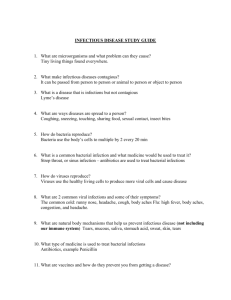
GI Drugs Class - Drug Ther. Use/ Admin MOA Adverse Reactions Precautions/Considerations Psyllium (Metamucil) and Methylcellulose(Citrucel) Bulk forming Laxatives (Group III) Soften stool and help evacuation Maintains water in stool, softening stool and increasing bulk Esophageal obstruction Internal obstruction or impaction 1-3 days to be effective Avoid in patients with narrowing intestinal lumen Contraindicated --Bowel obstruction --Undiagnosed. Abd. Pain Scopolamine Anticholinergic Blocks impulses from vestibular apparatus of inner ear and vomiting center of the brain Prevention of motion sickness Dry mouth, blurred vision, drowsiness “Cant’ pee, can’t see, can’t piss, can’t shit” Give PO, IV, SQ Use w/ caution in patients with ..... urinary retention or obstruction Asthma Narrow angle glaucoma Cimetidine (Tagamet) Histamine 2 Receptor Antagonists (H2RAs) GERD PUD Zollinger-Ellison Syndrome Block H2 receptors, lowering secretion of gastric acid ● ● ● , Gynecomastia, decreased libido, impotence ○ Caused by blocked androgen receptors Lethargy, hallucinations, confusion, restlessness, agitation ○ Crosses BBB Pneumonia ○ Decreased acid allows bacterial colonization of stomach and respiratory tract CNS effects increased w/ older adults Caution w/ pneumonia risk patients (COPD, asthma, etc.) Doses should be reduced w/ renal or liver impairment Sucralfate (Carafate) Mucosal Protectant Tx of acute duodenal ulcers and maintenance therapy Stomach acid changes sucralfate into a protective barrier that adheres to ulcers ---This paste like substance lasts for up to 6 hours Constipation No systemic effects, the drug is minimally absorbed Caution w/ diabetes and chronic kidney disease Patient Education Increase fiber and fluids Take 4x/day, 1 hr before meals and before bed Dissolve in water is needed, DO NOT chew or crush tablet Liraglutide (Saxenda) GLP-1 Agonist ONLY FDA approved injectable medication for weight loss Adjunct therapy for reduced calorie intake and increased physical activity BMI>30 or >27 with at least one weight related comorbidity Slows gastric emptying N/V/D ○ Reduced by slowly titrating the dose up HA Increased resting HR Contraindicated in patients w/ medullary thyroid cancer (MTC) 1` Drugs that Weaken the Bacterial Cell Wall Penicillins Protype: Penicillin G Potassium Give IM/IV Other PCNs can be PO Prophylaxis of bacterial endocarditis in clients with prosthetic heart valves or congenital heart disease Meningitis Destroy bacteria by weakening the bacterial cell wall Considered a beta-lactam antibiotic Allergic reactions Pain at the injection site (with IM admin) Renal impairment Neurotoxicity (seizures, confusion, hallucinations) with high blood levels Hyperkalemia with large IV doses Pneumonia Syphilis History of allergic reactions to penicillin, cephalosporins, or imipenem Use cautiously in clients who have or are at risk for kidney dysfunction (clients who are acutely ill, older adults, or young children) DO NOT MIX with aminoglycosides Cephalosporins Protype: Cephalexin (Gen 1) --Kills gram positive --Destroyed by betalactamases Gen 2 Cefaclor, Cefotetan Gen 3 Ceftriaxone, cefotaxime Gen 4 Cefepime Gen 5 Cetraroline --MRSA Ceftobiprole --MRSA,PCN resistant bacteria Infections of skin, bone, heart, blood (septicemia), respiratory tract, GI tract, and GU tract Admin Give vitamin K if… -Increased PT/INR Weakens the bacterial cell wall Beta-lactam antibiotic Allergic reaction Thrombophlebitis with IV infusion Renal insufficiency Pain with IM injection Comprise 5 generations…. --More likely to reach CSF Patient Education Complete the entire course of therapy, even --Less susceptible to destruction by beta-lactamase Take PO cephalosporins with food Store PO cephalosporin suspensions in a IV or IM b/c of decreased GI absorption; mainly eliminated by the kidneys if manifestations resolve -Allergic reaction -ETOH intolerance -Nephrotoxicity -Thrombophlebitis --More effective against gramnegative organisms and anaerobes refrigerator Precautions Dose adjustment for renal patients Hx of allergy to PCN or cephalosporins Use w/ caution in patients with bleeding tendencies o Interactions --Alcohol strong disulfiram reaction --Anticoagulantsbleed risk --Aminoglycosides --Calcium can form precipitate w/ ceftriaxone --Probenecid delays renal secretion Carbapenems Protype: Imipenem-cilastatin (Primaxin) Serious infections due to gram-positive and gram-negative cocci, anaerobic bacteria Destroy bacteria by weakening bacterial cell wall EXTREME broad spectrum antibiotic For serious infections (pneumonia, peritonitis,UTI) Most effetctive betalactam vs. anaerobes Used for patients who cannot be treated with other, more narrow antibiotics A beta-lactam antibiotic --Allergic reaction --N/V/D --Superinfection Monitor for indications of colitis (diarrhea), oral thrush, black furry overgrowth on tongue, and vaginal yeast infection MUST BE GIVEN IV!! Monobactams Protype: Aztreonam (Azactam) Serious infection caused by gram-neg Destroys bacterial cell walls NO ACTIVITY vs. gram-pos, anaerobes NOT A BETA LACTAM Contraindications/Precautions --Pregnancy Risk Category C --Use cautiously in clients who have renal impairment --History of allergic reaction to penicillins or other beta-lactams Glycopeptides Protype: Vancomycin --often given w/ aminoglycosides ONLY for gram-pos; MRSA, C. diff, PCN resistant pneumococci, S. aureus, Streptococcus infections Destroy bacterial cell wall Can be given to PCN allergic patients, not a beta lactam --Ototoxicitywatch for other ototoxic drug in combo (i.e. loop diuretics) --Nephrotoxicity --Red man’s syndrome Caused by rapid infusion of Vancomycin Rash, itching, flushing, tachycardia, hypotension, angioedema GLOBAL RXN --Thrombophlebitis --Immune related thrombocytopenia (rare) Give slowly, over 60 mins Contraindications/Precautions --Allergy to vancomycin --Use cautiously in clients who have renal impairment --Caution w/ older adults, especially with kidney or ear PMH --Monitor peak and trough, renal function, infusion times, s/s of ototoxicity Antimycobacterials Class - Drug Therapeutic Use MOA Adverse Reactions Precautions/Considerations Isoniazid (INH) Primary agent for TB Bactericidal Peripheral neuropathy (Pyridoxine vitamin B6) Hepatotoxicity CNS effects Drug Interactions: Inhibitor of several cytochrome P450 isoenzymes Increases levels of phenytoin, diazepam, carbamazepine Alcohol!! Rifampin (Rifadin) Broad spectrum Multiple uses TB, leprosy, H Flu, Legionella Others Hepatitis Discoloration of body fluids(red-orange) -Tears, urine, sweat, saliva -Can stain contact lenses Drug Interactions (several cytochrome P450 isoenzymes) Coumadin, oral contraceptives, HIV drugs nucleoside reverse transcriptase Inhibitors ) In combo with INH and Pyrazinamide = severely hepatotoxic PZA TB Bactericidal Hepatotoxicity hyperuricemia (gout) & Arthralgias GI side effects (N/V/D) General Info - - - Difficult to treat-primarily due to resistance - Drug selection and length of treatment based on susceptibility of organism and immunocompetence of host! Principle cause of resistance is inadequate drug therapy Goals of treatment o Kill actively dividing Renders sputum noninfectious o Eliminate intracellular persisters Two phases Initial (induction or intensive) phase o Eliminate actively dividing Second (continuation) phase o Eliminate those resting st 1 line treatment for active TB – RIF, INH, Pyrazinamide, Ethambutol Latent TB treatment o Preferred regimens: Rifamycin-based Rifapentine + INH; Rifampin alone; Rifampin + INH Rifapentine and Rifampin are NOT interchangeable! o Alternative regimens: INH monotherapy for 6 or 9 months Identifying barriers to adherence > directly observed therapy Bacteriostatic/Bactericidal Inhibitors Class - Drug Ther. Use/ Admin MOA Adverse Reactions Precautions/Considerations Tetracyclines Tetracycline Demeclocycline Doxycycline (Long acting lyme disease, chlamydia) Minocycline --Rickettsial diseases (lyme disease) --H. Pylori infection --Animal bites --STIs --Acne --Periodontal disease PO (preferred), topical, or IV Blocks protein synthesis Discoloration of teeth BACTERIOSTATIC Disruption of long-bone growth --Fall precautions Selective toxic—poor ability to hurt mammal cells BROAD SPECTRUM *no longer 1st line b/c of resistance Photosensitivity Short/immediate acting (tetracycline, demeclocycline.) --Monitor kidney function --Administer on empty stomach Long acting (Doxycyline, Minocin) --Monitor LFTs --Administer w/wo food PO: Incomplete swallowesophageal irritation --Take w full glass of water, keep HOB elevated, do not sleep after taking Caution w/ renal and/or liver impaired patients AVOID dairy, calcium supp., iron supp., milk of mag, antacids --Admin tetracycline by 2 hours from these products Interactions --Digoxin --Warfarin Contraindicated --Pregnancy, breast feeding --Children under 8 Macrolide Antibiotics Erythromycin --Alternate for PCN allergic patients --PO entericcoated, IV, topical Most effective vs. gram-positive -Legionella pneumophilia (Legionnaires disease) -Bordetella Pertussis (Whooping cough) - Acute diphtheria Binds to 50S ribosomal subunit, block additional amino acids from making chain GI Upset Superinfection QT prolongation -risk for ventricular tachycardia, Torsades des pointes --cardiac monitoring ---educate pt to report s/s e.g. unexplained fainting Two derivatives of the base ---Erythromycin stearate -- food decreases absorption ---Erythromycin ethyl succinate -- food does not affect absor. Azithromycin Upper resp, infection Ear infections IV over 60 mins Follow w/ PO Absoprtion ↓ w/ food Clarithromycin Immediate-release tabs or suspension CYP450 Inhibitor Use alternate contraception when taking (blocks pill) Lincosamides Clindamycin Anaerobic infections outside CNS BACTERIOSTATIC IV, IM, PO, vaginal, topical --SLOW IVcardiac C. diff associated diarrhea --Superinfection w/ c. diff --Treat w. PO vancomycin or metronidazole Education --Monitor for diarrhea --Take w/ full glass of water --Can take / meals Rapid IV administration may cause EKG Δ’s (changes), hypotension, cardiac arrest Oxazolidinones Linezolid (Zyvox) MDRO gram-positive --MRSA and VRE Binds to 50S subunit, block protein synthesis **Used as last resort to prevent development of resistance BACTERIOSTATIC PO, IV N/D, HA Neuropathy Myelosuppressionanemia, thrombocytopenia, leukopenia, etc. --Monitor CBC (Hgb, platelets, WBC) Interactions --MAOIshypertensive crisis --SSRIsserotonin syndrome Other bacteriostatic antibiotics Tigecycline (Tygacil) MDRO gram-neg and gram-pos ONLY USE WHEN OTHER ANTIBIOTICS WILL NOT BE EFFECTIVE --Using Tigecycline for severe infections is associated with ↑ mortality Dalfopristin/ Quinupristin (Synercid) Inhibit binding of tRNA to mRNA by binding to the 30S subunit to block protein synthesis BACTERIOSTATIC, broad spectrum BACTERICIDAL when in combo, bacteriostatic separate Alternate for PCN/cef allergy Chloramphenicol **Limited infections that can’t be treated w/ safe antibiotics IV, PO, topical (eye infections) BROAD SPECTRUM gram pos and gram neg Blocks protein synthesis N/V SuperinfectionC. diff associated diarrhea (CDAD) Photosensitivity --Teaching wear sunscreen when outside Pancreatitis r/t build up of toxic metabolites Disruption of long-bone synthesis Teeth discoloration Interactions --Warfarincan slow clearance MONITOR PT/INR ***Bleeding precautions w/ concurrent use Contrindications --Hx of pancreatitis --Pregnancy Hepatotoxicity --MONITOR LFTs FREQUENTLY Thrombophlebitis, with IV admin --Admin via central line --Flush before and after with dextrose, assess access site, rotate site Avoid grapefruit Reversible bone marrow suppression --Monitor CBC, neutropenic precautions --S/S weakness and fatigue Gray syndrome --Rare; newborns especially preemies Aplastic anemia --CBC Drug interactions: CYP3A4 inhibitor – e.g. immunosuppressants Aminoglycosides Gentamicin Tobramycin Neomycin Narrow spectrum Used primarily against aerobic gram bacilli E Coli (Escherichia coli) Klebsiella pneumoniae Serratia marcescens Proteus mirabilis Pseudomonas aeruginosa NO anaerobic orgs Disrupt protein synthesis at 30S subunit, eventual cell death Bactericidal No CNS, poor oral absorption, given IV or intrathecal Nephrotoxicity (BUN, creatinine, protein urea) Ototoxicity (hearing/balance difficulties, tinnitus, CN 8) Neuromuscular blockade (can mimic) -Inhibits neuromuscular transmission causing flaccid paralysis, severe resp depression -Do not give with a NM blocker, general anesthetics -treat with IV calcium gluconate Narrow therapeutic range: monitor peaks and troughs Use caution in renal dysfunction, while taking other nephro/ototoxic meds, diuretics Used in combo with Vanco/other beta-lactam antibiotics – do not run through same IV line Keep pt well hydrated, use <10 days CI pregnancy Dosing schedule may be daily or 2-3 smaller doses: levels vary widely based on age, body fat, patho, fever, edema/dehydration UTI Antibiotics and Adjuncts Class - Drug Therapeutic Use/ Admin MOA Adverse Reactions Precautions/Considerations Sulfonamides Systemic Sulfamethoxazole --Intermed. acting --Only used w/ trimethoprim Sulfadiazine --Short acting --For meningitis prophylaxis Topical Silver sulfadiazine --Burn victims, suppress bacterial colonization Sulfacetamide --Eye infections UTIs Inhibit folic acid synthesisprotein synthesis BACTERIOSTATIC BROAD SPECTRUM Hemolytic anemia --CBC monitoring Monitor for rash, immediately contact HCP if skin begins to peel Kernicterus --Rare neuro SE mostly in newborns --↑ bilirubin in brain --LFTs and bilirubin Avoid direct sunlight, wear sunscreen Crystalluria --BUN and creatinine --encourage ↑ fluids Caution w/ renal impaired patients Contraindications --Newborns < 2 months old --Pregnancy and breast feeding --Sulfa allergies Hypersens. Reactions --Photosensitivity --Steven-Johnson’s Syndrome Interactions -Warfarinbleed risk MONITOR PT/INR --Phenytoinneurotoxicity --Sulfonylureas risk of hypoglycemia Silver sulfadiazine specific --Skin discoloration **Avoid use on face Sulfacetamide specific --Blurred vision Associated w/ ↑ risk of hypersensitive reactions Other UTIs Antibiotics Trimethoprim (TMP) ONLY acute uncomplicated UTIs Inhibits protein synthesis Rash, itching (pruritus) Most common used in combo w/ sulfamethoxazole (Bactrim) BROAD SEPCTRUM GI upset Bactericidal or bacteriostatic depending on site of infection Hematologic effects --Blood dyscrasias in those with preexisting folic acid deficiency --MONITOR CBC Selective toxic, no harm to host cells --bacteria cells most sensitive, can be low dose Contraindications Folic acid deficiency Pregnancy Other meds that increase K+ levels --Loop/thiazide diuretics Hyperkalemia --MONITOR K+ LEVELS Neural tube defects, such as spina bifida --Crosses placenta -- ensure adequate folic acid intake TrimethoprimSulfamethoxazole (Bactrim) **Lower risk of resistance w/ combo UTIschronic and recurrent Pneumocystis Pneumonia (Pneumocystis jiroveci) Opportunistic fungus Otitis media Bronchitis GI-Shigellosis PO, IV Inhibits protein synthesis BROAD SPECTRUM BACTERIOSTATIC Nausea, vomiting, rash (can be mild to severe) Sulfonamide reactions Headache, hallucinations, depression Hypersensitivity reactions Stevens-Johnson’s syndrome Blood dyscrasias MONITOR CBC Kernicterus BILIRUBIN AND LFTs Renal damage BUN & CREATININE Birth defects Contraindications --Pregnancy and breast feeding --Sulfa allergies --Newborns < 2 months old Caution w/ renal impaired patients Caution w/ mental health patients and elderly due to CNS effects Interactions Same as sulfamethoxazole Fosfomycin 1st line for women w/ uncomplicated UTI caused by E. coli or enterococci Headache N/D Abd. Pain Single course PO; qualified pts --Not pregnant, uncomplicated UTI --Expected effect 2-3 days Rash Drowsy/dizzy Rhinitis Urinary Tract Antiseptics Nitrofurantoin Furadantin Macrobid Macrodantin Methenamine ONLY UTI’s b/c they do not reach high concentrations in other parts of body Prophylactic Tx recurrent UTIs ONLY for UTIs, requires acidic environment to work Mandelamine PO enteric coated no chew or crush BROAD SPECTRUM CNS efftecs BACTERIOSTATSIC at low; Bactericidal at high concentrations Caution w. renal impaired patients Prodrug that under acid conditions breaks down into ammonia and formaldehyde, denaturing bacterial proteins and causing cell death OTC Urinary Tract Analgesics Phenazopyridine Hydrochloride (AZO) UTI pain relief OTC --take 1-3 days to effect Caution w/ mental health patients and elderly b/c of CNS effects Turns urine orange Miscellaneous Antibiotics Class - Drug Therapeutic Use MOA Adverse Reactions Precautions/Considerations Fluoroquinolones Ciprofloxacin (Cipro) -Sinusitis, AOM, UTI, Pneumonia, Salmonella & Shigella infections -Topical for conjunctivitis, acute otitis externa, tympanostomy tube associated otorrhea -Drug of choice for anthrax Broad spectrum antibiotic Inhibits bacterial DNA gyrase (needed to replicate) Bactericidal Metronidazole (Flagyl) Used for protozoal infections and infections caused by obligate anaerobic bacteria -Bacteroides fragilis and C. difficile Bactericidal to anaerobic organisms only -PO,IV Rifampin TB (active and latent) Neisseria meningitides (in asymptomatic carriers) Prophylaxis of H.influenzae meningitis Other off label uses as well Broad spectrum High risk of resistance Given: IV, PO, Topical (eye drops, ear drops) N/V/D, HA, CNS, candida pharynx and vagina, photosensitivity, Risk for C.diff Serious AE: Prolong QT, weakness in MG patients, permanent peripheral neuropathy, tendon rupture, aortic dissection, disturbances in attention, disorientation, agitation, nervousness, memory impairment, and delirium, severe hypoglycemia > coma -DC at first sign of tendon pain or inflammation, do not give to children under 18 -Absorption decreased by milk, calcium, Al, Mg, Fe ,Zn, Carafate -CYP450 inhibitor: monitor dose of Warfarin, Theophylline Lowers seizure threshold GI HA, dizziness Red-brown urine Metallic taste Thrombophlebitis with IV use Disulfiram-like reaction with concomitant alcohol Stevens Johnson Syndrome Crosses placenta and BBB Avoid in 1st trimester; cautious use in 2nd & 3rd, Breastfeeding Liver metabolism—unknown if via CYP450 -Warfarin, lithium, phenytoin, others— levels increased so monitor -Ketoconazole (antifungal) —increases metronidazole levels Antifungal Agents Class - Drug Therapeutic Use MOA Adverse Reactions Precautions/Considerations Polyene Antibiotics Amphotericin Amphoterrible – think TOXIC -Toxic to kidneys and liver -Observe H/H, LFTs, electrolytes, renal labs -Xamine for multiple organ failure -Interactions -Cardiac failure Nystatin Broad spectrum – fungal infections Drug of choice for most systemic mycoses Reserved for potentially fatal infections Candidiasis Binds with ergosterol, a component of fungal cell membrane, to cause fungal death Infusion Reaction – fever, chills, rigor, HA - Pre-treat w Diphenhydramine and Tylenol Kills fungus but binds to cholesterol in humans-> AE Nephrotoxic – monitor BUN, creatinine, GFR HIGHLY TOXIC IV only – systemic Hypokalemia – damage kidneys, monitor K+ All pts will experience infusion reaction and renal damage to varying degrees Hematological Effects – bone marrow suppression>anemia, monitor H&H, CBC Rigor antidote = Dantrolene Phlebitis – use large central vein, change peripheral sites often, monitor IV, administer slowly over 2-4 hours Avoid other nephrotoxic drugs like NSAIDS, aminoglycosides Intrathecal Swish and swallow for oral, use oral rehydrator brush if pt NPO PO, topical Use after eating, not before Use powder if area is moist – use cream if skin is really irritated to calm/cool it Azoles Ketoconazole Broad spectrum Systemic and superficial mycoses Lower toxicity, can be given PO Griseofulvin Treats dermatophytic infections Deposited in the keratin precursor cells of skin, hair and nails – newly formed keritin is resistant to fungal invasion/infection N/V/D Hepatotoxicity Inhibit CYP450: Quinidine, cyclosporine, digoxin, warfarin, & sulfonylureas Cardiac suppression (neg inotrope) Caution in HF patients Hepatotoxicity – check underlying liver failure Take orally with fatty foods to increase -O-Fulvin” Pyrimidine Analogs Flucytosine Used in combination with Amphotericin B to treat severe systemic mycosis (prevent resistance) Hepatotoxicity Bone marrow depression Concentration dependent Parasitic Meds Class - Drug Therapeutic Use MOA Adverse Reactions Precautions/Considerations Metronidazole Amebiasis, Giardiasis, Trichomoniasis (STD), commonly prescribed after GI surgery Works by entering anaerobic bacteria and inhibiting its DNA synthesis, causing bacterial cell death Causes Disulfiram-like reaction (flushing, severe nausea & vomiting) when taken with Alcohol For STDs - treat all sex partners PO or IV Nausea, HA, dark urine, metallic taste, neurological effects (rare) Hypersensitivity risk (SJS) Mebendazole Enterobiasis (pinworm) Crosses placenta and BBB – avoid in 1st trimester, caution in 2nd and 3rd Breastfeeding OK 12-24 hrs after dose Increases warfarin, phenytoin, lithium levels – monitor for toxicity Spreads easily – treat whole family ---Educate on hang hygiene