Nursing management of a bleeding child with severe Idiopathic
advertisement

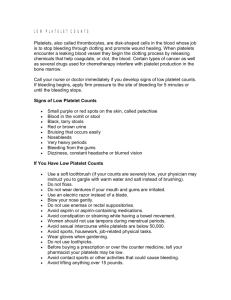
Nursing management of a bleeding child with severe Idiopathic Thrombocytopenia Purpura Primary Author: Beatrice Gundo Reviewed and updated by the Child Nurse Practice Development Initiative, April 2014 Practice guideline only. Please also consult your hospital’s protocols/policies. Severe Idiopathic Thrombocytopenia Purpura1,2,3,4 Definition: Idiopathic Thrombocytopenia Purpura (ITP) is an autoimmune blood disorder characterised by reduction of platelets levels in blood. Normal platelet level is 150-450 x 109/L. In severe ITP the platelet count is below 20x109/L and is life threatening. Etiology: Unknown, hence the name ‘idiopathic’. However, viral infections, such as chicken pox, rubella, mumps and live vaccinations may trigger ITP in children. The highest risk group are children between the ages of 2-5 years. Pathophysiology1,3 Nursing Care Normally, the liver and kidneys produce a glycoprotein hormone called thrombopoeitin. It regulates production of platelets in the bone marrow. The hormone binds to megakaryocytes (large cells in the bone marrow). Megakaryocytes now fragment into small particles called platelets. Platelets are part of blood cells responsible for blood clotting. The normal life span of these platelets is between 3-10 days. The spleen is responsible for destruction of old platelets as well as affected platelets. For unknown reasons, antibodies are triggered to attack either the megakaryocytes cells in the bone marrow or the already produced platelets. The megakaryocytes become immature and less productive. When the platelets are attacked by the antibodies, the spleen recognises them as foreign bodies and destroys them. The destruction of platelets occurs very rapidly, leading to reduced platelet levels. Mother-child interaction: • Explain the condition and treatment to the caregiver to reduce anxiety. She can then reassure the child.3 • Allow the caregiver to be with the child to promote interaction.3 Pain/comfort management: • Assess for pain and manage accordingly.3 • Promote sleep. Nurse child in a comfortable position.1 Nutrition: • Encourage the child to eat dark green leafy vegetables. They promote clotting.1 • Describe and monitor stools for diarrhoea and blood3 Hydration: • Observe and report the amount and location of bleeding episodes3 • Secure IV line for fluids, medication and possibly blood transfusions.3 • Exert pressure on any puncture sites for 5 to 10 minutes3 • Monitor fluid balance by recording input and output daily3 • Describe and monitor urine and vomitus for blood3 • Transfuse blood if there are signs of cardiac failure such as tachypnea4 Prevent infection: • Apply infection prevention measures such as hand washing, linen changes and sterility during procedures3. • Encourage short stay to prevent nosocomial infections1 Maintain skin and mucosal integrity: • Provide primary care such as bathing, frequent nappy changes, mouth care and skin care to promote skin and mucosal integrity1 • Use a soft toothbrush to prevent gum mucosal breakdown3 • Protect area of petechiae from further injuries3 • Promote exercises as tolerated1 Support regulatory system: • Monitor and record vital signs such as temperature, heart rate, respiratory rate and blood pressure 6 hourly and report any deterioration • Observe for signs of respiratory distress and cardiac failure, such as chest recessions, cyanosis and nasal flaring.4 • Maintain patient on strict bed rest during active bleeding episodes3 • Obtain blood samples for haemoglobin levels and platelet count daily3. • Avoid taking drugs like aspirin, because it impairs coagulation3. • Monitor glucose levels daily1. Signs and Symptoms1,2,3 • • • • • • • Petechiae or purpura Ecchymosis (Bruises) Persistent bleeding from cuts Mucosal/Gingival bleeding Frequent or heavy nose bleeding Haematuria Splenomegaly Complications3. • • • • • • Intracranial/ cerebral haemorrhage Bleeding into diaphragm can lead to pulmonary complications. Gastrointestinal bleeding Anaemia Hematomas on nerve or brain tissue can lead to paralysis. Purpural lesions can occur in vital organs such as brain, kidneys and intestinal tract, compromising their functions. • Hypothyroidism or hyperthyroidism, as antibodies attack the thyroid gland. References Treatment • Might not be required, depending on severity • IV immune globulin (IVIG) or Rh immune globulin to prevent further destruction of platelets • Medications (e.g. Eltrombopag/ Romiplostim) to increase platelet count • Surgery to remove spleen, if site of destruction of platelets. 1. Nurses Group of the European for Blood and Marrow transplantation. 2011. Immune Thrombocytopenia: A practical guide for nurses and other Allied health care professionals. Available: www.ebmt.org/contents/resources/library/.../ITP%20Handboo. PD [2013, February, 27] 2. Glasper, E.A., McEwing, G. & Richardson, J. 2007. Oxford book of Children’s &Young People’s Nursing. Oxford University Press. New York. 3. Mills, E.J. 2006. Handbook of Medical-Surgical Nursing. 4th ed. Ambler PA: Lippincott Williams and Wilkins. Available: books.google.co.za/books?/isbn=1582554455 [2013, March, 8] 4. Josephs, T. Personal communication [2013, April, 21] Working with Red Cross War Memorial Children’s Hospital and School of Child and Adolescent Health, University of Cape Town