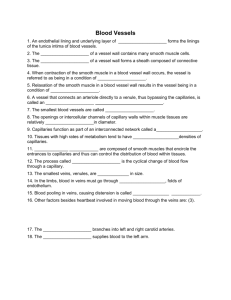
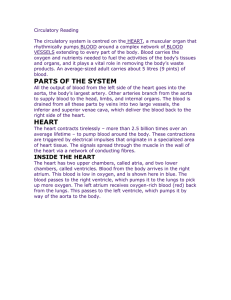
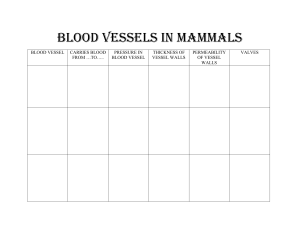
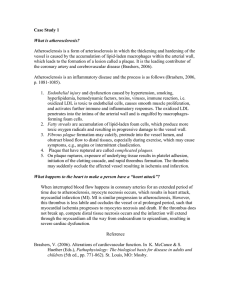
Chapter 15 Alterations of Blood Flow Organization of Circulatory and lymphatic systems Circulatory circuit o Absorption and delivery of nutrients o Oxygen uptake and delivery o Removal of waste products Lymphatic circulation o Specialized system of channels and tissues (nodes) o Collect the excess fluid (2-4 liters/day) that leaks from vascular network into the interstitium and returns it to the general circulation. Interaction of the capillary And lymphatic networks The complete process moving ~5 liters of blood through the entire circuit takes only ~1 minute Anatomy of Arteries and Veins Three microscopically distinct layers (tunicae) Lumen o Intima: endothelial cells in direct contact with the blood as it flows through the vessel • Peridically, the intima layer protrudes into the lumen, creating valves that prevent the backflow of blood o Media: smooth muscle tissue (thickest section in arteries) o Adventitia: collagenous connective tissue (thickest section in veins) Contains elastic tissue Elastic tissue only in large veins Anatomy of Capillaries Single thickness of endothelial cells attached to a basement membrane Diameter decreases as capillaries move from end of arteriole to the beginning of venule Spaces (pores) between endothelial cells determine the capillary permeability o Blood-brain barrier (very tight) o Kidney capillary beds (more porous) Smooth Muscle Principles of flow Known as hemodynamics of the circulatory system • Govern the quantity of blood passing by a given point in a specific period • Measured as a given number of liters, milliliters, per second, minute, or hour • Includes the concepts of • Pressure • Resistance • Velocity • Turbulent flow • Wall tension Blood flow, pressure and resistance Blood flow—movement along a pressure gradient within the vascular bed Pressure—blood moves from areas of higher pressure (arteries) to an area of lower pressure (veins); the greater the pressure difference, the greater the blood flow Resistance—opposing forces that deter blood flow; as resistance increases, blood flow decreases A significant decrease in pressure occurs as blood flows through the arterioles into The capillaries Question 1 Which of the following is the major site of resistance in the vascular system and requires a greater pressure to maintain blood flow? A. B. C. D. Vena cava Venules Arterioles Capillaries Blood Flow, Pressure and Resistance Physical laws govern the flow of blood though vessels Determinants of Resistance 1. Vessel length 2. Vessel radius 3. Blood viscosity Important Laws: oFlow = Pressure/Resistance oBlood pressure = flow (cardiac output) x Resistance oResistance = Pressure/Flow Blood Flow, Pressure and Resistance At a constant pressure gradient: The longer the blood vessel, the higher the resistance and the lower the flow The narrower the blood vessel, the higher the resistance, the lower the flow Velocity and turbulence Velocity and Laminar and Turbulent Flow o Laminar flow: Fastest blood flow in the center of stream Laminar blood flow o Turbulent flow is an interruption in the forward current of blood flow by crosswise flow. Turbulent flow may manifest as o Bruit (audible vascular sound) o Thrill (vibratory sensation on the skin over a turbulent flow) o Thrombus formation (blood clot affecting flow) • Example of pathologic cause of turbulence Turbulent flow generated at a vessel bifurcation Wall tension and compliance Distending pressure (P) is the difference between the pressures on either side of the vessel An increase in radius or distending pressure results in increased wall tension. o If pressure reaches 20 mm Hg, called the critical closing pressure, blood flow ceases entirely. Compliance reflects the distensibility of a blood vessel: veins are highly distendible and are referred to as capacitance vessels. Wall tension (T) = Distending pressure (P) x radius (r) Dynamics in the Microcirculation (Capillaries) Essence of the entire circulatory system Exchange of nutrients and gases takes place Clinically, The capillary fluid pressure and plasma colloid osmotic pressure are most important Capillary fluid pressure is the blood pressure inside the capillary (force that pushes fluid out of vessel) Pathologic conditions resulting in increases in BP or resistance to flow, can alter this force, increasing it and propelling more fluid into the interstitial space, resulting in the formation of edema Question A patient has edema caused by heart failure and hypertension. In this situation, the edema has developed because of A. B. C. D. increased capillary fluid (hydrostatic) pressure. increased plasma colloid osmotic pressure. decreased interstitial fluid colloid osmotic pressure. decreased lymphatic fluid pressure. Control of blood flow By Extrinsic mechanisms All blood vessels except small venules and capillaries contain smooth muscle cells. Arteries have much more smooth muscle than veins Smooth muscle cells are innervated by nerve fibers from the sympathetic nervous system (SNS) Smooth muscle cells have α1 adrenergic receptors that respond to the SNS neurotransmitter, noradrenaline resulting in vasoconstriction Skeletal muscle blood vessels contain β2 adrenergic receptors which respond to epinephrine (adrenaline) resulting in vasodilation Control of blood flow By intrinsic mechanisms Autoregulation is ability of blood vessels within organs to maintain a relatively constant blood flow regardless of changes in arterial pressure o When vascular smooth muscle is stretched, it contracts in response causing vasoconstriction o Endothelial cells also play an important role in vessel dilation and constriction • Produce nitric oxide (NO) gas which causes dilation by relaxing neighboring smooth muscle cells General causes of altered blood flow Obstructions of the vessels Alterations in arterial flow Alterations in venous flow Blood vessel structural alterations Blood vessel obstructions May involve arterial or venous system Obstruction results in reduced flow beyond the obstruction (downstream) and increased pressure before the obstruction (upstream). In the arterial system obstruction manifests as distal ischemia. In the venous system obstruction manifests as edema. Thrombus as a cause of obstruction Thrombus is a stationary blood clot formed within a vessel or a chamber of the heart Etiology: Thrombosis Initiated by alterations in one or more of the following: o Blood flow: slow or turbulent flow o Blood vessel wall: damage or inflammation to the intimal wall of vessel o Blood coagulability: emergence of a hypercoagulable state oCan occur in arteries and veins o Oral contraceptives may increase tendency for thrombosis Thrombus as a cause of obstruction Pathogenesis oArterial thrombosis • Clot within an artery reduces flow and increases turbulence which enhances thrombus enlargement and formation of more thrombi • Decreased distal flow can cause ischemia which can cause Arterial occlusion Myocardial infarction (heart attack) Stroke oVenous thrombosis • Clot in a vein alters venous return impairing the removal of metabolic waste and producing swelling • Inflammation that occurs in a vein is called phlebitis and when it is accompanied with a clot, it is called thrombophlebitis Thrombus as a cause of obstruction Clinical manifestation and treatment oArterial thrombosis o Usually manifested by intermittent claudication (pain with activity) in the affected limb that improves with rest o Limb might be cool and cyanotic (bluish discoloration) o Painful arterial ulcer around one toe oVenous thrombosis o Symptoms may be absent or maybe life-threatening secondary to pulmonary embolism (PE) o Calf or groin tenderness o Swelling of the affected limb Treatment: Surgical or Medical (anticoagulant therapy) Embolus as a cause of obstruction Embolus is a travelling clot that is propelled forward in the bloodstream to a distant point, where it lodges to produce a new site of obstruction Etiology and pathogenesis o Clot usually originates from deep veins of the pelvis and lower extremities (legs) o Go through the right heart and then most commonly lodge in the lung arteries to cause pulmonary embolism (PE) o Clots dislodged from the left side of the heart usually end up in the brain artery and cause “ischemic stroke”. Embolus as a cause of obstruction Clinical Manifestation Pulmonary Embolism (PE) o o o o May be asymptomatic or present vague (non-specific) signs and symptoms Sudden shortness of breath Chest pain Sudden death Stroke: manifestation depends on the area of the brain affected o Loss of cognitive function o Motor changes o Various levels of sensory loss Treatment: Embolectomy; Filter in vena cava Emboli produced by other causes: o Fat aggregates o Metastasizing tumor cells inside the bloodstream forming aggregate o Bacterial emboli o Air bubbles (intravenous catheters) Other causes of vessel obstruction Vasospasm: sudden contraction of arterial smooth muscle Inflammation: intima of the artery and veins Mechanical compression: Trauma, tight casts, stockings Atherosclerosis Means hardening of the arteries Coronary atherosclerosis plague Pathologic origin for the vast majority of arterial disease Ultimately the leading cause of death in U.S and western Europe Develops mostly in large and medium size arteries o Coronary (associated with most mortality; coronary artery disease [CAD]) o Cerebral o Carotid o Femoral o Aorta o Other organs Site of plaque rupture Pathogenesis of atherosclerosis In response to irritation or trauma to the intima, platelets and leukocytes are stimulated These activated cells attach to the endothelial cells 1 Pathogenesis of atherosclerosis Medial smooth muscle cells proliferate and migrate into the intima Cholesterol leaks into the vessel wall Lipids get oxidized by leukocytes and endothelial cells causing more damage 2 Pathogenesis of atherosclerosis A fibrous cap forms over the plaque The lesion slowly grows to decrease the vessel diameter 3 Pathogenesis of atherosclerosis Additional injury may cause rupture of the plaque resulting in thrombus formation and manifestation of acute occlusion Atherosclerotic plaque composed of Smooth muscle cells, lipoproteins and inflammatory debris 4 Atherosclerosis Risk Factors Modifiable Risk Factors o Smoking o Elevated blood pressure o Glucose intolerance o Elevated cholesterol o Decreased physical activity o Ineffective stress management o Depression Nonmodifiable Risk Factors o Age o Gender o Heredity (Family history) Atherosclerosis : Clinical Manifestations and Treatment Disease manifestations vary with the tissues involved and the severity of altered flow Atherosclerosis is an underlying condition for much of o Hypertension o Renal disease o Cardiac disease o Peripheral arterial disease (PAD) Treatment Nonpharmacologic (weight loss, diet, cessation of smoking etc.) Surgical (angioplasty, bypass surgery) Peripheral Artery Diseaese (PAD) Intermittent claudication (Pain with Activity) Less common conditions affecting blood flow Aneurysms Localized arterial dilations, bulge outward Classified as true or false aneurysms True aneurysms include • Saccular: one-sided balloon • Fusiform: both sides balloon out • Berry: balloon has a stem/neck Frequently found in cerebral circulation and thoracic and abdominal aorta Less common conditions affecting blood flow Raynaud Syndrome Extreme vasoconstriction producing cessation of flow to fingers and toes o Color changes: white, blue (cyanosis), red (hyperemia); pain, numbness; cold triggers attacks Intrinsic structural factors, extrinsic neuroregulation, and locally produced mediators involved Treatment: enhancing circulation through relaxation,calciumchannel blockers, sympatholytic drugs, prostaglandins Alterations of Venous Flow Incompetent valves (e.g. in obesity, pregnancy, right heart failure, prolonged standing) producing o Varicose veins • Superficial veins affected o Chronic venous insufficiency • Deep veins affected o Deep vein thrombosis • Could lead to life-threatening pulmonary emboli Accompanied by edema, venous stasis, inflammation, ulcers, and pain Open valves Closed valves Incompetent valve Alterations in Lymphatic Flow Lymphedema Occurs when normal flow is obstructed or altered in some fashion Primary lymphedema results from congenital anomaly or dysfunction of the lymphatic system. Secondary lymphedema associated with a disease process or iatrogenic o Most common worldwide: infection by filarial worms (Wuchereria bancrofti) o Most common in United States because of lymph node removal, radiation Lymphedema associated with mastectomy