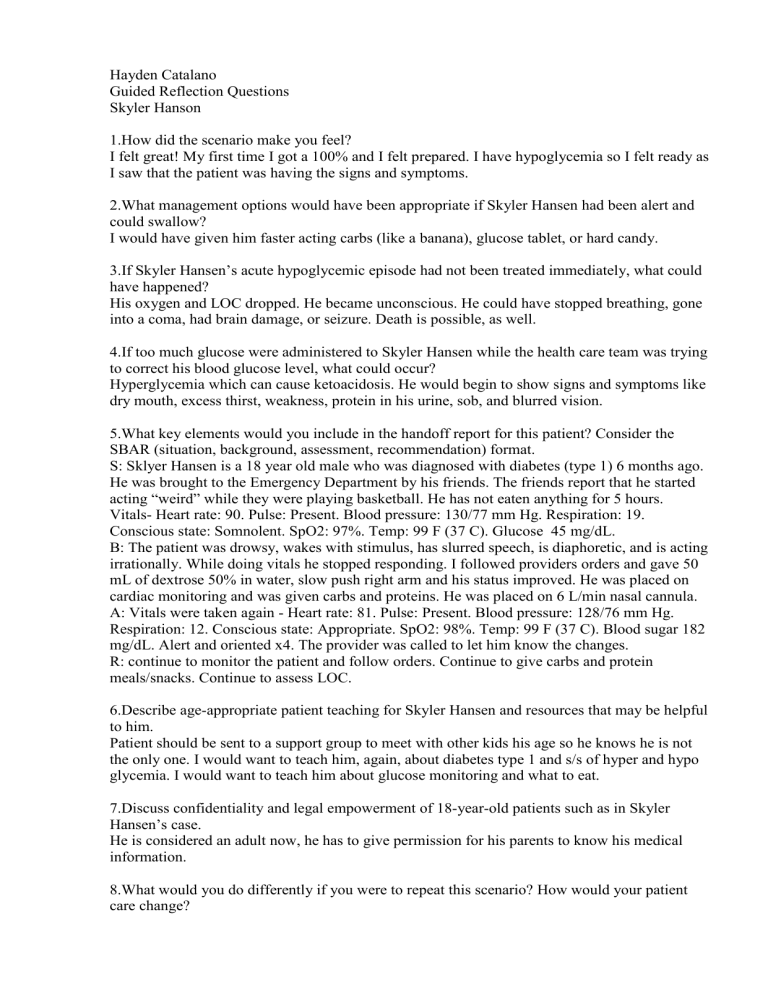
Hayden Catalano Guided Reflection Questions Skyler Hanson 1.How did the scenario make you feel? I felt great! My first time I got a 100% and I felt prepared. I have hypoglycemia so I felt ready as I saw that the patient was having the signs and symptoms. 2.What management options would have been appropriate if Skyler Hansen had been alert and could swallow? I would have given him faster acting carbs (like a banana), glucose tablet, or hard candy. 3.If Skyler Hansen’s acute hypoglycemic episode had not been treated immediately, what could have happened? His oxygen and LOC dropped. He became unconscious. He could have stopped breathing, gone into a coma, had brain damage, or seizure. Death is possible, as well. 4.If too much glucose were administered to Skyler Hansen while the health care team was trying to correct his blood glucose level, what could occur? Hyperglycemia which can cause ketoacidosis. He would begin to show signs and symptoms like dry mouth, excess thirst, weakness, protein in his urine, sob, and blurred vision. 5.What key elements would you include in the handoff report for this patient? Consider the SBAR (situation, background, assessment, recommendation) format. S: Sklyer Hansen is a 18 year old male who was diagnosed with diabetes (type 1) 6 months ago. He was brought to the Emergency Department by his friends. The friends report that he started acting “weird” while they were playing basketball. He has not eaten anything for 5 hours. Vitals- Heart rate: 90. Pulse: Present. Blood pressure: 130/77 mm Hg. Respiration: 19. Conscious state: Somnolent. SpO2: 97%. Temp: 99 F (37 C). Glucose 45 mg/dL. B: The patient was drowsy, wakes with stimulus, has slurred speech, is diaphoretic, and is acting irrationally. While doing vitals he stopped responding. I followed providers orders and gave 50 mL of dextrose 50% in water, slow push right arm and his status improved. He was placed on cardiac monitoring and was given carbs and proteins. He was placed on 6 L/min nasal cannula. A: Vitals were taken again - Heart rate: 81. Pulse: Present. Blood pressure: 128/76 mm Hg. Respiration: 12. Conscious state: Appropriate. SpO2: 98%. Temp: 99 F (37 C). Blood sugar 182 mg/dL. Alert and oriented x4. The provider was called to let him know the changes. R: continue to monitor the patient and follow orders. Continue to give carbs and protein meals/snacks. Continue to assess LOC. 6.Describe age-appropriate patient teaching for Skyler Hansen and resources that may be helpful to him. Patient should be sent to a support group to meet with other kids his age so he knows he is not the only one. I would want to teach him, again, about diabetes type 1 and s/s of hyper and hypo glycemia. I would want to teach him about glucose monitoring and what to eat. 7.Discuss confidentiality and legal empowerment of 18-year-old patients such as in Skyler Hansen’s case. He is considered an adult now, he has to give permission for his parents to know his medical information. 8.What would you do differently if you were to repeat this scenario? How would your patient care change? I would want to ask more questions to the patient to clarify information. I would want to know how he is taking his glucose, if at all, and how often. I would want to know what a typical daily snack and meal regime consists of.