The Neurobiology of Trauma
advertisement

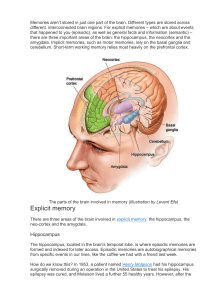
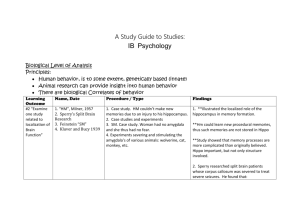
The Neurobiology of Trauma and Memory Some patients may also benefit from basic information about the differences in how normal memories are stored in the brain versus how traumatic memories are stored. See van der Kolk (1996) for a summary of the neurobiology of trauma. Normal memories are encoded primarily in the left cerebral hemisphere and in the hippocampus as coherent narratives of the experience. The hippocampus is located in the brain stem and is the indexing center for complex memories. The hippocampus also holds information about the “where” and “when” experience occurs. Trauma memories are encoded primarily in the right hemisphere as sensory memories and in the amygdala. The amygdala is the defensive center in the brain where fight, flight, and submission responses (among others) take place. Sensory threat cues (sights, sounds, body sensations, and smells) are encoded in the amygdala. The amygdala retains a database of all threat cues to allow us to respond quickly, and without thought, to danger. A breakdown in the discrimination of threat cues in trauma survivors leads to persistent, recurring overly defensive reactions and intrusions from relatively innocuous stimuli. Stress hormones secreted by the amygdala lead to inhibitions in the function of the hippocampus in trauma survivors and, if untreated, to actual shrinkage in the size of the hippocampus. The excessive activation in the amygdala tends to dampen activation in the orbital prefrontal regions of the brain, just above the eyes in the forehead, inhibiting the normal executive function of exercising thoughtful control over impulses. Thus, when memories of trauma intrude, they tend to produce a state of “speechless terror” (van der Kolk, 1996) in which they are not really “remembering”, but instead are helplessly re-experiencing their traumatic experiences. The Adaptive Information Processing (AIP) model parallels what is known about the neurobiology of how the brain moves memories of traumatic and adverse life experiences from this maladaptive, temporary storage system- sometimes referred to as implicit memory—into adaptive longterm storage in the narrative—or explicit memory system (Schacter, 1987). This reorganization and consolidation occurs during dreaming or rapid eye movement (REM) sleep. It may well be one of the mechanisms behind the effectiveness of EMDR (Stickgold, 2002, 2008). While many contemporary forms of psychotherapy rely primarily on getting the patient to consider or rehearse new thoughts, EMDR depends on stimulating the brain’s intrinsic capacity for adaptive information processing. This capacity is not driven by deliberate thought, but by deeper, intrinsic structural capacities in the brain to adapt and learn from experience. Indeed, during the periods of bilateral stimulation with eye movements, taps, or tones in EMDR reprocessing, most patients are not capable of holding specific thoughts in mind. This inability to deliberately retain images or thoughts in awareness is normal and needs to be explained to patients as part of the preparation phase to prevent patients from judging them-selves as somehow failing or not doing EMDR correctly. On the other hand, during reprocessing some patients will experience a wealth of vivid images, body sensations, emotions, associations to other memories, insights, disturbing or pleasant thoughts, and even smells. Leeds, Andrew Ph.D., (2009). A Guide to the Standard EMDR Protocols for Clinicians, Supervisors, and Consultants. Springer Publishing Company, Ch.6 (104-105).