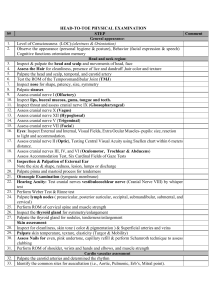
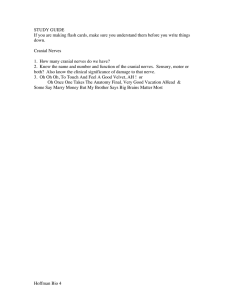
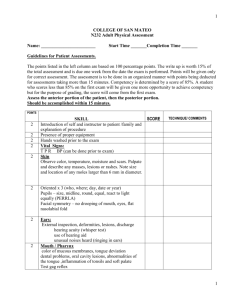
NURA 304 Health Assessment Health Assessment Validation Tool Health Assessment Validation Tool Refer to the health assessment validation guidelines for additional information. PRIVACY/SAFETY/PURPOSE 15 points Wash hands Gather supplies needed for the exam and bring them to the bedside Greet patient & identify the patient by checking the armband and using 2 identifiers Create and maintain an appropriate environment Provide privacy throughout the exam Introduce self and purpose of exam Indicate confidentiality (information only shared with health care team) Utilize effective communication skills /explain procedures Position patient appropriately being sure they are as comfortable as possible Wear appropriate attire--Don gloves and/or PPE (when indicated) Organize assessment (supplies, procedures, time management) ABBREVIATED/INTEGRATED BEDSIDE ASSESSMENT 2 1 2 3 1 1 1 4 70 points WHEN OBSERVING OR ASKING QUESTIONS YOU MUST VERBALIZE YOUR FINDINGS/OBSERVATIONS General Survey (overview of patient) – VERBALIZE FINDINGS Observe physical development- patients actual age contrasted to how they appear Observe body build, weight and height and posture Observe level of hygiene, grooming and dress Observe behavior, comfort level or signs of distress, and non-verbal signs Is the patient’s speech clear, can they hear, and what is their primary language? Mental/Neuro Status Observe movement of extremities (state if they are smooth and controlled) Test symmetric muscle strength (hand grip, feet) Observe gait (walking to BR or in hall) Observe balance (sitting and standing- Romberg test for standing) Respiratory 1 1 1 1 1 8 points Orientation to person, place, time PERRLA (Pupils Equal, Round, Reactive to light & Accommodation) [cranial nerve III, IV, VI] Assess eyes for convergence Musculoskeletal 5 points Observe color of face, lips and nail beds Assess respiratory rate and rhythm Look at characteristics of respirations (pattern, depth, work of breathing) Assess breath sounds (bilaterally, anterior & posterior all fields) 3 4 1 7 points 1 2 2 2 9 points 2 1 2 4 Cardiac/Heart 10 points Assess apical pulse rate and rhythm Auscultate for extra sounds (A, P, T, M with diaphragm & bell) 2 8 Peripheral Vascular Palpate temperature of arms, hands, legs and feet Assess capillary refill (upper & lower extremities--bilaterally)(fingernails & toenails) Palpate pulses (upper & lower extremities--bilaterally) (R, PT, DP) Gastrointestinal (Abdomen) Observe appearance (flat, rounded, distended) and for pulsations Auscultate bowel sounds (4 quadrants) Palpate for tenderness (light palpation) Ask patient about bowel movement patterns (frequency, color, amount) Genitourinary (observation/inquiry) Ask patient about voiding pattern (normal frequency, do they have a catheter) Ask or observe characteristics of urine (color, odor, appearance) Integumentary (Skin / Hair/ Nails) 2 2 3 6 points 1 2 2 1 2 points 1 1 9 points Assess skin integrity (intact or areas of breakdown, ant & post surfaces); lesions/wounds 4 Assess skin turgor (elastic, tenting, diaphoretic) 2 Assess overall color (normal for race, pale, cyanotic, flushed, jaundiced, erythema) 1 Assess mucus membranes (pink, moist) 2 Pain 7 points 7 points State you would observe patients facial expression and posture / non-verbal’s Ask patient to rate pain on a scale of 0-10 Ask patient location (where is pain?) Ask patient a minimum of 4 characteristics (describe the pain) FOCUSED/PROBLEM ORIENTED ASSESSMENT 1 1 1 4 15 points 1. Integumentary (Skin / Hair/ Nails): Ask patient if they are experiencing any skin problems or changes in skin condition Assess for dryness or moisture anteriorly and posteriorly Assess for lesions or wounds anteriorly and posteriorly (description, location) Assess finger nails and toe nails (shape, texture, color, capillary refill) Assess hair & scalp (distribution, texture, inhabitants) 2. Respiratory: Ask patient “Do you have a cough? Is it productive?” Ask patient “Do you have any difficulty breathing— any chest tightness or shortness of breath?” Ask patient if they smoke; How much? How long? Assess O2 saturation / oxygen requirement Inspect chest configuration Observe use of accessory muscles Percuss over anterior & posterior chest Assess chest expansion (excursion) 3. Peripheral Vascular: Ask patient if they are experiencing any signs of swelling in legs or feet. Assess for edema (facial, upper & lower extremities-- bilaterally) Inspect lower extremities for color, temperature, hair distribution, vascularity Assess for sensation 4. Cardiovascular: Ask patient if they have been experiencing any chest pain Ask patient if they have a history of palpitations, high BP, or high cholesterol Assess for neck vein distention Inspect for heave or lift; palpate for thrill Palpate carotids (individually) Auscultate with bell Palpate abdominal aorta Auscultate with bell 5. Musculoskeletal: Functional ROM: Ask patient if they are able to complete ADLs such as dress yourself, brush teeth & hair Assess for joint swelling and tenderness (palpate elbows, fingers, knees, toes) Inspect & palpate spine Palpate joints & muscle groups for symmetry o Shoulders→elbows→wrists→fingers o Hips→knees→ankles→toes Assess muscle strength (bilaterally against resistance) o Shoulders→arms→wrists→fingers o knees→ankles Assess ROM (bilaterally) o Shoulders→elbows→wrists→fingers [cranial nerve XI] o Hips→knees→ankles 6. Neuro: Ask patient if they have any numbness or tingling in any of your extremities Ask patient if they have any problems with headaches, dizziness, falling Assess memory o Immediate o Recent (24 hr memory) o Remote (past dates & historical accounts) Assess light touch sensation [cranial nerve V] o Face o Upper extremities o Lower extremities Assess sharp/dull discrimination [cranial nerve V] o Upper extremities o Lower extremities Assess Deep Tendon Reflexes (DTRs): o Biceps tendon o Triceps tendon o Patellar reflex 7. Ears: Nose: o Plantar reflex Assess swallowing [cranial nerve IX, X] Assess coordination (Tandem walking) Ask patient if they wear a hearing aid Ask patient if they have had any recent changes in their hearing Inspect & palpate pinna & tragus Whisper test [cranial nerve VIII] Assess patency Inspect nasal mucosa and nasal septum Olfactory (smell) function [cranial nerve I] Mouth / Throat: Ask patient if they wear dentures; inspect teeth Have patient stick out tongue and move side to side or say “light, bright, dynamite” [cranial nerve XII] Inspect throat - Observe for rise of uvula [cranial nerve IX, X]; tonsils Eyes: Ask patient: Do you wear glasses? All the time or reading glasses? Ask patient: Have you had any recent changes in your vision? Inspect distribution of eyelashes & brows Inspect lids for swelling, ptosis [cranial nerve III, IV, VI] Inspect sclera Fields of gaze [cranial nerve III, IV, VI] 8. Cranial nerves: CN I—sense of smell CN II—Snellen chart or reading to assess vision CN III—6 fields of gaze / ptosis / PERRLA CN IV—6 fields of gaze / ptosis / PERRLA CN V—contraction of masseter muscle & light touch sensation over face CN VI—6 fields of gaze/ ptosis / PERRLA CN VII—symmetrical movements of face (puff cheeks, smile, frown) CN VIII—whisper test CN IX—swallowing & uvula rise with “aah” CN X—swallowing & uvula rise with “aah” CN XI—turn head against resistance, shrug shoulders against resistance CN XII—test tongue movement by saying “light, bright, dynamite” or push tongue against cheek Grade: _________ Student: ________________________________ Student signature: __________________________________ Faculty: _________________________________ Date: _______________________________________ Revised FEK 3/19