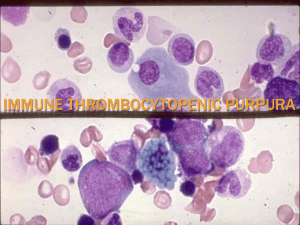
Thrombocytopenia Lecture Learning objectives Definition of Thrombocytopenia • Thrombocytopenia is a platelet count below the normal range (< 150,000/mm3) that is most commonly due to: • impaired platelet production in the bone marrow • Or • increased platelet turnover in the periphery. Etiology of Thrombocytopenia • Impaired platelet production in bone marrow • Bone marrow conditions → ↓ megakaryocytes → ↓ thrombopoiesis • Bone marrow failure: aplastic anemia, paroxysmal nocturnal hemoglobinuria • Bone marrow suppression: drugs (e.g., linezolid, daptomycin, valproic acid, valacyclovir), chemotherapy, radiation • Congenital thrombocytopenias: Wiskott-Aldrich syndrome, Alport syndrome, BernardSoulier syndrome, Fanconi anemia, von Willebrand disease • Other congenital conditions: Gaucher disease • Infection: CMV, EBV, hepatitis C virus, HIV, mumps and rubella, parvovirus B19, rickettsia, VZV, dengue • Malignancy: leukemia, lymphoma, bone marrow infiltration, myelodysplastic syndrome • Nutritional deficiency: vitamin B12 deficiency and/or folate deficiency (e.g., in chronic alcohol abuse) • Other: necrotizing enterocolitis Etiology of Thrombocytopenia • Increased platelet turnover in the periphery • Immune thrombocytopenia (ITP) and other autoimmune diseases (e.g., systemic lupus erythematodes, rheumatoid arthritis) • Disseminated intravascular coagulation (DIC) and sepsis • Thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) • Drug-induced immune thrombocytopenia (DITP): Platelet-activating antibodies cause a hypercoagulable state and simultaneous reduction in platelet count. • The following drugs are most likely to be associated with DITP: • • • • • • • • • • • Sodium-channel blockers: quinine, class I antiarrhythmics (e.g., quinidine), carbamazepine Calcium-channel blockers: valproate Antibiotics: linezolid, vancomycin, TMP-SMX, penicillin, ceftriaxone, rifampin Antiviral agents: ganciclovir, protease inhibitors (e.g., indinavir), zidovudine Antithrombotic agents: glycoprotein IIb/IIIa inhibitors (e.g., abciximab), heparin Others: oxaliplatin, suramin, ibuprofen, mirtazapine Heparin-induced thrombocytopenia (HIT) Pregnancy: preeclampsia and HELLP syndrome Infection (see above) Post-transfusion thrombocytopenia Mechanical damage due to artificial cardiac valves or extracorporeal circulation (e.g., dialysis) Clinical features of Thrombocytopenia • Bleeding of mucous membranes, e.g.: • Epistaxis • Bleeding gums • Gastrointestinal bleeding • Cutaneous and subcutaneous bleeding, e.g.: • • • • Petechiae Purpura Superficial ecchymoses Easy bruising • Menorrhagia • Prolonged and excessive bleeding after surgery Clinical features of Thrombocytopenia Clinical features according to platelet count Platelet count Mild Moderate Severe Symptoms •> 70,000–149,999/mm3 •Typically: no abnormal bleeding, i.e., asymptomatic thrombocytopenia •20,000–70,000/mm3 •Prolonged bleeding following surgery or trauma •Easy bruising •Occasionally: petechiae and purpura •< 20,000/mm3 •Spontaneous bruising (ecchymoses), petechiae, and purpura •Bleeding from the mucosa (e.g., bleeding gums) or after minimal trauma •Increased risk of spontaneous, lifethreatening bleeding Superficial, petechial bleeding indicates defects of primary hemostasis, whereas large, palpable ecchymoses and deep tissue bleeding suggest defects of secondary hemostasis! Diagnostic Approach • Confirm the diagnosis in all patients: • Repeat CBC and compare with previous platelet counts. • Consider peripheral blood smear to exclude pseudothrombocytopenia. • Investigate for underlying causes with a thorough history and routine laboratory studies. • If the etiology remains unclear: • Evaluate recent medication (see “Etiology”). • Order additional investigations based on clinical suspicion, e.g., evaluation for Myelodysplastic syndromes (MDS) or other malignancies in patients > 60 years old with new-onset thrombocytopenia. • Do not delay treatment for diagnostic testing in patients with significant bleeding or new neurological symptoms. Diagnostic Approach • Routine laboratory studies • CBC: ↓ platelet count (< 150,000/mm3); depending on the etiology, anemia or pancytopenia may be present. • Coagulation studies: ↑ bleeding time • Peripheral blood smear • Renal function tests • Liver chemistries Differential diagnoses • Pseudothrombocytopenia (Spurious thrombocytopenia) • A spuriously low platelet count seen in laboratory studies that occurs due to platelet clumping in vitro. Automatic counters mistake platelet clumps for individual platelets or white blood cells. Clumping can occur secondary to sampling issues (e.g., technique, anticoagulant used in collection tubes) or disease factors (e.g., antibodies to EDTA anticoagulant, viral infections, malignancy) • Dilutional thrombocytopenia: Falsely low platelet concentration due to volume overload; typically affects all other cell counts (i.e., associated dilutional anemia and leukopenia) Differential diagnosis of platelet disorders TTP Disseminated intravascular coagulation (DIC) •ADAMTS13 defi ciency •Systemic coagulation activation •Platelet and coagulati on factor consumption (mixed disorder) •Antiplatelet anti bodies (AntiGpIIb/IIIa) •Previously healthy adult, •Toddler or preschool sometimes associated er with history with triggers (e.g., of diarrheal illness infection, •Presents surgery, pregnancy) with petechiae, jaundi •Presents with mental ce, and oliguria status changes, fever, petech iae, fatigue, and pallor •Patient with a history of serious underlying illness (e.g., sepsis, trauma, malignancy) •Presents with thrombosis, embolism, organ dysfunction, and/or bleeding •Asymptomatic or presenting with petechiae, purpura, epistaxis, menorrhagia, gingival bleeding •+/- Schistocytes •↓ Platelets •Normal platelet m •Giant platelets •↓ Platelets orphology •Abnormal ristocetin •↓ Platelets cofactor assay •Normal/increased •Increased •Normal D-dimer, fibrin •Normal/increased degradation products •Increased •Normal HUS •Endothelial cell Pathophysiology dysfunction due to bacterial toxins Typical presentation •+ Schistocytes Peripheral smear •↓ Platelets PT (INR) and aPTT •+ Schistocytes •↓ Platelets Immune thrombocytopenic purpura (ITP) Bernard-Soulier syndrome Glanzmann thrombasthenia •Aggregation •Adhesion disorder: disorder: deficient platelet GPIb deficient platelet GPII -IX b-IIIa •Autosomal recessive •Autosomal recessive •Normal platelets •Abnormal results on platelet aggregation testing confirm the diagnosis. Immune thrombocytopenia (ITP) • ITP is a type of thrombocytopenia involving the formation of autoantibodies against platelets. • Primary immune thrombocytopenia: an autoimmune disorder characterized by isolated thrombocytopenia (< 100,000/mm3) with no known precipitating cause • Secondary immune thrombocytopenia: an autoimmune hematologic disorder causing isolated thrombocytopenia that is secondary to an identifiable trigger • Newly diagnosed ITP: all cases within the first 3 months of diagnosis • Persistent ITP: ITP lasting 3–12 months • Chronic ITP: ITP lasting > 12 months Immune thrombocytopenia (ITP) • • • • Epidemiology Prevalence: up to ∼ 10 per 100,000 ♀>♂ Children • Highest prevalence in children < 5 years of age • Typically self-limiting after a viral infection; 80% of cases resolve within 12 months [4] • Adults • Highest prevalence in individuals > 55 years of age • 80% of patients develop chronic ITP. • An incidental finding on a routine CBC in 25% of cases Immune thrombocytopenia (ITP) • Etiology • Primary ITP: idiopathic (most common) • Secondary ITP associated with: • Autoimmune disorders: SLE, antiphospholipid syndrome • Malignancy: lymphoma, leukemia (particularly CLL) • Infection: HIV, HCV • Drugs: e.g., quinine, beta-lactam antibiotics, carbamazepine, heparin, vaccines, linezolid, sulfonamides, vancomycin, TMP-SMX, antiepileptics Immune thrombocytopenia (ITP) • Antiplatelet antibodies (mostly IgG directed against, e.g., GpIIb/IIIa, GpIb/IX) bind to surface proteins on platelets → sequestration by spleen and liver → ↓ platelet count → bone marrow megakaryocytes and platelet production increase in response (in most cases). • In some cases, platelet production may be impaired because of destruction within the bone marrow or inhibition of megakaryocytopoiesis. Immune thrombocytopenia (ITP) • Clinical features can correlate with platelet count • Most commonly • Asymptomatic • Splenomegaly is typically absent. • Minor mucocutaneous bleeding (less common) • Subcutaneous: e.g., bruising, petechiae, purpura • Mucosal: e.g., mild epistaxis, gingival bleeding • Other types of bleeding (rare) • • • • Gastrointestinal: e.g, melena Genitourinary: e.g., hematuria, menorrhagia CNS: e.g., features of intracranial hemorrhage Prolonged or excessive traumatic or surgical bleeding • Splenomegaly is very unusual in ITP and makes other diagnoses more likely! • There should be suspicion for ITP in a child with thrombocytopenia and petechiae following a viral illness! Immune thrombocytopenia (ITP) • ITP is a diagnosis of exclusion; patients typically have a low platelet count with no other abnormalities. • Laboratory studies • Routine • CBC: ↓ platelet count (< 100,000/mm3) • Coagulation panel: usually normal • Bleeding time: may be prolonged • Peripheral blood smear: normal to large platelets • Additional investigations • All adults: HIV and HCV screening • Bone marrow biopsy • Consider in atypical cases or if there is diagnostic uncertainty • Findings: normal or ↑ megakaryocytes • Additional testing as required: consider in suspected secondary ITP, e.g., antinuclear antibodies in SLE or H. pylori testing if the patient has GI symptoms or is from a high prevalence area Immune thrombocytopenia (ITP) • Indications for observation • Children: no symptoms or only mild mucocutaneous bleeding with any platelet count • Adults: no symptoms or minor mucocutaneous bleeding with a platelet count of ≥ 30,000/mm3 • All patients: Refer to hematology for regular monitoring and counseling on bleeding risks. • First-line medical therapy • Preferred: Corticosteroids • Dexamethasone • OR prednisone • Alternatives: if contraindication, non-response, or intolerance to corticosteroids • Intravenous immunoglobulin (IVIG) • OR anti-Rho(D) immunoglobulin • Anti-Rho(D) immunoglobulin can cause potentially fatal intravascular hemolysis in patients with ITP. Close monitoring is recommended. Thrombotic thrombocytopenic purpura • Thrombotic thrombocytopenic purpura (TTP) is a thrombotic microangiopathy, a condition in which microthrombi, consisting primarily of platelets, form and occlude the microvasculature (i.e., the arterioles and capillaries). • Etiology • ADAMTS13 deficiency/inhibition • Acquired TTP (∼ 95%): autoantibodies against ADAMTS13 (see “Pathophysiology” below) • Congenital TTP (∼ 5%): gene mutations resulting in deficiency of ADAMTS13 • Risk factors • Drugs • Pregnancy • Systemic disease: cancer, HIV, SLE, infections Thrombotic thrombocytopenic purpura • Pathophysiology • Autoantibodies or gene mutations → deficiency of ADAMTS13 (a metalloprotease that cleaves von Willebrand factor) • ↓ Breakdown of vWF multimers → vWF multimers accumulate on endothelial cell surfaces • Platelet adhesion and microthrombosis • Microthrombi → fragmentation of RBCs with schistocyte formation → hemolytic anemia • Arteriolar and capillary microthrombosis → end-organ ischemia and damage, especially in the brain and kidneys (potentially resulting in acute kidney injury or stroke) Thrombotic thrombocytopenic purpura • Mnemonic for TTP symptoms: “Nasty Fever Ruined My Tubes” N – Neurological symptoms, F – Fever, R – Renal function impairment, M – Microangiopathic hemolytic anemia, T – Thrombocytopenia • The typical patient is a previously healthy adult presenting with mental status changes, fever, petechiae, fatigue, and pallor. Laboratory tests will then indicate hemolytic anemia and possibly acute kidney injury (AKI). Impaired kidney function may not be present, and only a minority of patients will present with all five clinical findings. Thrombotic thrombocytopenic purpura • TTP patients are typically previously healthy adults. The pentad of clinical findings consists of: • 1.Fever • 2.Neurological signs and symptoms • Altered mental status, delirium • Seizure, focal defects, stroke • Headache, dizziness • 3.Low platelet count (i.e. thrombocytopenia) • Petechiae, purpura • Mucosal bleeding • Prolonged bleeding after minor cuts • 4.Microangiopathic hemolytic anemia • Fatigue, dyspnea, and pallor • Jaundice • 5.Impaired renal function • Hematuria, proteinuria • Oliguria, anuria Thrombotic thrombocytopenic purpura. Diagnostics • Hematology • • • • • ↓ Platelets (< 140,000/μL, usually ∼ 40,000/μL) ↓ Hemoglobin (< 8–9 g/dL, normochromic/normocytic anemia, ↓ hematocrit) ↑ Reticulocytes ↓ Haptoglobin A decrease in haptoglobin is a sign of hemolysis.) Normal or mildly prolonged prothrombin time (PT) and activated partial thromboplastin time (aPTT) • Normal or mildly elevated fibrin degradation products and D-dimer levels • Negative Coombs test (In contrast to autoimmune hemolytic anemia) • Peripheral blood smear • Large number of schistocytes (up to 10% of RBCs) • Low number of platelets Peripheral blood smear Numerous healthy erythrocytes (E) and several fragmented erythrocytes (black dashed circles) with a normal convex side (colored blue) and a fragmented side that is concave or straight (colored red) can be seen. Schistocytes are a diagnostic finding in microangiopathic hemolytic anemias. These cellular fragments can also result from mechanical damage to erythrocytes (e.g., due to prosthetic heart valves). Thrombotic thrombocytopenic purpura. Diagnostics • Serum chemistry • • ↑ LDH, ↑ indirect bilirubin (hemolytic anemia) ↑ BUN and ↑ creatinine (impaired renal function) • Urinalysis • Hematuria, proteinuria • ADAMTS13 activity and inhibitor testing • • ↓ ADAMTS13 activity Not a routinely available test and should be used for confirmation only • Identification of secondary causes (e.g., tests for pregnancy, SLE, HIV, malignancy) • See “Differential diagnosis of platelet disorders.” Thrombotic thrombocytopenic purpura. Treatment • TTP requires urgent diagnosis and treatment! Waiting for test results to confirm ADAMTS13 deficiency should not delay treatment. • Treatment should be started after a presumptive diagnosis is made based on clinical features and initial labs (e.g., blood count, peripheral smear, creatinine). • Monitoring and correction • • • • • • • • Fluid status abnormalities Electrolyte disturbances Acid-base abnormalities RBC transfusions Prompt initiation of plasma exchange therapy (PEX) Glucocorticoids (e.g., prednisone) Rituximab is reserved for severe cases. Caplacizumab • • Humanized bivalent single-domain antibody used in the treatment of acquired or immunemediated thrombotic thrombocytopenic purpura Prevents microvascular thrombosis by inhibiting the interaction of von Willebrand factor and platelets • Platelet transfusion should only be reserved for patients who are bleeding or require an invasive procedure. • Thank you for learning!