling of blood in the atria; treated with anticoagulant medication to prevent clotting and potential CVA Drugs Used to Treat Dysrhythmias Review action potential in myocardial muscle cells in Adams et al., page 699-700. Figure 55.4 Adams et al. (2nd Canadian ed.) p. 701 General mechanism of action of the drugs alter the electrophysiological properties (response to an action potential) of the heart by: -blocking the flow of ions through ion channels -altering activity of the autonomic nervous system Antidysrhythmics drugs are grouped according to their effect on the action potential 4 classes of antidysrhythmic drugs: Class I – sodium channel blockers Class II – beta-adrenergic blockers Class III – potassium channel blockers Class IV – calcium channel blockers Class V – miscellaneous drugs Remember that these drugs have a narrow margin between a therapeutic and a toxic effect. They may, in fact, worsen existing dysrhythmias or create new dysrhythmias. Class I – Sodium Channel Blockers – the largest class of antidysrhythmic drgus block the sodium channels and therefore, prevent depolarization results in a slowing of the action potential across the myocardium and suppresses the areas of ectopic pacemaker activity – what does this mean? Prototype drug is procainamide (Pronestyl) Class II – Beta-adrenergic Blockers slow heart rate (negative chronotropic effect) slow conduction velocity through the AV node most effective against tachycardia caused by excessive sympathetic stimulation prototype drug is propranolol (Inderal) – a non-selective beta-adrenergic blocker, affecting beta-1 receptors in the heart and beta-2 receptors in the pulmonary and vascular smooth muscle explain why hypotension is an adverse effect of propranolol explain why bradycardia is an adverse effect of propranolol Class III – Potassium Channel Blockers – usually not first-line drugs due to adverse effects block potassium ion channels in myocardial cells recall that when the myocardial cell has been depolarized, repolarization depends on the removal of potassium from the cell these drugs delay repolarization of the myocardial cells and lengthen the refractory period, which tends to stabilize dysrhythmias prototype drug is amiodarone (Cordarone) – also blocks sodium channels Class IV – Calcium channel blockers block calcium ion channels, thus inhibiting the flow of calcium into both myocardial and vascular smooth muscle cells slow conduction velocity by reducing automaticity in the SA node and slowing impulse conduction through the AV node, thus prolonging the refractory period effective against supraventricular dysrhythmias only prototype drug – verapamil (Isoptin) what will these drugs do to blood pressure and why? Miscellaneous drugs Digoxin decreases automaticity of the SA node slows conduction through the AV node