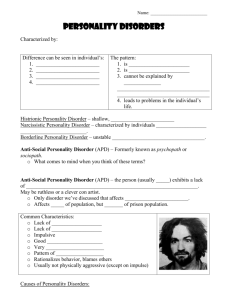
Lecture 8 – Chapter 13 A personality disorder is: o Persistent pattern of emotions, cognitions, behaviour resulting in enduring emotional distress for affected person and others and can be traced back to adolescence or early adulthood o An enduring pattern of inner experience and behavior that manifests in two or more of the following: cognition, affectivity, interpersonal functioning, impulse control o Personality disorders have a negative prognostic significance for Axis I disorders such as anxiety and mood disorders o Distress may (or may not) be subjective o Causes difficulties with work and relationships Category of personality disorders is controversial: o Categorical and dimensional models Problems of kind vs. problems of degree Five-factor model of personality to be used as a meaningful way of measuring personality traits This model considered normal universal Personality disorder clusters o DSM-5 divides personality disorders into three groups (clusters) Cluster A: odd or eccentric Cluster B: dramatic, emotional, erratic Cluster C: anxious, fearful Statistics and development o Personality disorder are common (6-13% of the adult population in the US) o Same person can be diagnosed with different personality disorders at different times o Higher prevalence in high-income countries o Histrionic personality disorder biased against females o Antisocial personality disorder biased against males o Comorbidity – being diagnosed with more than one disorder/disease Cluster A disorders Paranoid personality disorder Clinical description: a pervasive distrust and suspiciousness of others such that their motives are interpreted as malevolent o Argumentative, may complain, quiet, hostile towards others, suicidal Persistently bears a grudge Perceives attacks on his character o Suspicious, mistrustful of others without justification Suspects others are exploiting or deceiving him Recurrent suspicions regarding fidelity of spouse or sexual partner o Bears relationship to paranoid type of schizophrenia and delusional disorder Is reluctant to confide in others because he believes they will use the information against him Reads hidden demeaning meanings into benign remarks o Prevalence: 2% Causes o Genetics o Heritability: 0.34 o Relatives with schizophrenia o Mistreatment or traumatic childhood experiences o Cognitive cultural factors Treatment o Cognitive therapy to change mistaken assumptions about others Schizoid personality disorder Clinical description: pervasive pattern of detachment from social relationships and restricted expression of emotion with 4 or more of the following: Neither desires nor enjoys close relationships Almost always chooses solitary activities Little if any interest in sexual experiences with another person Takes pleasure in few if any activities Lacks close friends other than first-degree relatives Appears indifferent to praise or criticisms of others Shows emotional coldness or flattened effect o Detachment from social relationships, no desire to enjoy closeness with others, cold, aloof o Homelessness o Extreme social deficiencies o Social isolation, poor rapport, and constricted affect o Prevalence: 1% Causes o Childhood shyness, abuse, neglect, low-density dopamine receptors o Heritability: 0.43 Treatment o Social skills training (Role-playing) o Limited outcomes Schizotypal personality disorder Clinical description: a pervasive pattern of social and interpersonal deficits with reduced capacity for close relationships as well as cognitive or perceptual distortions and eccentricities of behaviour with 5 or more of the following: Ideas of references Odd beliefs or magical thinking Unusual perceptual experiences including bodily illusions Odd thinking and speech Suspiciousness or paranoid ideation Inappropriate or constricted affect Behaviour or appearance that is odd or eccentric Lack of close friends other than first-degree relatives Excessive social anxiety that does not diminish with familiarity o Social deficits, psychotic-like symptoms, cognitive impairments/paranoia o Magical thinking o Report unusual perceptual experiences o Hypersensitive to criticism as children o Prevalence: 1% Causes o Genetics, prevalence of disorder in relatives Heritability: 0.54 o Left hemisphere damage; brain abilities May be cause of magical ideation Treatment o Antipsychotic medication, community treatment, social skills training, CBT Cluster B disorders Antisocial personality disorder Clinical description: a pervasive pattern of disregard for and violation of the rights of others occurring since the age of 15 years as indicated by 3 or more of the following: Failure to conform to social norms with respect to lawful behaviours Deceitfulness and conning others for personal profit or pleasure Impulsivity or failure to plan ahead Irritability or aggressiveness as indicated by repeated fights or assaults Reckless disregard for safety of self or others Consistent irresponsibility Lack of remorse There is evidence of conduct disorder with onset before age 15 o Aggressive, lying, cheating, no remorse, substance abuse, unnatural death in boys with this disorder o Moral insanity, egopathy, sociopathy, and psychopathy o Conduct disorder in children o 50% to 80% of male offenders diagnosed with this disorder o Prevalence: 1-4% Genetic influences o Gene-environment interaction o Heritability: 0.41 o Chronic stress in family o Academic difficulty, peer problems, low family income, neglect and harsh discipline from parents o Under arousal of cortex, fearlessness Neurobiological influences o Executive cognitive function deficits in psychopaths Under arousal hypothesis – abnormally low levels of cortical arousal, which causes fearlessness Fearlessness hypothesis – antisocial and risk-taking behaviours o Insufficiently developed cortices o Deficient MAOA due to defective gene producing it o Study by Blair found person with psychopathic tendencies showed decreased amygdala and orbitofrontal cortex responses to emotionally provocative stimuli which the author felt was suggestive of difficulties with basic forms of emotional learning and decision making Psychological and social dimensions o Failure to abandon an unattainable goal o Aversive interchange with parents o Parents inept monitoring of child’s activities o Inconsistent parental discipline at home o Experience of physical abuse An integrative model o Genetic vulnerability to antisocial behaviours and personality traits Leads to under arousal and fearlessness Weak inhibition systems and overactive reward system Differences in emotions and cognition Treatment o Multifaceted for juvenile offenders o CBT o Parent training for diagnosed children o Comorbid with alcohol dependence and depressive disorders Prevention o Preschool program combining good parenting skills and family support Borderline personality disorder Clinical description: a personality disorder in which there is a marked tendency to act impulsively without consideration of the consequences, together with affective instability. The ability to plan ahead may be minimal, and outbursts of intense anger may often lead to violence or behavioural explosions, these are easily precipitated when impulsive acts are criticized or thwarted by others. Two variants of this disorder: Impulsive type: the predominant characteristics are emotional instability and lack of impulse control. Outbursts of violence or threatening behaviour are common, particularly in response to criticism by others Borderline type: several of the characteristics of emotional instability are present; in addition, the patient’s own self-image, aims, and internal preferences (including sexual) are often unclear or disturbed. There are usually chronic feelings of emptiness. A liability to become involved in intense and unstable relationships may cause repeated emotional crises and may be associated with excessive efforts to avoid abandonment and a series of suicidal threats or acts of self-harm (although these may occur without obvious precipitants). o Turbulent relationships, fear of abandonment, self-mutilating behaviours, no control over emotions o Pervasive pattern on instability of interpersonal relationships, self-image and affects and marked impulsivity as indicated by 5 or more of the following: Frantic efforts to avoid abandonment Unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation Identity disturbance Impulsivity in at least two areas that are potentially self-damaging Recurrent suicidal behaviors, gestures or threats or self-mutilating behaviours Affective instability due to a marked reactivity of mood Chronic feelings of emptiness Inappropriate anger Transient, stress-related paranoia o Subtypes: Dependent – ambivalent unstable relationships Impulsive – in multiple areas including breaking the law Borderline – emotional instability and disturbed self-image o Often engage in suicidal or self-mutilating behaviours o Approximately 10% die by suicide o 75% achieve remission six years after initial treatment o Prevalence: 2-3% Similar prevalence between genders in general population. Females > males in clinical populations Causes o Genetics, related to mood disorders o Early trauma and biological predisposition Beginning in adolescence or early adulthood o Memory bias (for negative cognitions typical of this disorder) o o o o Childhood sexual abuse; similarities with PTSD Experienced rapid cultural changes Heritability: 0.61 Individuals poor emotional development, scarred by trauma and emotional deficits, with failure to adapt to adapt environment to child’s needs Treatment o Antipsychotic and antidepressants (no medication is effective for BPD yet, medication is used to treat comorbid disorders) Sedatives should not be used for more than a week o Dialectical behaviour therapy (DBT) Effective in reducing suicide attempts o Treatments similar to those with PTSD o Couples therapy o Treatment of adolescents with BPD should usually be delivered as outpatient Symptoms o Substance misuse o Mood swings o Abnormal eating o Self-harm o Relationship problems Burden of illness o Stress of risk-taking behaviour on families o Communication problems with parents o Physical consequences of risk-taking behaviours o Observational studies of mothers with BPD: Less availability Poorer organisation of behaviours and mood Lower expectation of positive interactions More often overprotective/intrusive Less demonstrative/sensitive Higher rates of parent’s separation and loss of employment disorganized attachment Increased rate of depression for the child Comorbidity o Depression (71%), anorexia (40%), alcohol abuse (24%), substance abuse (8%) Histrionic personality disorder Clinical description: pervasive pattern of excessive emotionality and attention seeking indicated by five or more of the following: Uncomfortable in situations in which he is not the center of attention Interaction with others often characterized by inappropriate sexually seductive behaviour Displays rapidly shifting and shallow expression of emotions Consistently uses physical appearance to draw attention to self Has a style of speech that is excessively impressionistic and lacking in detail? Shows self-dramatization and exaggerated emotion Is suggestible Considers relationships to be more intimate than they are o Dramatic, theatrical, self-centred, vain, seek constant reassurance, impulsive View situations in global, black-and-white terms Speech is often vague, lacking in detail o Higher in women: may be over diagnosed Western “stereotypical female”; overdramatic, vain, seductive, overconcerned with physical appearance o Prevalence: 2% Causes o Co-occurs with antisocial personality disorders o Heritability: 0.59 Treatment o Improving problematic interpersonal relationships o Teaching appropriate ways of negotiating their wants and needs o Comorbid with alcohol dependence, somatization disorder Narcissistic personality disorder Clinical description: a pervasive pattern of grandiosity (in fantasy or behavior), need for admiration, lack of empathy as indicated by 5 or more of the following: Grandiose sense of self-importance Preoccupied with fantasies of unlimited success, power, brilliance or beauty Believes he is special and can only be understood or should associate with other special or high-status people Requires excessive admiration Has a sense of entitlement Is interpersonally exploitive Lacks empathy Is often envious of others and believes others are envious of him Shows arrogant, haughty behaviours or attitudes o Unreasonable sense of self-important, grandiosity o No compassion for others, envious, arrogant o Frequently depressed o Prevalence: 0.5-1% Causes o Failure of empathetic mirroring from parents o Child remains fixated at self-centred, grandiose stage of development o Heritability: 0.5 Treatment o CBT, coping strategies (relaxation training, accepting criticism), empathizing, treatment for depression Cluster C disorders Avoidant personality disorder Clinical description: A pervasive pattern of social inhibition, feelings of inadequacy and hypersensitivity to negative evaluation as indicated by four or more of the following: Avoids social occupations that involve significant interpersonal contact Is unwilling to get involved with people unless certain of being liked Is preoccupied with being criticized in social situations Shows restraint in intimate relationships because of fear of being shamed or ridiculed Inhibited in new interpersonal situations because of feeling adequate Views self as socially inept and unappealing Is unusually reluctant to take personal risks or engage in any new activities because they may prove embarrassing o Interpersonally anxious, fear rejection, pessimistic about their future o Prevalence: 1-2% Causes o Born with difficult temperament, parental rejection, uncritical love Low self-esteem, social alienation persisting into adulthood o Overreactive behavioural inhibition system o Heritability: 0.42 Treatment o Social skills training o CBT: gradual exposure to feared situations o Systematic desensitization: relaxing in the presence of feared situations o Behavioural rehearsal: patients act out situations that cause anxiety o Treatment leads to modest improvements in behaviour o Comorbid with social phobia Dependent personality disorder Clinical description: a pervasive and excessive need to be taken care of that leads to submissive and clinging behaviours and fears of separation as indicated by 5 or more of the following: Has difficulty making everyday decisions without an excessive amount of reassurance Needs others to assume responsibility for most major areas of his life Has difficulty expressing disagreement with others because of fear of loss of approval Difficulty initiating projects on his own because of lack of self confidence Goes to excessive lengths to obtain nurturance and support from others Feels uncomfortable or helpless when alone Urgently seeks another relationship as a source of care and support when a relationship ends Is unrealistically preoccupied with fears of being left to take care of himself o Interpersonally dependent, anxious o Submissive, timid, and passive o Feelings of inadequacy, sensitive to criticism, need reassurance o Cling to relationships o Prevalence: 0.5% Causes o Disruptions in early childhood lead to fears of abandonment o High in sociotropic traits o Low on individualistic achievement traits o Heritability: 0.56 Treatment o Developing confidence; ensuring patient does not over depend on therapist Obsessive-compulsive personality disorder Clinical description: a pervasive pattern of preoccupation with orderliness, perfectionism and mental and interpersonal control at the expense of flexibility, openness as indicated by four or more of the following: Preoccupied with details, rules, lists, order or schedules to the extent that the major point of activity is lost Shows rigidity and stubbornness Perfectionism that interferes with task completion Excessively devoted to work and productivity to the exclusion of leisure activity and friends Over conscientious and inflexible about matters of morals or ethics Is unable to discard worn or worthless objects even those without sentimental value Reluctant to delegate tasks Adopts miserly spending style toward self and others o Rigidity, poor interpersonal relationships, quest for perfectionism o Prevalence: 2% Causes and treatment o Genetics Heritability: 0.60 o Relaxation techniques, CBT to reframe compulsive thoughts Personality disorders under study Sadistic personality disorder – receiving pleasure by inflicting pain on others Passive-aggressive personality disorder – people are defiant and refuse to cooperate with requests Treatment Can reduce symptomatology, improve social and interpersonal functioning, reduce frequency of maladaptive behaviours and decrease hospitalizations Always screen for comorbid disorders If the personality disorder is ego-syntonic, it will be hard to engage the client in treatment Increasing serotonin levels may reduce depression, impulsiveness, rumination and may enhance a sense of well being Low dose neuroleptics and mood stabilizers can be effective in modulating affective stability