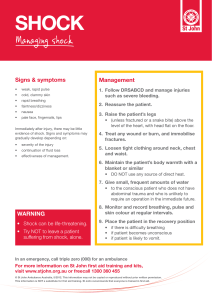
-isolated traumatic brain injury with increased ICP causes an increased BP and decreased pulse -hyperventilation in a TBI patient causes vasoconstriction and increased cerebral ischemia -pulmonary contusion is caused by hemorrhage into the lung parenchyma -the cause of secondary brain injury is hypoxia - cardiac arrest, treating an airway obstruction or if the scene becomes unsafe the primary assessment can be interrupted -monitoring the level of conscious in a pediatric patient is the best way to follow changes in a head injury -the lungs will suffer the least structural damage from a bullet wound -shock is what distinguishes a simple pneumothorax from a tension pneumothorax -external arterial bleeding should be managed in a trauma patient before airway obstructions -the most common cause of cardiopulmonary arrest in the trauma patient is hypoxemia -a narrowed pulse pressure is usually associated with post-traumatic hemorrhage early shock -immobilization onto a longboard is not indicated in penetrating wounds to the torso neck, or head SHOCK Compensated: 15-25% blood loss, tachycardia, narrowed pulse pressure, thirst, delayed capillary refill Decompensated: 30-45% blood loss, hypotension, no peripheral pulse, prolonged capillary refill Hypovolemic Shock (absolute hypovolemia/low-volume): caused by hemorrhage or other major bodily fluid loss, typically decreased LOC, rapid and shallow breathing, pulse is raid and thready, skin is cool/clammy and pale Disruptive Shock (relative hypovolemia/high-space): condition causing the blood vessels to be too large for a normal amount of blood. Typically decreased LOC, diaphragmatic breathing, weak normal or slow pulse, skin colour normal without diaphoresis -neurogenic shock: occurs most often after an injury to the spinal cord causing loss of normal vascular tone Obstructive Shock (mechanical shock): any traumatic or medical condition that slows or prevents the venous return of blood, typically decreased LOC, rapid and laboured breathing, weak/thready possibly irregular pulse and absent radials, pale/cool/ diaphoretic possibly cyanotic skin Cardiogenic Shock (pump failure):pumping strength is reduced, cardiac output falls, and decreases blood pressure ESSENTIAL INFORMATION -perform reassessment exam when patients condition changes, you move the patient or complete an intervention -perform a secondary exam to look for additional missed injuries -trauma assessment treatment decision tree provides actions based on assessments pg. 46 - FOUNDATIONAL KNOWLEDGE SPECIAL POPULATIONS -burn damage occurs when heat or caustic materials come in contact with the skin -the zone of coagulation is where portions of the skin are necrosed by the thermal insult -the zone of stasis is where blood flow is compromised and tissues will die if blood flow is not restored -the zone of hyperemia is where there is increased blood flow to the tissues as a result of inflammatory mediators -superficial or first degree burns result in minor tissue damage, the skin is red with no blisters -partial thickness or second degree burns cause damage to the epidermis and into a variable depth of the dermis, the skin is mottled red with blisters and usually the most painful -full thickness or third degree burns cause damage to all layers of the epidermis and dermis, the skin is pearly white and charred or translucent -for smaller or irregular burns the size can be estimated by the palmar surface of the patient being 1% of the skin tissue -in the adult the head, each leg and the arms together are 9% of the body tissue and the front and back are 18% each - in the child the head is instead 18% and the legs are 7% -the burning process must be halted immediately upon removal off the patient from the source of the burn -care of the burn itself has a low priority compared to airway and excessive bleeding management -critical problems in the burn patent the require immediate intervention include airway compromise, altered mental status and the presence of major injuries -hoarseness, stridor or a persistent cough indicate involvement of deeper airway structures -wheezing or rales indicate the involvement of lower airway injury from inhalation -cooling should be done with tap water at room temperature and should be undertaken for no more than 5-10 minutes -the patient should be covered even when the environment is not cool -lactated ringer's solution is preferred for fluid resuscitation in burn patients -eschar can cause swelling and result in loss of circulation or limit chest excursion -inhalation injuries are classified as carbon-monoxide poisoning, heat-inhalation injury or smoke (toxic) inhalation -an altered level of consciousness is the predominant sign of hypoxia -treat patients with suspected carbon monoxide poisoning with high flow oxygen by mask -heat inhalation injuries are confined to the upper airway and tissue swelling can easily progress to complete airway obstruction -treat bronchospasm with inhaled albuterol and oxygen -chemical burns may not only injure the skin but also be absorbed an cause internal organ failure -all contaminated patients should be decontaminated prior to transport -irrigation of caustic chemicals in the eye is especially important as it can cause irreversible damage -the most serious injury that results from electrical burns is cardiac arrhythmias -fractures and dislocations may be present due to violent muscle contractions -rhabdomyolysis is the breakdown of muscle with the release of myoglobin into the circulation and renal failure -in lightning injuries the patient remains in respiratory arrest which is followed by a second cardiac arrest due to hypoxia -if a patient is awake and breathing after a lightening strike they will likely survive without further intervention -in pediatric patients they are at greater risk for injury following a burn such as hypothermia because of there thinner skin - TRAUMA SCENARIO Primary Survey Scene size-up - I am donning my BSI - Are there any hazards - How many patients do I have - Do I need more resources - What is the mechanism of injury, is it generalized or focused Initial Assessment - Are there any bystanders - What is the general impression of the patient - Is there any life threatening bleeding - Take c-spine, ask if there is any numbness, pain or tingling - Assess LOC, AVPU - What is the chief complaint, the signs and symptoms - Is the airway patent, is there any snoring, gurgling, stridor or silence - Is breathing present, rate depth effort. Am I administering O2? - Is circulation present? Rate, rhythm, quality at carotid or radial - What is the pts skin condition, temperature, colour and capillary refill - Has the bleeding been controlled? If not apply a tourniquet - Is this a focused or rapid exam? Rapid Trauma Survey - Obtain baseline vital signs, pulse, respiration, blood pressure, O2 stat, skin condition, - If altered mental status, BGL, pupils and GCS - Looking for DCAP BLS TIC (but can ask instead pain, numbing or tingling) - Start at head, is there JVD, is the trachea midline, are you applying a c-collar - Is the chest asymmetrical, is there any paradoxical motion, auscultating for heart and lung sounds, percuss the apex and bases of lungs - Palpating the abdomen - Squeeze down on pelvis, is there any discharge - Checking upper and lower extremities, checking motor and sensory present, pedal pulse? - Check posterior - If critical continue to reassessment exam, if stable continue to secondary survey 1: Reassessment Exam - SAMPLE - LOC, AVPU, check pupils PERL - Check vital signs again: pulse, BP, RR, skin, temp, SPO2, BGL, GCS - Is the airway open and clear, any irregular sounds What is the rate, depth and effort of breathing What is the rate, rhythm, quality at the carotid and radial, skin condition, temperature and cap refill, bleeding still controlled Neck: injuries, JVD, trachea midline Chest: lung and heart sounds, chest movement, pain Palpate abdomen Reassess LOC, ABC, interventions and vitals every 5 minutes 2: Secondary Survey - Reassess LOC and ABC - SAMPLE - Vital signs: BP, RR, pulse, pupils, GCS, BGL, skin condition, temperature, SPO2 - Reassess interventions - Check head, neck, chest, abdomen, pelvis, lower/upper extremities - Reassess LOC, ABC, interventions and vitals every 15 minutes