Sense Organs Study Material: Receptors, Pain, Taste, Smell, Hearing
advertisement

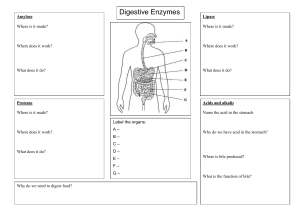
Exam 1 Material *REVIEW CRANIAL NERVES Chapter 16 – Sense Organs Properties of Receptors Receptor – any structure specialized to detect a stimulus (simple nerve ending or complex sense organ) Sensory receptors are transducers converting stimulus energy into electrochemical energy = sensory transduction Information about stimulus that can be conveyed: o Modality or type of stimulus or sensation (vision, hearing, taste) Transduce is o Location of stimuli Each sensory receptor receives input from its receptive field to change Brain identifies site of stimulation = sensory projection Post central gyrus of parietal lobe o Intensity (frequency, numbers of fiber & which fibers – low threshold vs. high) o Duration = change in firing frequency over time Phasic receptor – burst of activity initially & quickly adapt and stop sending signals (smell & hair receptors) i.e. getting used to a bad smell Tonic receptor – adapt slowly, generate impulses continually (proprioceptor) Classification of Receptors By modality: chemoreceptors (receiving signals from chemicals), thermoreceptors (receptors for heat), nociceptors (receptors for pain), mechanoreceptors (stimulate nerves by mechanical ways – like sitting down) and photoreceptors (visual receptors) By origin of stimuli: o Interceptors = detect internal stimuli o Proprioceptors = sense position & movements of body o Exteroceptors = sense stimuli external to body By distribution: o General (somesthetic) sense – widely distributed o Special senses – limited to head (hearing, taste, smell) Unencapsulated Nerve Free nerve endings include o Warm, cold, pain Tactile (Merkel) discs are associated with cells at base epidermis - tonic Hair receptors monitor movement of hairs - phasic Encapsulated Nerve Dendrites wrapped by glial cells or connective tissue, more sensitive o Tactile (Meissner) corpuscles Light touch & texture - phasic o Krause End Bulb Tactile corpuscles in mucous membranes – phasic o Lamellated (Pacinian) corpuscles Deep pressure, stretch, tickle, and vibration – phasic o Ruffini corpuscles Heavy touch, pressure, joint movements & skin stretching – tonic Somesthetic Projection Pathways First-order neuron or afferent neuron o from below head, enter the dorsal horn of spinal cord via spinal nerves o from head, enter pons and medulla from cranial nerve o touch, pressure & proprioception are carried on large, fast, myelinated axons o heat & cold are carried on small, unmyelinated, slow fibers Second-order neuron o decussation (crossing of fibers) of signals to opposite side in spinal cord or medulla o end in thalamus, except for proprioception (cerebellum) Third-order neuron o extend from thalamus to primary somesthetic cortex of cerebrum on contralateral side Pain Found in all tissues except the brain Somatic pain arises from skin, muscles & joints Visceral pain from stretch, chemical irritants or ischemia (lack of blood flow to tissues) of viscera (poorly localized) Referred pain is misinterpreted pain o brain “assumes” pain is coming from skin or superficial sites o heart pain felt in left shoulder or arm (or even the thumb!) because both send pain input to the interneurons of spinal cord segments T1 to T5 CNS Modulation of Pain Intensity of pain is affected by state of mind Endogenous opioids (enkephalins, endorphins, dynorphins) o far more potent that opium, morphine, or heroin o produced by CNS and other organs under stress o found especially in dorsal horn of spinal cord, explaining the spinal gating of pain o act as neuromodulators blocking the transmission of pain Spinal gating stops pain signals at dorsal horn o descending analgesic fibers from reticular formation travel down reticulospinal tract to dorsal horn Cephalgia – secrete inhibitory substances, enkephalins and dynorphins, that block pain headache (head fibers from secreting substance P pain) pain signals never ascend o dorsal horn fibers inhibited by input from mechanoreceptors i.e. rubbing a sore arm reduces pain because you’re inhibiting pain receptors The Chemical Sense – Taste Gustation is the sensation of taste resulting from the action of chemicals on the taste buds Lingual papillae (4 types) o filiform (no taste buds) important for texture o foliate (no taste buds) o fungiform at tip & sides of tongue o vallate (circumvallate) 7-12 at rear of tongue contains 1/2 of taste buds Physiology of Taste To be tasted, molecules must dissolve in saliva 5 primary sensations: salty, sweet, sour, bitter & umami (meaty taste of amino acids such as MSG) o taste is also influenced by food texture, aroma, temperature, and appearance mouthfeel (texture) is detected by lingual nerve branches of Cranial Nerve V in papillae o hot pepper stimulates free nerve endings (pain) Sweet tastes concentrated on tip of tongue, salty & sour on lateral margins of tongue & bitter (alkaloid toxins) at rear o all tastes can be detected throughout the tongue surface o the “bitter” taste can often be from poisonous aspects of plants – defense mechanism Mechanisms of action o sugars, alkaloids & glutamates bind to receptors & activate 2nd messenger systems (i.e. cyclic AMP) o sodium & acids penetrate cells & depolarize them directly Which taste sensation would be most impaired by: o Damage to the facial nerve? Sweet (facial nerve is front 2/3 of tongue o Damage to the glossopharyngeal nerve? Bitter (glossopharyngeal nerve is back 1/3 of the tongue) Taste on the palate, pharynx, and epiglottis is carried by the vagus nerve The Chemical Sense – Smell Receptor cells for olfaction form olfactory mucosa o smell is highly sensitive (more so in women than men) dormitory effect – study done that women who are often close to each other tend to have menstrual cycles sync up due to sense of pheromones 2 Covers 5cm of superior concha & nasal septum Cells of the Olfactory Mucosa and Bulb Olfactory cells 10 to 20 million cells o neurons with 20 cilia called olfactory hairs binding sites for odor molecules in thin layer of mucus, immobile cilia o axons pass through cribriform plate and are known collectively as Cranial Nerve 1? o Olfactory cells survive 60 days o These are the only neurons in body exposed to external environment Basal cells divide & differentiate into new olfactory cells (unusual for neurons) A fracture of which cranial bone cause anosmia? Anosmia is without smell so ethmoid bone Pitch and Loudness Frequency at which party of the ear vibrate gives us sense of pitch (low- or high- pitched sounds) o Hearing range is 20-20,000 Hz (cycles/sec) Human speech tends to fall within 1500-4000 Hz where hearing is most sensitive Loudness if perception of intensity of sound energy Outer Ear Fleshy auricle (pinna) directing air vibrations down auditory canal (external auditory meatus) Middle Ear Air-filled cavity in temporal bone separated from air outside the head by tympanic membrane (tympanum, eardrum) o 1 cm in diameter, slightly concave, freely vibrating membrane Tympanic cavity filled with air by auditory tube (Eustachian tube) connected to nasopharynx o opens during swallowing or yawning to equalize air pressure on both sides of eardrum o offers a path for upper respiratory infections to spread from the throat to the middle ear, resulting in otitis media (inflammation of middle ear) Auditory ossicles span tympanic cavity o malleus attached to eardrum, incus, stapes attached to membranous oval window of inner ear Auditory ossicles concentrate sound waves and conduct them to oval window Inner Ear Passageways in temporal bone = bony labyrinth Fleshy tubes lining bony tunnels = membranous labyrinth o filled with endolymph (similar to intracellular fluid) o floating in perilymph (similar to cerebrospinal fluid) Anatomy of the Cochlea Stereocilia of hair cells embedded in gelatinous tectorial membrane. Hearing comes from inner hair cells -- outer ones adjust cochlear responses to different frequencies increasing precision— not neurons Physiology of Hearing -- Middle Ear Eardrum vibrates quite easily o 18 times the area of the oval window creates enough force/unit area (conducted through auditory ossicles to the stapes’ connection to the oval window) in order to vibrate the endolymph in the scala vestibuli The auditory ossicles do NOT amplify the vibration, they concentrate it Protection of cochlea by muscle contraction in response to loud noises (tympanic reflex) o tensor tympani pulls eardrum inward, tightening it o stapedius reduces mobility of stapes o 40 msec latency o designed for slowly building noises like thunder not gunshots (irreversible damage by breaking stereocilia) does not protect us from sustained loud noises such as music, either o muscles also contract while speaking – so we can hear others Potassium Gates of Cochlear Hair Cells Stereocilia bathed in high K+ concentration (endolymph) creating electrochemical gradient from tip to base Stereocilia of OHCs have tip embedded in tectorial membrane which is anchored to bony core of cochlea called the modiolus Movement of basilar membrane bends the cell’s many stereocilia Bending of taller stereocilia pulls on protein tip links of shorter neighboring ones and opens ion channels K+ flows in -- depolarizing it & causing release of neurotransmitter stimulating sensory dendrites at its base Sensory Coding Loudness produces more vigorous vibrations & excites more hair cells over a larger area o triggers higher frequency of action potentials from a given location on the basilar membrane o brain interprets this as louder Determination of pitch depends on which part of basilar membrane is vibrated at peak amplitude of standing wave o membrane is narrow & stiffer at basal end (collagen) brain interprets signals from IHC at basal end as high-pitched o at distal end is 5 times wider & more flexible brain interprets signals from IHC at distal end as low-pitched Auditory Projection Pathway Cochlear nerve joins vestibular nerve to form vestibulocochlear nerve (cranial nerve #8) Lead to cochlear nuclei in pons and synapse with second-order neurons there or in the inferior colliculus of the midbrain Third-order neurons in the inferior colliculus ascend to the thalamus o Any sensation you are conscious of must go through the thalamus on the way to the cerebral cortex. Fourth-order neurons (unusual for afferent pathways to have 4) finish the pathway to the primary auditory cortex in the temporal lobes Deafness Term encompasses any hearing loss: mild and temporary to complete and irreversible Conduction deafness o due to interference of conduction of vibrations to inner ear o damaged eardrum, otitis media, blockage of auditory canal with cerumen (cerumen), otosclerosis (fusion of ossicles) Sensorineural (nerve) deafness o due to death of hair cells or any nervous element involved in hearing o occupational hazard for musicians, factory and construction workers Equilibrium Control of coordination and balance Receptors in vestibular apparatus o semicircular ducts contain cristae o saccule & utricle contain maculae Static equilibrium is perception of head orientation o perceived by macula Dynamic equilibrium is perception of motion or acceleration o linear acceleration perceived by macula o angular (rotational) acceleration perceived by crista The Saccule and Utricle Saccule & utricle chambers contain maculae o patch of hair cells with their stereocilia & one kinocilium buried in a gelatinous otolithic membrane weighted with granules (calcium carbonate) called otoliths o otoliths add to the density & inertia and enhance the sense of gravity and motion Macula Sacculi and Macula Utriculi With the head erect, stimulation is minimal, but when the head is tilted, weight of membrane bends the stereocilia (static equilibrium) When car begins to move at green light, linear acceleration is detected since heavy otoliths of the utricle lag behind (one type of dynamic equilibrium) (horiz. oriented) When ascending in an elevator, the otoliths of the saccule lag behind. (vert. oriented) Crista Ampullaris of Semicircular Ducts Crista ampullaris consists of hair cells buried in a mound of gelatinous membrane, the cupula (one in each duct) Crista Ampullaris & Head Rotation As head turns, the endolymph lags behind pushing the cupula and stimulating its hair cells The macula and the crista CANNOT detect constant, steady motion—they only detect changes in motion. Why? constant rotation will be very smooth so you can’t tell you’ Equilibrium Projection Pathways Hair cells of macula sacculi, macula utriculi & semicircular ducts synapse on vestibular nerve Vision and Light Vision (sight) is perception of light emitted or reflected from objects in the environment Visible light is electromagnetic radiation with wavelengths from 400 to 750 nm Light must cause a photochemical reaction to produce a nerve signal our brain can notice o radiation with wavelengths below 400 nm (ultraviolet, etc.) has so much energy it kills cells o radiation with wavelengths above 750 nm (infrared, etc.) has too little energy to cause photochemical reaction (it only warms the tissue) Note: shorter wavelength correlates with more energy Eyebrows and Eyelids Eyebrows provide facial expression, protection from glare & perspiration Eyelids (palpebrae) o block foreign objects, help with sleep, blink to moisten o meet at corners (commissures/canthi) o consist of orbicularis oculi muscle & tarsal plate covered with skin outside & conjunctiva inside conjunctiva is transparent mucous membrane that lines the eyelids and covers anterior surface of eyeball except cornea Richly innervated & vascular (heals quickly) Conjunctivitis is pink eye What mechanism involving the conjunctiva would produce a blood-shot eye? vasodilation o tarsal glands secrete oil that reduces tear evaporation o eyelashes help keep debris from the eye Innervation of Extrinsic Eye Muscles Superior oblique muscle – Trochlear Nerve (IV) Lateral rectus muscle – Abducens Nerve (VI) Levator palpebra superioris muscle (elevate eyelid), superior rectus muscle, medial rectus muscle, inferior rectus muscle, inferior oblique muscle – Oculomotor Nerve (III) The Tunics (Layers) of the Eyeball Fibrous layer (tunica fibrosa) = sclera and cornea Vascular layer (tunica vasculosa) = choroid, ciliary body & iris - also called the uvea Internal layer (tunica interna) = retina and optic nerve The Optical Components Series of transparent structures that bend or refract light rays to focus them on the retina o cornea is transparent covering of anterior surface of eyeball (which does most of the refracting!) Detached retina o aqueous humor is clear serous fluid filling area in front of lens (between lens and is when the cornea) retina pulls away o lens is suspended by ring of suspensory ligaments capable of changing shape to help focus light rays Glaucoma is more rounded when no tension on it (ciliary muscle contracted, increased intraocular near vision) pressure- smashes somewhat flattened normally due to pull of suspensory ligaments retina against (ciliary muscle relaxed, far vision) eyeball and can lead o vitreous humor (vitreous body) is jelly filling the space between the lens and to blindness retina Aqueous Humor Serous fluid produced by ciliary body flows from posterior chamber through pupil to anterior chamber -- reabsorbed into canal of Schlemm (scleral venous sinus) The Neural Components Neural apparatus includes the retina & optic nerve Retina forms as an outgrowth of the diencephalon o attached only at optic disc where optic nerve begins and at ora serrata (its anterior margin) Retina is actually part of the brain. Only part seen without dissection. o pressed against rear of eyeball by vitreous body Detached retina o blow to head or lack of sufficient vitreous body o blurry areas in field of vision o leads to blindness if uncorrected due to disruption of blood supply Ophthalmoscopic Examination of Eye Cells on visual axis of eye = macula lutea (3 mm area) o fovea centralis is the center of macula where most finely detailed images are seen Lutea - yellow due to packed receptor cells Eye exam provides direct evaluation of blood vessels Test for Blind Spot Optic disk or blind spot is where optic nerve exits the posterior surface of the eyeball o no receptor cells are found in optic disk Blind spot can be seen using the above illustration o with right eye closed, stare at X and move toward screen until red dot disappears Visual filling is the brain filling in the green bar across the blind spot area (better than a hole in visual field) Formation of an Image Light must pass through the lens to form tiny inverted (upside down) image on retina Pupillary constrictor is smooth muscle cells encircling the pupil know the difference o parasympathetic stimulation narrows the pupil between constrictor and dilator Pupillary dilator is spokelike myoepithelial cells o sympathetic stimulation widens the pupil to admit more light Remember this using fight-or-flight mnemonic Active when light intensity changes (photopupillary reflex) or when shift gaze from distant object to nearby object (to decrease spherical aberration due to refraction) o both pupils constrict if one eye is illuminated (consensual light reflex) Refraction Bending of light rays occurs when light passes through substance with different refractive index at any angle other than 90 degrees o refractive index of air is arbitrarily set to n = 1 o refractive index of cornea is n = 1.38 o refractive index of lens is n = 1.40 Cornea refracts light more than lens does o lens fine-tunes the image as shift focus between near and distant objects The Near Response Emmetropia = eyes focused on distant object (more than 6 m away) receive parallel light waves & focus without effort Near response occurs if focus on object closer (light waves are NOT parallel and must be bent/refracted more to compensate) o convergence of eyes eyes orient their visual axis toward the object o constriction of pupil (pupillary miosis) does not admit peripheral light rays & reduces spherical aberration (blurry edges) o accommodation of lens contraction of ciliary muscle relaxes suspensory ligaments which allows lens to relax to a more convex shape light is refracted more strongly & focused onto retina Hyperopia and Myopia Hyperopia is farsightedness (eye is too short front to back) o eyeball is too short, focused image would fall behind the retina o CAN see far objects because the ciliary muscle contracts to fatten the lens and bend the parallel rays enough to make the image fall on the retina. A normal eye’s ciliary muscle does not have to do this. Convex lens – fat in the middle skinny on the edges Concave lens – thin in the middle thicker on the edges o Close objects can’t be focused because the lens is as fat as it can get and it’s still not enough to force the focused image onto the retina o correct with convex lens which helps bend the light waves before they reach the eye so the image falls on the retina properly Myopia is nearsightedness (eye is too long front to back) o eyeball is too long, focused image would fall in front of retina o CAN see near objects (even nearer than a normal eye) because the ciliary muscle doesn’t have to work as much to refract the light waves by fattening the lens. (A -opia means eye thinner lens than normal can get the image onto the retina.) o Far objects are a problem to see because the lens is as thin as it can get and the light waves are still being bent too much. (Remember: the cornea cannot be adjusted to stop bending light waves.) The focused image falls in front of the retina and starts to diverge again before it reaches the retina, producing a blurry image. o correct with concave lens which diverges the light waves before they reach the eye to compensate for the “excessive” refracting produced by the cornea. Effects of Corrective Lenses Presbyopia = “old eyes” o Old lens can’t see near objects due to increasing stiffness of the lens. Corrected with bifocals. Astigmatism (cornea is funny shaped) o Warped cornea makes focusing all parts of the image difficult. Corrected with cylindrical lenses. Retinal Cells Posterior layer of retina is pigment epithelium o purpose is to absorb stray light & prevent reflections o unlike tapetum lucidum of cow eyeball which Acts like a mirror to improve night vision Photoreceptors cells are next layer o derived from stem cells that produced ependymal cells Rod cells (night vision) o outer segment is stack of coinlike membranous discs studded with rhodopsin pigment molecules Cone cells (color vision in bright light) o outer segment tapers to a point Notice that light must travel through a bunch of neurons before ever reaching the photoreceptors! Nonreceptor Retinal Cells Bipolar cells (1st order neurons) Moiety - portion of a molecule that o synapse on ganglion cells refers to a certain part/portion. o large amount of convergence Ganglion cells (2nd order neurons) o axons of these form optic nerve o more convergence occurs (114 receptors to one optic nerve fiber) A lot of processing done before even leaving the eye! Horizontal & amacrine (anaxonic neurons) cells form connections between other cells Thalamus is where 3rd order neurons are found (later geniculate nuclei specifically) o enhance perception of contrast, edges of objects & changes in light intensity Visual Pigments Visual pigment of the rod cells is called rhodopsin (visual purple) 2 major parts to the molecule o protein called opsin o vitamin A derivative called retinal Rod cells contain single kind of rhodopsin with an absorption peak at wavelength of 500 nm Cones contain photopsin (iodopsin) o opsin moieties contain different amino acids that determine which wavelengths of light are absorbed o 3 kinds of cones (red, green, blue) absorbing different wavelengths of light produce color vision The Photochemical Reaction in Rod Cells When rhodopsin absorbs light, it is converted from the bent shape (cis-retinal) [crooked = cis] to the straight (trans-retinal) which then dissociates from the opsin (bleaching) Takes 5 minutes to regenerate 50% of rhodopsin o trans-retinal converted back to cis-form in the pigment epithelium & then returned to the rod to be reunited with opsin there Light and Dark Adaptation Light adaptation (wake up in middle of night and turn on bright light) o pupil constriction and pain from over stimulated retinas o color vision & acuity not optimal for 5 to 10 minutes Dark adaptation (sitting in a bright room at night and power failure occurs) o dilation of pupils occurs o 20 to 30 minutes required for bleached rhodopsin to return to maximal possible sensitivity in the dark Scotopic System (Night Vision) Sensitivity of rods in dim light o extensive neuronal convergence o 600 rods converge on 1 bipolar cell o many bipolar cells converge on each ganglion cell o high degree of spatial summation (very weak light can stimulate ganglion cell) but no ability to resolve detail one ganglion cell receives information from huge 1 mm2 of retina producing only a coarse image Edges of retina with widely spaced receptor cells is low-resolution system only alerting us to motion Photopic System (Day Vision) Fovea contains only 4000 tiny cone cells and no rods o no neuronal convergence o each foveal cone cell has “private line to the brain” Color Vision Primates have well developed color vision o nocturnal vertebrates have only rods Cones are named for absorption peaks of photopsins o blue cones peak sensitivity at 420 nm o green cones peak at 531 nm o red cones peak at 558 nm (orange-yellow) Perception of color is based on mixture of nerve signals Color blindness is hereditary lack of one photopsin o red-green is common (lack either red or green cones) incapable of distinguishing red from green sex-linked recessive (8% of males, 0.5% of females) Stereoscopic Vision (Stereopsis) Depth perception is the ability to judge how far away objects are Requires 2 eyes with overlapping visual fields o panoramic vision has eyes on sides of head (horse) Fixation point is spot on which eyes are focused o objects farther away require image focus medial to the fovea o objects closer result in image focus lateral to fovea o the location of the image of an unfocused object on the retina relative to the fovea tells the brain if it is nearer or farther away than the object that the eye is focused on Visual Projection Pathway KNOW THE PATHWAY DIAGRAM FOR THE EXAM! Bipolar & ganglion cells in retina are 1st & 2nd order neurons (axons of ganglion cells form CN II) Hemidecussation occurs in optic chiasm o 1/2 of fibers decussate so that images of all objects in the left visual field (which fall on right half of each retina) go to the right visual cortex o each side of brain sees what is on the side where it has motor control over limbs 3rd order neurons in lateral geniculate nucleus of thalamus form optic radiation to 1 visual cortex in the occipital lobe where conscious visual sensation occurs Hemianopsia – “half no o Few fibers project to superior colliculi & midbrain for visual reflexes sees” (photopupillary & accommodation) Visual Information Processing Decussation – to cross Some processing occurs in the retina o adjustments for contrast, brightness, motion & stereopsis Primary visual cortex is in the occipital lobe Visual association areas in parietal & temporal lobes process visual data o object location, motion, color, shape, boundaries o store visual memories (recognize printed words) Read about the history of anesthesia in Clinical Insight 16.5 Chapter 25 – Digestive System Digestive Functions Ingestion = intake of food Digestion = breakdown of molecules Absorption = uptake nutrients into blood/lymph Defecation = elimination of undigested material Stages of Digestion Mechanical digestion is physical breakdown of food into smaller particles o teeth & churning action of stomach & intestines Chemical digestion is series of hydrolysis reactions that break macromolecules into their monomers The process of hydrolysis requires the use of what molecule? Water o enzymes from saliva, stomach, pancreas & intestines results o polysaccharides into monosaccharides o proteins into amino acids o fats into glycerol and fatty acids Digestive Processes Motility = muscular contractions that break up food, mix it with enzymes & move it along Secretion = digestive enzymes & hormones will be secreted to coordinate the actions of digestive system Membrane transport = absorption of nutrients Subdivisions of the Digestive System Digestive tract (alimentary canal) o 30-foot-long tube extending from mouth to anus o gastrointestinal (GI) tract includes only the stomach and intestines Accessory organs o teeth, tongue, liver, gallbladder, pancreas, salivary glands Material inside the digestive tract us not considered to be inside the body. Why? You have to absorb it into the wall of the GI tract for body to properly absorb the material. Tissue Layers of the GI Tract Mucosa (actually touches the food) o epithelium - next to lumen (center opening of tube) o lamina propria - connective tissue o muscularis mucosae - thin layer of smooth muscle Submucosa- blood/lymph vessels, nerve plexus Muscularis externa o inner circular layer o nerve plexus between o outer longitudinal layer Serosa or Adventitia o serosa is areolar CT topped by mesothelium found from the infradiaphragmatic esophagus through the sigmoid colon o adventitia is fibrous CT found elsewhere on digestive tract (oral cavity, pharynx, portion of the esophagus above the diaphragm, and the rectum) Enteric usually refers to the intestines Enteric Nervous Control Enteric nervous system – esophagus, stomach, and intestines have their own nervous network: o controls motility & secretion in response to stimuli to the mucosa o part of the parasympathetic nervous system o Two subdivisions: submucosal (Meissner) plexus located between submucosa and inner layer of muscularis externa controls glandular secretions and movements of muscularis mucosae myenteric (Auerbach) plexus located between the inner and outer layers of the muscularis Peristalsis – movement externa in the tube controls peristalsis and other movements of muscularis externa -ante in this Relationship to the Peritoneum case means Most of the gastrointestinal tract is anteperitoneal (within the peritoneal sac) o Only duodenum, pancreas, & parts of large intestine are retroperitoneal inside, usually Dorsal mesentery suspends GI tract & forms serosa (visceral peritoneum) of stomach & means in intestines front of Ventral mesentery forms lesser omentum & greater omentum o greater omentum hangs like an apron over the viscera lacy layer of connective tissue contains lymph nodes, lymphatic vessels and blood vessels lesser omentum runs from lesser curvature of stomach to liver and may also be called the gastrohepatic ligament (gastro - stomach; hepatic - liver) the omenta adhere to perforations or inflamed areas of stomach or intestines, contribute immune cells to the site, and isolate infections that might otherwise cause peritonitis Mesentery and Mesocolon Mesentery of small intestines holds many blood vessels Mesocolon anchors the colon to the posterior body wall Regulation of Digestive Tract Neural control o short myenteric reflexes (i.e., swallowing) act through myenteric nerve plexus to stimulate nearby areas of muscularis externa reflex arc travels a short distance o long vagovagal reflexes parasympathetic stimulation of digestive motility and secretion by autonomic nerve fibers of the vagus nerves impulses travels from gut to head and back to gut (a long distance) Hormones like gastrin and secretin o long-range chemical messenger molecules that diffuse into the bloodstream and stimulate distant target cells Paracrine secretions o short-range chemical messenger molecules that diffuse through extracellular tissue fluid (NOT the bloodstream) to nearby target cells o histamine and prostaglandins stimulate digestive function Features of the Oral Cavity Cheeks and lips keep food between teeth for chewing, are essential for speech & suckling in infants o vestibule is space between teeth & cheeks o cutaneous area versus red or vermilion area Tongue is sensitive, muscular manipulator of food o papillae & taste buds on dorsal surface o lingual glands secrete saliva, tonsils in root How does the tongue avoid being bitten? Proprioception Hard & soft palate o allow breathing & chewing at same time o palatoglossal (anterior) & palatopharyngeal (posterior) arches palatine tonsils found in space between known as fauces Friction ridges (palatal rugae) of the hard palate help the tongue in manipulating food Teeth The teeth are collectively called the dentition. The meeting of the teeth when the mouth closes is called occlusion. (Poor meeting = malocclusion) Types of teeth: o 8 incisors chisel-like for cutting and biting off pieces of food o 4 canines pointed for puncturing and shredding (reduced in humans) o 8 premolars 2 cusps (bumps) each, so also called bicuspids Broad occlusal surfaces for grinding and crushing. Not present in children. o 12 molars 4-5 cusps each, for grinding and crushing Only 8 in children. Third molars may not erupt in small-jawed adults, becoming impacted. Permanent & Baby Teeth Baby (deciduous) teeth (20) erupt by 2 years of age; Adult teeth (32) erupt between 6 and 25 Deciduous – they fall out Tooth Structure Periodontal ligament is modified periosteum (covering on outside of bone made of Dense Irr. CT) o anchors into alveolus Cementum & dentin are living tissue Enamel is noncellular secretion formed during development Root canal leads into pulp cavity o nerves & blood vessels Gingiva or gums o Gingivitis – inflammation of gums Mastication or Chewing Breaks food into smaller pieces to be swallowed o surface area exposed to digestive enzymes Contact of food with sensory receptors triggers chewing reflex o tongue, buccinator & orbicularis oris manipulate food o muscles of mastication move the mandible Saliva Functions of saliva o moisten, begin starch & fat digestion, cleanse teeth, inhibit bacteria, bind food together into bolus pH of 6.8 to 7.0 (neutral) Hypotonic – less solutes in it Hypotonic solutions of 99.5% water and solutes: than in the blood o salivary amylase = begins starch digestion immediately pH optimum of 7 (neutral pH) Salivary amylase – made of o lingual lipase = digests fat after reaches the stomach pH of 2 in stomach is optimal for lingual lipase activity protein; enzyme o mucus = aids in swallowing o lysozyme = enzyme that kills bacteria o immunoglobulin A = inhibits bacterial growth o electrolytes = Na+, K+, Cl-, phosphate & bicarbonate Salivary Glands Small intrinsic glands found under mucous membrane of mouth, lips, cheeks and tongue - secrete at constant rate 3 pairs extrinsic glands connected to oral cavity by ducts parotid, submandibular and sublingual Histology of Salivary Glands Compound tubuloacinar glands Mucous cells secrete mucus Serous cells secrete thin fluid rich in amylase Mixed acinus is possible What does “acinus” mean? Berry “Demilune”? Half moon, technically Salivation Total of 1 to 1.5 L of saliva per day Cells filter water from blood & add other substances Food stimulates receptors that signal salivatory nuclei in the medulla & pons via C.N.s CN 7,9, & 10 VII & IX carry taste o parasympathetic stimulation salivary glands produce thin saliva, rich in enzymes CN 3,7,9, & 10 o sympathetic stimulation produce less abundant, thicker saliva, with more carry mucus parasympathetic Higher brain centers stimulate salivatory nuclei so sight, smell & thought of food cause fibers salivation Pharynx Skeletal muscle o deep, inner layer – longitudinal orientation o superficial, outer layer – circular orientation circular muscle divided into superior, middle and inferior pharyngeal constrictors Inferior pharyngeal constrictor remains constricted when food is not being swallowed to exclude air from the esophagus. Note that the muscular layers of the pharynx are “backwards” from the normal orientation (circular inner, longitudinal outer) The Esophagus Straight muscular tube 25-30 cm long o nonkeratinized stratified squamous epithelium o esophageal glands in submucosa Extends from pharynx to cardiac stomach passing through esophageal hiatus in the diaphragm Lower esophageal sphincter closes cardiac orifice to prevent gastroesophageal reflux (GERD, “heartburn”) Superior one-third is skeletal muscle, middle one-third is mixture of skeletal and smooth muscle, and lower one-third is smooth muscle Barrett’s o corresponds to shift from voluntary to involuntary control esophagus – Swallowing or Deglutition severe GERD Series of muscular contractions coordinated by swallowing center in medulla & pons o motor signals from cranial nerves V, VII, IX and XII Buccal phase o tongue collects food & pushes it back into oropharynx Pharyngeal-esophageal phase o root of tongue blocks oral cavity o soft palate rises & blocks nasopharynx o infrahyoid muscles lift larynx & epiglottis is folded back o pharyngeal constrictors push bolus down esophagus called peristalsis— sequential pushing of food material through alimentary canal liquids reach stomach in 2 seconds -- food bolus may take 8 seconds lower esophageal sphincter relaxes can swallow even if standing on your head! Introduction to the Stomach Mechanically breaks up food particles, liquefies the food & begins chemical digestion of protein & fat o resulting soupy mixture is called chyme Stomach does not absorb any significant amount of nutrients o does absorb aspirin & some lipid-soluble drugs Gross Anatomy of the Stomach Muscular sac (internal volume from 50ml to 4L, FULL) o J-shaped organ with lesser & greater curvatures o regional differences cardiac region just inside cardiac orifice fundus is domed portion superior to esophageal opening ‘fundus is fun – you burp out of it’ body is main portion of organ pyloric region is narrow inferior end (like a funnel) 2 parts: antrum & pyloric canal Pylorus is opening to duodenum o thick ring of smooth muscle forms a pyloric sphincter Innervation and Circulation Innervation by parasympathetic fibers from vagus & sympathetic fibers from the celiac plexus All blood drained from stomach is filtered through the liver (hepatic portal circulation) before returning to heart Unique Features of Stomach Wall Mucosa o simple columnar glandular epithelium o lamina propria is filled with tubular glands (gastric pits) Muscularis externa has 3 layers o outer longitudinal, middle circular & inner oblique layers Cells of the Gastric Glands and Their Secretions Mucous cells secrete mucus Regenerative cells divide rapidly to produce new cells that migrate upwards towards surface Chief cells secrete pepsinogen throughout life o Pepsinogen is a zymogen (inactive enzyme precursor) HCl converts it to pepsin (active form, digests protein) pepsin then activates more pepsinogen by “digesting” it to form more active pepsin (autocatalytic effect—positive feedback loop – self-speeding up) During infancy only, chief cells also secrete chymosin (curdles milk by coagulating its proteins) & lipase (digests butterfat in milk) Cells of the Gastric Glands and Their Secretions Parietal cells secrete HCl acid & intrinsic factor o Parietal cells also secrete a hunger-producing hormone called ghrelin o HCl activates pepsinogen to pepsin o Intrinsic factor is needed to absorb Vitamin B12 (cobalamin) Vitamin B12 is required for hemoglobin synthesis Deficiency of Vitamin B12 results in what disease? Pernicious Anemia – can’t produce hemoglobin Enteroendocrine cells secrete hormones & paracrine messengers Gastric Acid Secretions 2 to 3 L of gastric juice/day (H2O, HCl & pepsin) Parietal cells contain carbonic anhydrase (CAH) o CO2 + H2O H2CO3 HCO3- + H+ o H+ is pumped into stomach lumen by H+-K+ATPase (active transport) antiporter uses ATP to pump H+ out & K+ in o HCO3- exchanged for Cl- (chloride shift) Cl- pumped out to join H+ forming HCl HCO3- in blood causes alkaline tide (blood pH ) when food is being digested Functions of Hydrochloric Acid Lingual lipase – secreted in Activates enzymes pepsin & lingual lipase mouth, breaks up fats Breaks up connective tissues & plant cell walls o liquefying food to form chyme Chemical digestion in mouth and stomach Converts ingested ferric ions (Fe+3) to ferrous ions (Fe+2) that can be absorbed & utilized for hemoglobin synthesis Destroys ingested bacteria & pathogens Oligo – few Enzymes versus Hormones Enzymes are released by glandular cells into the lumen of the alimentary canal to work on the food particles there. o Examples include: pepsin(ogen) -ogen means inactive precursor Chymosin lipase amylase (salivary or pancreatic) carboxypeptidase watch for the ending -ase Trypsin Chymotrypsin Hormones are released by enteroendocrine cells into the bloodstream to tell other cells elsewhere what to do. o Examples include: gastrin ghrelin cholecystokinin (CCK) vasoactive intestinal peptide (VIP) gastric inhibitory peptide secretin Gastric Motility Swallowing center signals stomach to relax Arriving food stretches the stomach activating a receptive-relaxation response o resists stretching briefly, but relaxes to hold more food Rhythm of peristalsis controlled by pacemaker cells in longitudinal muscle layer o gentle ripple of contraction every 20 seconds churns & mixes food with gastric juice o stronger as reaches pyloric region squirting out 3 mL duodenum neutralizes acids and digests nutrients little at time typical meal is emptied from stomach in 4 hours Vomiting (Emesis) Induced by excessive stretching of stomach, psychological stimuli or chemical irritants (bacterial toxins) Emetic center in medulla causes lower esophageal sphincter to relax as diaphragm & abdominal muscles contract Retching involves thoracic expansion and abdominal contractions to dilate esophagus o lower esophageal sphincter (located at opening into the cardiac stomach) relaxes as stomach and duodenum contract spasmodically o pushes chyme up esophagus o upper esophageal sphincter (located posterior to larynx) remains contracted, preventing ejection of chyme Vomiting occurs when upper esophageal sphincter opens o esophagus and body of stomach relax o chyme driven out by strong abdominal contraction and reverse peristalsis of gastric antrum and duodenum o may even expel some contents of small intestine Protection of Stomach and Peptic Ulcer Three mechanisms to protect stomach tissue from digesting itself: o mucous coat: thick, highly alkaline mucus o epithelial cell replacement: cells live only 3-6 days and are then replaced by regenerative cells in gastric pits o tight junctions: stop HCl from trickling between epithelial cells to digest lamina propria underneath Peptic ulcer is erosion of the gastric wall accompanied by gastritis (stomach inflammation) o Caused by psychological stress? NO! o Caused by excess acid secretion? NO! Used to prescribe cimetidine (Tagamet) to block histamine from binding to and stimulating H2 receptors on parietal cells, but this doesn’t treat the real cause… o Helicobacter pylori! (A bacterial infection!) Antibiotics have a much better cure rate (90% versus 20%-30%) in less time and at lower cost than cimetidine. Regulation of Gastric Function Cephalic Phase (Cephalic refers to “towards the brain”) o vagus nerve stimulates gastric secretion & motility just with sight, smell, taste or thought of food Gastric phase o activated by presence of food or semidigested protein by stretch or in pH o secretion is stimulated by ACh (from parasympathetic fibers), histamine (from gastric enteroendocrine cells) and gastrin (from pyloric G cells) receptors for all 3 substances on parietal cells receptors for ACh and gastrin (not histamine) on chief cells As dietary protein is digested, smaller peptides and amino acids stimulate G cells to produce more gastrin (+ feedback). amino acids and peptides buffer pH so it does not fall too low but when chyme leaves stomach, peptides also leave, so pH drops below 2.0 low pH inhibits parietal and G cells (- feedback) which winds down gastric phase Intestinal phase - duodenum regulates gastric activity through hormones & nervous reflexes o at first gastric activity increases (if duodenum is stretched or amino acids in chyme cause gastrin release) o enterogastric reflex = duodenum inhibiting stomach caused by acid and semidigested fats in duodenum inhibition of vagal nuclei, stimulation of sympathetic neurons which inhibit action of stomach. Like saying, “Stop! Wait until I finish with what you just gave me!” o chyme stimulates duodenal enteroendocrine cells to release secretin, cholecystokinin (CCK) & gastric inhibitory peptide all 3 suppress gastric secretion & motility to give the duodenum time to work on the chyme it already has in it Look at Figure 25.18 in your text book. Liver, Gallbladder and Pancreas All release important secretions into small intestine to continue digestion Gross Anatomy of Liver 3 lb. organ (body’s largest gland) located inferior to the diaphragm 4 lobes -- right, left, quadrate & caudate o falciform ligament separates left and right o round ligament (aka ligamentum teres) is remnant of umbilical vein Gallbladder adheres to inferior surface between right and quadrate lobes Inferior Surface of Liver Porta hepatis is irregular opening between quadrate and caudate lobes containing hepatic portal vein, proper hepatic artery, and bile passages. Porta Hepatis – liver door Microscopic Anatomy of Liver Tiny cylinders called hepatic lobules (2mm by 1mm) Central vein surrounded by sheets of hepatocyte cells separated by sinusoids lined with fenestrated epithelium Blood filtered by hepatocytes on way to central vein o Liver removes nutrients including glucose, amino acids, iron, & vitamins from blood. o Also removes and degrades hormones, toxins, bile pigments, drugs, bacteria & debris o Secretes albumin, lipoproteins, clotting factors, angiotensinogen, etc. into blood Histology of Liver -- Hepatic Triad 3 structures found in corner between lobules o hepatic portal vein and hepatic artery bring blood to the liver provide nutrient-laden, oxygen-poor blood & oxygen-rich blood, respectively o bile ductules collect bile from bile canaliculi between sheets of hepatocytes to be secreted from liver via right and left hepatic ducts Ducts of Gallbladder, Liver & Pancreas Bile passes from bile canaliculi between cells to bile ductules to right & left hepatic ducts Right & left ducts join outside the liver to form common hepatic duct Cystic duct from gallbladder joins common hepatic duct to form the bile duct Pancreatic duct and bile duct combine to form hepatopancreatic ampulla emptying into the duodenum at the major duodenal papilla o sphincter of Oddi (hepatopancreatic sphincter) regulates release of bile & pancreatic juice Cholecystectomy – removal of your gallbladder Gallbladder and Bile Gallbladder is a sac on underside of liver -- 10 cm long 500 to 1000 mL bile are secreted daily from liver Gallbladder stores & concentrates bile o bile backs up into gallbladder from a filled bile duct o between meals, bile is concentrated by factor of 20 Yellow-green fluid containing minerals, bile acids, cholesterol, bile pigments & phospholipids o bile acid (salts) emulsify fats & aid in their digestion enterohepatic circulation - recycling of bile salts (80%) from ileum cholesterol used to synthesize more bile acids to replace the 20% of those secreted that are lost in feces this is the only way the body eliminates excess cholesterol (in the bile) What effect would a drug that blocks bile acid reabsorption have and why? Excretion of bile acids which would lower your cholesterol o all other components of bile are destined for excretion bilirubin pigment from hemoglobin breakdown intestinal bacteria convert to urobilinogen = brown color Gross Anatomy of Pancreas Retroperitoneal gland posterior to stomach o head, body and tail Endocrine and exocrine gland o secretes insulin & glucagon into the blood o secretes 1500 mL pancreatic juice into duodenum water, enzymes, zymogens, and sodium bicarbonate other pancreatic enzymes are activated by exposure to bile and ions in the intestine Pancreatic duct runs length of gland to open at sphincter of Oddi (pancreatic juice mixes with bile) o accessory duct opens independently on duodenum o Why would pancreatic juice need to contain sodium bicarbonate? It helps to neutralize the acid; from the pH of 2 to 8 or 9 Pancreatic Acinar Cells Zymogens = proteases o Trypsinogen (Enterokinase converts this to trypsin which converts the following:) o chymotrypsinogen o procarboxypeptidase Other enzymes (not zymogens) o pancreatic amylase – What molecule does it break down? Starch o pancreatic lipase o ribonuclease and deoxyribonuclease o These are activated when exposed to bile and ions in intestinal lumen. Hormonal Control of Secretion Cholecystokinin released from duodenum in response to arrival of acid and fat which causes: o contraction of gallbladder o secretion of pancreatic enzymes o relaxation of hepatopancreatic sphincter The ultimate goal being… getting it into the duodenum Secretin released from duodenum in response to acidic chyme o stimulates all ducts to secrete more bicarbonate ion Gastrin from stomach & duodenum weakly stimulates gallbladder contraction & pancreatic enzyme secretion Small Intestine Much of the body’s chemical digestion occurs in the small intestine. Also the mouth and stomach. Practically all of the body’s nutrient absorption occurs in the small intestine. Gross Anatomy of Small Intestine Duodenum curves around head of pancreas (10 in.) o retroperitoneal along with pancreas o receives stomach contents, pancreatic juice & bile o neutralizes stomach acids, emulsifies fats, pepsin inactivated by pH increase, pancreatic enzymes Pepsin works at a pH of 2 Jejunum is next 8 ft. (in upper abdomen) o covered with serosa and suspended by mesentery Ileum is last 12 ft. (in lower abdomen) o covered with serosa and suspended by mesentery o ends at ileocecal junction with large intestine Large Surface Area of Small Intestine Circular folds (plicae circularis) up to 10 mm tall o involve only mucosa and submucosa o chyme flows in spiral path causing more contact Villi are fingerlike projections 1 mm tall o contain blood vessels & lymphatics (lacteal) nutrient absorption fat absorption by lacteals Microvilli 1 micron tall o brush border on cells o brush border enzymes are integral proteins embedded in the cells’ plasma membranes for contact digestion -- final stages of digestion, necessitates spiral path Intestinal Cryptus Pores opening between villi lead to intestinal crypts o absorptive cells, goblet cells & at base, rapidly dividing cells life span of 3-6 days as migrate up to surface, then sloughed off & digested o paneth cells – antibacterial secretions Brunner’s glands (in duodenum’s submucosa) secrete bicarbonate mucus Goblet cells make mucus Peyer patches (in ileum) are populations of lymphocytes (WBC) to fight pathogens Secrete 1-2 L of intestinal juice/day o water & mucus, pH 7.4-7.8 Intestinal Motility Mixes chyme with intestinal juice, bile & pancreatic juice Churns chyme to increase contact with mucosa for absorption & digestion Moves residue toward large intestine o Segmentation (kneading the materials inside the tube/mixing it in place) random ringlike constrictions mix & churn contents 12 times per minute in duodenum o Peristaltic waves begin in duodenum but each one moves further down (termed a migrating motor complex) push remaining undigested residue along for 2 hours toward cecum refilling of stomach at the next meal suppresses peristalsis and reactivates segmentation Food in stomach also causes gastroileal reflex (relaxing of ileocecal valve & filling of cecum) Segmentation in the Small Intestine Purpose of segmentation is to mix & churn not to move material along as in peristalsis Peristalsis Gradual movement of contents towards the colon Begins after absorption occurs Migrating motor complex controls waves of contraction o second wave begins distal to where first wave began Carbohydrate Digestion in Small Intestine Salivary amylase stops working in acidic stomach (if < 4.5) o 50% of dietary starch digested before it reaches small intestine Pancreatic amylase completes first step in 10 minutes (at pH of 8) Brush border enzymes act upon oligosaccharides, maltose, sucrose, lactose & fructose o dextrinase, glucoamylase, maltase, sucrase, and lactase o lactose (milk sugar) is indigestible after age 4 in most humans (lack of lactase) Carbohydrate Absorption Sodium-glucose transport proteins (SGLT) in membrane help absorb glucose & galactose Fructose absorbed by facilitated diffusion then mostly converted to glucose inside the cell Some glucose is absorbed by paracellular route (solvent drag) Protein Digestion & Absorption Pepsin has optimal pH of 1.5 to 3.5 -- inactivated when passes into duodenum & mixes with alkaline pancreatic juice (pH 8) Pancreatic enzymes take over protein digestion by hydrolyzing polypeptides into shorter oligopeptides…chains shorter than 10 or 15 amino acids These include trypsin, chymotrypsin, and carboxypeptidase Brush border enzymes (carboxypeptidase again, aminopeptidase, dipeptidase) finish the task producing amino acids that are absorbed into the intestinal epithelial cells o amino acid cotransporters move amino acids into epithelial cells & facilitated diffusion moves amino acids out into the blood stream Infants absorb proteins by pinocytosis (maternal IgA) o This ability still exists in the adult small intestine as well. Fat Digestion & Absorption Fat globule emulsification droplets micelles into cell chylomicrons into lacteal Nucleic Acids, Vitamins, and Minerals Nucleases hydrolyze DNA & RNA to nucleotides o nucleosidases & phosphatases of the brush border split them into phosphate ions, ribose or deoxyribose sugar, & nitrogenous bases Vitamins are absorbed unchanged o Fat-soluble vitamins are A, D, E & K and must be absorbed with other lipids o B complex vitamins & vitamin C absorbed by simple diffusion o B12 absorbed only if bound to intrinsic factor o Which cells made this? Parietal cells of gastric mucosa Minerals are absorbed all along small intestine o Na+ cotransported with sugars & amino acids o Cl- exchanged for bicarbonate reversing stomach’s chloride shift o Iron (ferrous ions (Fe2+) only) & calcium absorbed as needed other minerals are absorbed at constant rates and the kidney is left to excrete any excess Why would women have four times as many iron transport proteins as men? Because of their menstrual cycle Water Balance Digestive tract receives about 9 L of water/day o .7 L in food, 1.6 L in drink, 6.7 L in secretions o 8 L is absorbed by the small intestine & .8 L by the large intestine Water is absorbed by osmosis following the absorption of salts & organic nutrients Diarrhea occurs when too little water is absorbed o feces pass through too quickly if irritated by bacteria o feces contains high concentrations of a solute (lactose) Constipation occurs when too much water absorbed o feces pass too slowly, feces become hardened o caused by lack of dietary fiber or exercise, laxative abuse, emotional upset also caused by chiropractic misalignment Gross Anatomy of Large Intestine 5 feet long and 2.5 inches in diameter in cadaver Begins as cecum & vermiform appendix in lower right corner Vermis – “worm” Ascending, transverse and descending colon frame the small intestine Sigmoid colon is S-shaped portion leading down into pelvis Rectum is straight portion ending at anal canal Microscopic Anatomy Mucosa is simple columnar epithelium o anal canal is stratified squamous epithelium No circular folds or villi to increase surface area Intestinal crypts (glands sunken into lamina propria) produce mucus only More Anatomy of Large Intestine Teniae coli are three ribbon-like strips of longitudinal fibers of the muscularis externa. o This is different than anywhere else in the digestive tract. Usually the longitudinal layer covers the entire surface. Haustra (-um) are pouches in the large intestine caused by the teniae coli Epiploic (omental) appendages are clublike fatty pouches of peritoneum of unknown function. Bacterial Flora & Intestinal Gas Bacterial flora populate large intestine o called the gut microbiome o ferment cellulose & other undigested carbohydrates o synthesize vitamins B and K diet alone does not usually provide enough vitamin K to ensure adequate clotting Flatus (gas) o average person produces 500 mL per day o Next question: How many “emissions” per day? 14 o most is swallowed air but it can contain hydrogen, nitrogen, carbon dioxide, methane, hydrogen sulfide, indole & skatole the last three cause the odor of feces and flatus hydrogen gas is highly flammable – flatus has been known to explode during surgeries that use electrical cauterization! Absorption and Motility Transit time of large intestine is 12 to 24 hours o reabsorbs water and electrolytes Feces consist of water & solids (bacteria, mucus, undigested fiber, fat & sloughed epithelial cells Haustral contractions occur every 30 minutes o distension of a haustrum stimulates it to contract Mass movements occur 1 to 3 times a day o triggered by gastrocolic and duodenocolic reflexes filling of the stomach & duodenum stimulates motility sort of like “Oh, there’s more coming. I can get rid of this batch.” moves residue for several centimeters with each contraction Anatomy of Anal Canal Anal canal is 3 cm total length Anal columns are longitudinal ridges separated by mucus secreting anal sinuses Rectal valves (3) are internal transverse folds of rectal tissue that enable the rectum to retain feces while passing gas Hemorrhoids are permanently distended hemorrhoidal veins that protrude into the anal canal or form bulges distal to the anus Defecation Stretching of the rectum stimulates defecation o intrinsic defecation reflex via the myenteric plexus causes muscularis to contract & internal sphincter to relax relatively weak contractions defecation occurs only if external anal sphincter is voluntarily relaxed o parasympathetic defecation reflex involves spinal cord stretching of rectum sends sensory signals to spinal cord pelvic splanchnic nerves return signals intensifying peristalsis Abdominal contractions increase abdominal pressure on the rectum (Valsalva “manure” ?) Levator ani lifts anal canal upwards Read Insight 25.5: The Man with a Hole in His Stomach Neural Control of Defecation 1. Filling of the rectum 2. Reflex contraction of rectum & relaxation of internal anal sphincter 3. Voluntary relaxation of external sphincter Cranial Nerves I. Olfactory Nerve II. Optic Nerve III. Oculomotor Nerve IV. Trochlear Nerve V. Trigeminal Nerve VI. Abducens Nerve VII. Facial Nerve VIII. Vestibulocochlear Nerve IX. Glossopharyngeal Nerve X. Vagus Nerve XI. Accessory Nerve XII. Hypoglossal Nerve