ELISA, RIA & Immunofluorescence: Principles & Applications
advertisement

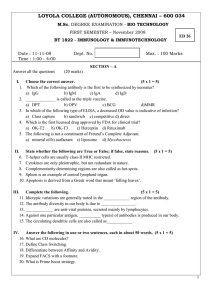
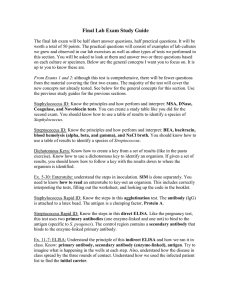
ELISA, RIA & Immunofluorescence ELISA Definition: • The enzyme-linked immunosorbent assay (ELISA) is a common laboratory technique which is used to measure the concentration of an analyte (usually antibodies or antigens) in solution. • The term ELISA was first used by Engvall & Perlma in 1971. BASIC PRINCIPLE OF ELISA Based on Basic Immunology Response Lock and Key Concept: 1) Antigen (key) 2) Antibody (lock): –Key fits into the lock Enzyme conjugate substrates • Bound to a secondary antibody that binds with the antibody-antigen complex. Basic Steps Of Enzyme-Linked Immunosorbant Assay Indirect Types of ELISA: (on the basis of procedure) Direct Types NonCompetitive Indirect Competitive Sandwich Non-Competitive: 1) Direct ELISA: • It uses a primary labeled anti-body that react directly with the antigen. • It can be performed with the antigen that is directly immobilized on assay plate. • Not widely used but common for immuno-histochemical staining of cells & tissues. Non-Competitive: 2) Indirect ELISA: • It utilizes a primary un-labeled antibody in conjunction with a labeled secondary antibody. • Secondary antibody has specificity for primary antibody. Non-Competitive: 3) Sandwich ELISA: • Antigens like Tumor markers, hormones, serum proteins may be determined. • Antigens in the sample bind with the capture antibody & become immobilized. • The antibody of the enzyme conjugate bind with the immobilized antigen to form a sandwich of Ab-Ag-Ab/ enzyme bound to microwell. Competitive: • Antibody coated microwell. • Serum antigen & labeled antigen added together .... Competition • Ab-Ag enzyme complex bound is inversely related to the conc. of antigen present in sample. • Increased serum antigen results in reduced binding of Agenzyme conjugate with the antibody producing less enzyme activity & (yellow) color formation. • Used to determine small molecules like T₃ , T₄ & Progesterone. to detect Ab (HIV, HCV) to detect Ag ( Tumor Markers, Hormones ) to detect Ag ( Free Testosterone) Comparison between Indirect Sandwich & Competitive ELISA APPLICATIONS OF ELISA 1- Hormones 7- Vaccine Quality Control 2- Proteins 8- FOR GMO (Genetically modified organism) 3- Infectious Agent ( Viral, Bacterial, Parasitic, Fungal ) 9- For Rapid Test 4- Drug Markers 10- IgG, IgM, IgA 5- Tumor Markers 11- In New Born Screening 6- Serum Proteins 12- In Clinical Research Radioimmunoassay (RIA) •Involves the separation of a protein (from a mixture) using the specificity of antibody - antigen binding and quantify it using radioactivity •The technique was introduced in 1960 by Berson and Yalow as an assay for the concentration of insulin in plasma. •Here radioactive materials are not administered to the individual but are used as reagents. 14 The technique of radioimmunoassay has revolutionized research and clinical practice in many areas, e.g., ✓blood banking ✓diagnosis of allergies ✓endocrinology 15 Principle of Radioimmunoassay Principle: Uses an immune reaction [Antigen – Antibody reaction] to estimate a ligand Ag + Ag* + Ab AgAb + Ag*Ab + Ag + Ab* ◦ Unbound Ag* and Ag washed out ◦ Radioactivity of bound residue measured ◦ Ligand conc. is inversely related to radioactivity [Ag : ligand to be measured ; Ag* radiolabelled ligand] 16 P* + Radioactive tag PQ Q + P P*Q Analyte Binding agent Free Bound 17 ✓Amixture is prepared of ▪ radioactive antigen ▪ antibodies against that antigen. ✓Known amounts of unlabeled ("cold") antigen are added to samples of the mixture. These compete for the binding sites of the antibodies. 18 ✓At increasing concentrations of unlabeled antigen, an increasing amount of radioactive antigen is displaced from the antibody molecules. ✓The antibody-bound antigen is separated from the free antigen in the supernatant fluid, and ✓ The radioactivity of each is measured. 19 20 Applications of RIA ❑ Analysis of hormones, vitamins,metabolites, diagnosticmarkers ◦ Eg. ACTH, FSH, T3, T4, Glucagon, Insulin, Testosterone, vitamin B12, prostaglandins, glucocorticoids, ❑Therapeutic drug monitoring: ◦ Barbiturates, morphine, digoxin, ❑ Diagnostic procedures for detecting infection ◦ HIV, Hepatitis A, B etc 21 RIA Sensitivity Nanomolar to picomolar More EIA Millimolar Cost Time duration More Tedious Ease of handling More Radiation hazards Less Disposal Care has to be taken Complex Easy Based on the measurement of radioactivity Based on measurement of28 enzymatic Equipment Mechanism Less Easy No Less Immunofluorescence • Immunofluorescence is a technique allowing the visualization of a specific antigen by binding a specific antibody chemically conjugated with a fluorescent dye such as fluorescein isothiocyanate (FITC). • The specific antibodies are labeled with a compound (FITC) that makes them glow an applegreen color when observed microscopically under ultraviolet light. Fluorescence • Fluorescence is the property of certain molecules to absorb light at one wave length and emit light at longer wave length when it is illuminated by light of a different wavelength. • The fluorescence can be visualized using fluorescence microscopy. The IF technique allows for a visualization of the presence as well as the distribution of target molecules in a sample. Immunofluorescence staining Direct immunofluorescence: Staining in which the primary antibody is labeled with fluorescence dye. Indirect immunofluorescence: Staining in which a secondary antibody labeled with fluorochrome is used to recognize a primary antibody. Direct immunofluorescence • Direct immunofluorescence uses a single antibody that is chemically linked to a fluorophore. The antibody recognizes the target molecule and binds to it, and the fluorophore it carries can be detected via microscopy. Advantages of direct immunofluorescence • This technique has several advantages over indirect immunofluorescence because of the direct conjugation of the antibody to the fluorophore. This reduces the number of steps in the staining procedure making the process faster and can reduce background signal by avoiding some issues with antibody crossreactivity. Indirect immunofluorescence • Indirect immunofluorescence uses two antibodies; the unlabelled primary antibody specifically binds the target molecule, and the secondary antibody, which carries the fluorophore, recognises the primary antibody and binds to it. Advantages of indirect immunofluorescence • Gives an amplification effect - more label per molecule of target protein. • Requires only one labeled antibody to identify many proteins- Same labeled secondary antibody can be used to bind to many different proteins. A different primary antibody is used for each target protein. Variable part of primary antibody binds to specific part of target protein. • The secondary antibody binds to the constant part of the primary antibody. Therefore a sample of the same batch of secondary antibody can bind to many different primary antibodies • Applications • Immunofluorescence can be used on tissue sections, cultured cell lines, or individual cells, and may be used to analyse the distribution of proteins and small biological and nonbiological molecules. • Immunofluorescence can be used in combination with other, non-antibody methods of fluorescent staining, for example, use of DAPI, (4',6-diamidino-2-phenylindole) is a fluorescent stain that binds strongly to A-T rich regions in DNA, to label DNA • The technique has a number of different biological applications including evaluation of cells in suspension, cultured cells, tissue, beads. • It also play a key role in the diagnosis of autoimmune disorder. Limitation • • • • Quality and concentration of the antibody. Proper handling of the specimen. Choice of secondary antibodies. Fluorophores undergoes photobleaching as they are exposed to light