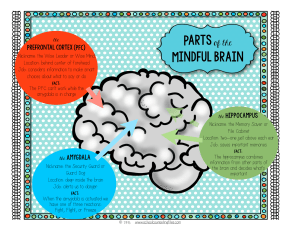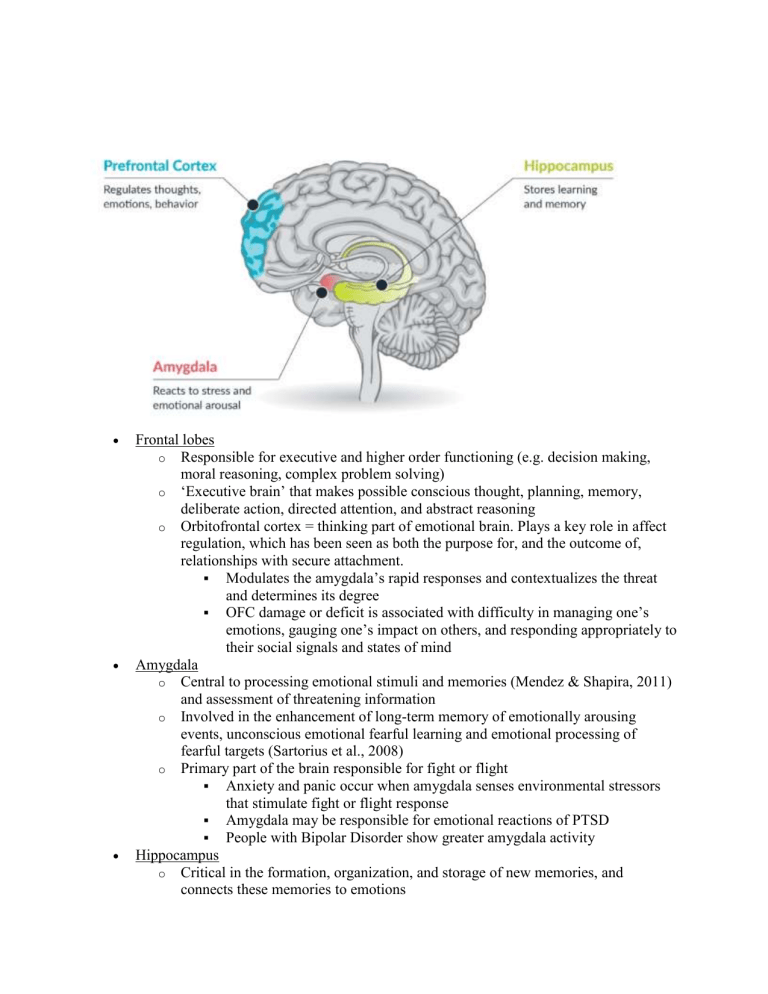
Frontal lobes o Responsible for executive and higher order functioning (e.g. decision making, moral reasoning, complex problem solving) o ‘Executive brain’ that makes possible conscious thought, planning, memory, deliberate action, directed attention, and abstract reasoning o Orbitofrontal cortex = thinking part of emotional brain. Plays a key role in affect regulation, which has been seen as both the purpose for, and the outcome of, relationships with secure attachment. Modulates the amygdala’s rapid responses and contextualizes the threat and determines its degree OFC damage or deficit is associated with difficulty in managing one’s emotions, gauging one’s impact on others, and responding appropriately to their social signals and states of mind Amygdala o Central to processing emotional stimuli and memories (Mendez & Shapira, 2011) and assessment of threatening information o Involved in the enhancement of long-term memory of emotionally arousing events, unconscious emotional fearful learning and emotional processing of fearful targets (Sartorius et al., 2008) o Primary part of the brain responsible for fight or flight Anxiety and panic occur when amygdala senses environmental stressors that stimulate fight or flight response Amygdala may be responsible for emotional reactions of PTSD People with Bipolar Disorder show greater amygdala activity Hippocampus o Critical in the formation, organization, and storage of new memories, and connects these memories to emotions o o o Part of the parasympathetic nervous system -- enables us to settle down Memories that register with the help of the hippocampus are explicit, linguistically retrievable, and contextualized according to time, place, and person Acute relational trauma can shut down the hippocampus temporarily or inhibit its development → unmodulated reactivity of the over vigilant amygdala (Wallin, 2007) Neurotransmitters: Dopamine o Feel good, love, reward-motivated behavior, helps regulate emotional responses o Associated disorders: Low → Parkinsons, ADHD, Depression High → Schizophrenia o Excitatory & Inhibitory o Movement & flow of information to front of brain; Mediate desire and motivation o Linked to reward systems Rewards tend to increase Dopamine (eg. social media likes) Impacts anticipation & drive o Schizophrenia <> High Dopamine Anti-psychotics block Dopamine Drugs that release dopamine cause Schizophrenia o ADHD <> Low Dopamine o Linked to substance abuse Serotonin o Well-being and happiness o Associated with mood disorders o Inhibitory o Feel good o Physiological processes: Mood, appetite, sleep, and pain o Depression <> Low Serotonin o OCD Epinephrine (Adrenaline) o Vigilant alertness, increased heart rate, underlines the fight or flight response o Mostly excitatory (during times of stress) o Raises blood pressure o May trigger anxiety GABA o Regulates communication btwn brain cells o Inhibits activity of neurons o Helps control fear and anxiety o Associated Disorders Low → Anxiety o Inhibitory (primary one) o Benzodiazepine system – bind to same receptors as GABA o Reduces anxiety Oxytocin o The love hormone o Produced during hugging, orgasm, child-birth o Influences social behavior and emotion – reduces stress and anxiety o Can be helpful for anxiety, depression (esp. postpartum), autism Homeostasis: body responds to environment in way that makes internal workings of body stable. Maintain right pH, temperature… Threats of dangers = stressors HPA axis o o o o Control’s body’s response to stress Amygdala senses threat and activates HPA axis Hypothalamus synthesizes CRH which stimulates the pituitary gland to secrete ACTH ACTH stimulates adrenal glands to produce cortisol (stress hormone) and epinephrine (adrenaline) – primes body for instant action Fight or Flight Response Sympathetic Nervous System – get out of danger mode – adrenaline causes physiological changes o Increased heart rate o Increased respiratory rate (breathing faster to get more oxygen in blood and expel more Co2) o Increased peripheral vasoconstriction (arms and legs tighten to push more blood to core area) o Digestion, immune function, ovulation shut down (butterflies) After the Threat Negative feedback loop: The hypothalamus recognizes higher level of cortisol and sends messages to suppress CRH and ACTH production Parasympathetic Nervous System activates the “rest and digest” response and returns the body to homeostasis after the flight-or-fight response by activating the release of the neurotransmitter acetylcholine o Vasodilation (opening of blood vessels), decreases heart rate, increases digestion Chronic Stress Repeated exposure causes individual to habituate with repeated HPA axis activation and decreases ability to regulate HPA axis activation HPA becomes too responsive and doesn’t turn off Continuously increases the cortisol secretion which desensitizes the glucocorticoid receptors in hypothalamus (negative feedback loop) resulting in hyperactivity of the HPA axis (Jeon & Kim, 2018). o increases activity level and number of neural connections in amygdala o In excess cause atrophy of the hippocampus (learning, memory, stress control), resulting in impaired memory, decrease in ability to learn, and impaired ability to respond appropriately to stress. Brain shrinks in size (loss in synaptic connections between neurons) Frontal cortex (concentration, judgment, decision making) shrinks Early Life Stress/Trauma Exposure to mild or moderate stressors early in life has been shown to enhance HPA regulation and promote a lifelong resilience to stress versus early-life exposure to extreme or prolonged stress can induce a hyper-reactive HPA Axis and may contribute to lifelong vulnerability to stress Nurturing mother gives to baby determines how well baby deals with stress – neglect leads baby to develop more cortisol receptors (dampens stress response) and become more sensitive to stress (DeBellis 2001). o More cortisol = hyperactive HPA axis, increased activity of amygdala, atrophy of hippocampus (decrease in memory, learning, stress control) If HPA Axis is impacted early in life (e.g. childhood trauma or maltreatment), a lot of cortisol is released over a long period of time, damaging the circuit and making you less sensitive, the system (negative feedback loop) no longer works as an effective signaling device because its desentized (e.g. no longer can identify cues for danger in environment). Exposure to trauma → cascade of biological changes and stress responses, which are associated w/PTSD, mental illnesses, and substance use disorders. This in turn increases a person's vulnerability to encountering subsequent traumas/violence as an adult. Transgenerational trauma can also occur, with traumatic experiences as well as resilience patterns being developed and inherited from subsequent generations (e.g. children of Holocaust survivors, Braga 2012). Trauma (Rasmussen and Bliss) Overactive limbic system and hypoactive frontal lobe interferes cognitive processing, lead to trauma reenactment; Activated SNS (activated by amygdala; increase energy output to respond to threat) responsible for fight-or-flight response, lead to hypervigilance; PNS (regulate stress by inhibiting SNS) related to freeze response, lead to dissociation; Elevated cortisol and norepinephrine interferes hippocampus functioning, inhibiting cognitive evaluation and memory storage, lead to blanking in memory; HPA axis: Hypothalamus release CRH, stimulates pituitary gland release ACTH, then adrenal gland releases cortisol, sensitizing the nervous system to threats; CRH stimulates the release of beta-endorphin, which reduces physical and emotional pain related to trauma and leads to avoidance and numbing; increase cortisol level relates to improved emotionally relevant memories, contribute to overgeneralization of negative experience to situations that others might judge as nonthreatening. Interfered hemispheric integration. Left: conscious logic, linearity and language; Right: process unconscious social and emotional information. So, either raw emotion without cognitive mediation or raw logic without the benefit of emotional awareness. Holsboer & Ising (2010) o Real or perceived stress, both psychological and psychosocial, are associated with structural changes of the prefrontal cortex, amygdala, septum, hypothalamus, and the hippocampus, a region of the brain that is sensitive to stress o Structural changes o HPA Axis: The biological stress response is generally adaptive but researchers have hypothesized that in PTSD it becomes maladaptive and leads to long-term negative consequences Chronicity of stress leads to changes in HPA Axis o Hippocampus: PTSD is linked with decreased volume in the hippocampus (learning, memory, stress response) o Studies o (Carter, 2009): The external cause of PTSD is the experience of trauma. In the brain itself, various abnormalities in areas involved in memory, the stress response and the processing of emotions have been identified. The amygdala (involved in memory and emotion processing) is overactivated (it is hyperresponsive and has a smaller volume among PTSD patients) in response to memories of traumatic events whereas the PFC is under-responsive to fearful stimuli, which may result in its failure to inhibit the amygdala and thereby inhibit traumatic memories. o Impact of trauma on the brain: o Increased secretion of cortisol Decreased size of hippocampus (negative impact on memory) o Increased amygdala function o Decreased medial prefrontal cortex function (learning, judgement) o Increase in epinephrine o Name neurotransmitters that can be dysregulated by trauma, and give examples. o Increased dopamine (modulated HPA axis responses), o increased norepinephrine (hyperarousal, heightened startle response, increased encoding of fear memories), o decreased serotonin (hypervigilance, heightened startle response, impulsivity), increased glutamate (derealization and dissociation). o If the stressor doesn’t go away, high levels of cortisol can be problematic o Alterations in the way you perceive the world and express emotions o Suppress reproductive functioning (menstrual cycle stops, infertility) o Suppress growth hormone release o Increases insulin resistance → weight gain o Inhibits bone remodeling → puts them at risk for osteoporosis Effects of Stress Most Glucocorticoid receptors in hippocampus (learning, memory) and frontal cortex (impulse control, judgment, planning, reasoning) o Atrophy (Death) in neurons of these areas – leads to emotional and behavioral responses o Depression – anterior cingulate stops making and responding to serotonin (perceive more stressors) o Anger – fight part of fight or flight – can lead to vascular disease (heart attack) o Anxiety – amygdala (fear center) flight part of fight or flight – perceive more things as fearful which increases anxiety o Addiction – drugs as coping mechanism. Impairment of frontal cortex (impaired reasoning and judgment) increases likelihood of being consumed by inappropriate coping mechanisms Coping with Stress Perceived control - lack of control is perceived threat – low SES, minority population Optimism – humor Social support – not alone in feelings, better eating, exercise, sleeping patterns Exercise – decrease chance of cardiovascular disease, increase blood to brain heart and body, increase neurogenesis (growth of new neurons), planning for daily exercise, increase size of hippocampus Meditation – lower heart rate and blood pressure, increase size of hippocampus Faith – (really more social support) Cognitive Flexibility – know what you can change and what you can’t a.k.a therapy. Mirror Neurons System Lacoboni et al. Mirror neurons echoes not only actions but also intentions; may play a significant role in our ability to infer another's state of mind based on their actions or description of events. Corradini and Antonietti (2013) noted that areas of the brain that are normally activated by one’s own emotion are also activated when one looks at the others feeling the same emotion or sensation, supporting the role of the mirror neuron in cognitively understood empathy. Wallin (2007) neural substrate for empathy, affect attunement, mentalizing and intersubjectivity Studies of mirror neurons: (Monkeys -- Rizolatti, 1996)(Humans -- Lacaboni, 2005). OFC damage or deficit is associated with difficulty in managing one’s emotions, gauging one’s impact on others, and responding appropriately to their social signals and states of mind Prolonged childhood stress can also led to deficits in oxytocin and GABA o Oxytocin is considered the “love hormone” because it allows individuals to trust others and form securely attached relationships (De Boer, et al 2012) o GABA is a NT that inhibits excitation and anxiety The stress Ms. X experienced may have altered her body’s ability to produce an adequate amount of oxytocin given that she did not receive enough love from her caregivers. o Deficiencies in oxytocin may account for inability to trust others or form securely attached relationships Further, Ms. X may also have deficiencies in GABA o Those with anxiety disorders tend to have deficiencies in GABA, making it difficult to calm down. o Because she constantly needed to be alert in the environment she lived growing up, her brain may have altered and decreased its production of GABA Depressant medications such as Xanax and Klonopin are GABA agonists, meaning that they work to increase the amount of GABA in the brain There is evidence that Ms. X experiences GABA deficits given that she is treating her symptoms with other depressants such as alcohol and uses them to relax What biological systems are implicated in regulating social relations Childhood exposure to severe stress, especially if chronic, can alter individuals’ brain and neurochemical development as well as individuals’ future responses to stressful situations. What are the most likely biological mechanisms (systems/ anatomy/interactions) by which these long-term effects are mediated? What biological changes could we expect to see as a result of his experiences of trauma and stress reactivity, and how would these physiological markers be expressed through his behavior in his relationships in and out of the consultation room? 1) Describe the biological aspects of high levels of stress, how the effect varies when stresses are repeated chronically, and the long-term effects on both brain and behavior, including the future ability to identify and manage stressful environments.