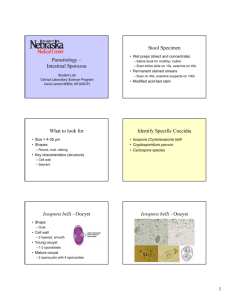
CLASS- ZOOMASTIGOPHERA • The parasites belonging to this group of protozoa possess one or more flagella giving them the power of motility. FLAGELLATES • These are classified according to their habitat into TWO groups: 1.Intestinal,oral & genital flagellates. 2.Blood & tissue flagllates. Giardiasis Giardia intestinalis =(lamblia) Class Zoomastigophorea Order Diplomonadida Family Hexamitidae – Giardia lamblia (intestinalis, duodenalis) humans, mammals – Giardia muris - mammals – Giardia ardeae - birds – Giardia psittaci - birds – Giardia agilis - amphibians Habitat • Duodenum and the upper part of the jejunum of the man. Morphology • Exits in two phases: A) Trophozoite B) Cyst TROPHOZITE • When viewed flat,the shape of the trophozoite is like that of badminton racket. • The dorsal surface is convex & the ventral surface is concave like a sucking disc. • The size of the trophpzoite is 14 micrometer long & 7 micrometer broad. • All organs of the body are paired. • There are 2 axostyles,2 nuclei and 4 pairs of flagella. CYST • It is oval in shape and measures 12 micrometer long and 7 micrometers in breadth. Giardia intestinalis Epidemiology Presumed to be zoonotic, but new evidence indicates that strains may be species specific. Host can be humans, primates, cats, dogs, calves, beavers, rabbits, etc. World wide distribution Highest incidence in children, young adults in late summer. Transmission Person to person transmission Water sports, surface contamination, watershed contamination Sexually active male homosexuals and persons in custodial institutions. PATHOGENICITY • With the help of the sucking disc the parasites attach itself on the epithelial cells of the intestine and may cause disturbance, leading to malabsorption of fat. • The patient may complain of persistent looseness of bowels , and mild steatorrhoea. Pathogenesis and Immune response •The production of diarrhea, and occasionally malabsorption, is the result of a complex interaction of Giardia with the host, •Infection occurs after oral ingestion of as few as 10 to 25 cysts. •After excystation, trophozoites colonize and multiply in the upper small bowel •Adherence of G. lamblia in the human gut may be via the disk, but may also involve specific receptor-ligand interactions Pathogenesis and Immune response Several pathogenic mechanisms have been postulated •Disruption of the brush border •Mucosal invasion •Elaboration of an enterotoxin •Stimulation of an inflammatory infiltration leading to fluid and electrolyte secretion and occasionally to villous changes Source: Gallery of histology Woods and Ellis2000 Giardia Lamblia clinging to the wall of a duodenal villus. Immune Response Partially protective immunity may develop to Giardia Immune response involves both cellular and humoral immunity Ig A, serum Ig G and Ig M are detected in patients: Role of Ig A is not completely understood, probably inhibits trophozoite attachment IgA deficiency lead to chronic giardiasis Cell mediated immune response may also play a role Human milk may also play a role in protection of the host against Giardia : Free fatty acids and IgA antibodies Infection with G. lamblia includes •Asymptomatic cyst passage (5 to 15% ) •Acute self-limited diarrhea (25 to 50% ) •Chronic syndrome of diarrhea, malabsorption and weight loss Symptomatic giardiasis is characterized by (Travelers Diarrhea) •Acute onset of diarrhea •Abdominal cramps, bloating, and flatulence •Malaise, nausea, and anorexia •May complain of sulfuric belching •Vomiting, fever, and tenesmus occur less commonly. •Stools may be profuse and watery, but later they are commonly greasy, and foul-smelling. Diagnosis • Giardia should be identified 50 to 70% of the time after one stool, and 90% identification after three stools • Wet, saline mounts: falling leaf motion, fibrils present, and nucleic characteristics. • Biopsy tissue/duodenal aspirate /Enterotest stained by trichrome or Giemsa stain. • Enzyme immunoassay and fluorescent monoclonal antibody antigen detection systems • Sensitivity & specificity: 90-100% ( ProSpec T, GiardEIA, MeriFluor, Color Vue, and DD System) Drug Adult Pediatric Metronidazole 250mgtidX 5-7 d 5mg/kg/tid x 7 d Quinacrine 100mgtidX5-7d 2mg/kg tidX7d Furazolidone 100 mg qid × 7–10 d 2 mg/kg qid × 10 Paromomycin 25–30 mg/kg/d in 3 doses × 5–10 d Tinidazole 2 g × 1 dose PREVENTION The prevention of giardiasis requires proper handling and treatment of water Good personal hygiene on an individual basis Chlorination alone is sufficient to kill G. lamblia cysts, important variables, such as water temperature, clarity, pH, and contact time, alter the efficacy of chlorine, and higher chlorine levels (4 to 6 mg/liter) may be required. Bringing water to a boil is sufficient to kill all protozoal cysts; at high altitudes, boiling for longer periods may be necessary Cryptosporidium, Cyclospora, and Isospora •Secretory diarrhea without RBC or WBC in the stool. •None are easily found in routine “stool for ova and parasites.” •Modified acid-fast staining is useful for all of the Coccidians. Isospora belli Cyclospora Cryptosporidium COCCIDIA Thick-walled oocysts excreted in feces In Humans • Cryptosporidium • Cyclospora • Isospora • Sarcocystis • Toxoplasma Classification • Kingdom : Animalia • Sub kingdom : Protozoa • Phylum : Apicomplexa • Class : Sporozoa • Sub class : Coccidia • Order : Eucoccidia • Sub order : Eimeriidae • Family: Eimeriidae Cryptosporidium parvum History : • Tyzzer -1907 1st reported by in gastric crypts of laboratory mouse • 1971-C.parvum as pathogenic causing micro organism. • 1976-1st case of human infection of diarrhea • 1993-Massive outbreak of cryptosporidiosis in Milkwaukee affected 4,00,000 people Species of Cryptosporidium C. parvum C. hominis (previously C. parvum genotype 1) C. canis, C. felis, C. muris Habitat of C.parvum • In the form of trophozoite. • It is present in the intestinal epithelial cell. • Remaining just within brush border. MORPHOLOGY TROPHOZOITE OOCYST THICK WALLED THIN WALLED Trophozoite • Measures 1micro meter in diameter. • They are found on brush border (micro villous surface) of small intestine. • They grow into schizonts. OOCYST These oocyts are either: • 1.Thickwalled-80% passed in feces THICKWALLED OOCYST • 2. Thin walled -20% excyst endogenously causing internal autoinfection • Oocyst contain 4 sporozoites. NO SPOROCYSTS PRESENT • Size - 4-5µm THIN WALLED OOCYST Modes of infection Reservoir host- Live stock, cats, dogs, birds etc. Portal of entry- occurs by ingestion of oocysts usually with • contaminated water • fecal-oral and • anal oral transmission from person to person Susceptibility- Veterinary personnel animal handlers are at high risk Transmission • The 50% infective dose (ID50) of C. parvum is only 132 oocysts for healthy persons with no previous serological immunity to cryptosporidiosis • Outbreaks result from drinking water of surface water sources -lakes and rivers . • Swimming pools and water park wave pools • Also, untreated groundwater or well water public drinking water supplies. • The highly environmentally resistant cyst of C. parvum survive various drinking water filtrations and chemical treatments such as chlorination. • Food can be contaminated by either an infected person or an asymptomatic carrier . The oocysts do not survive cooking, but food contamination can occur Person-person transmission • Day-care centers, where infants or younger children are clustered within classrooms, share toilets and common play areas • Day-care employees through careless diaper-changing or through washing the laundry of infected children. • Nosocomial settings • Aerosol infection is fairly likely, since Cryptosporidium oocysts are shed in large numbers during acute infection and are immediately infective to others Persons most likely to be infected by Cryptosporidium are: • Infants and younger children in day-care centers • Those whose drinking water is unfiltered and untreated • Involved in farming practices such as lambing, calving, and muck-spreading • Engaging in sexual practices that brings a person into oral contact with feces of an infected individual • Patients in a nosocomial setting with other infected patients or health-care employees • Veterinarians who come in contact with farm animals • Travelers to areas with untreated water • Living in densely populated urban areas • Owners of infected household pets (rare) MONOXENOUS LIFE CYCLE OF C.parvum 1)INTRA CELLULAR 2)EXTRA CYTOPLASMIC 3)PRESENT IN PARASITOPHOROUS VACUOLE Life cycle of C.parvum(monoxenous) Modes of infection LIFE CYCLE Large reservoir of wild animals and livestock(Cattles, rodents, puppies, kittens) Life cycle is completed within a single host Lacks host specificity-Capable of infecting many different mammalian species Zoonotic- from animals to humans Life Cycle Complex -sexual and asexual cycles, and distinct developmental stages Excystation of the ingested oocyst in the small bowel with release of the four sporozoites Invasion of intestinal epithelial cells via apical end of the sporozoite within a vacuole formed of both host and parasite membranes and the initiation of the asexual intracellular multiplication stage (parasitophorous vacuole) Differentiation of microgametes and macrogametes Fertilization - sexual replication Development of oocysts Formation of sporozoites within the oocyst, which is then excreted in the stool The cycle begins anew when these oocysts are ingested by a new host. Pathogenesis • Sporozoite-specific lectin adherence factor has been identified • After sporozoite attachment, epithelial mucosa cells release cytokines that activate resident phagocytes . These activated cells release soluble factors that increase intestinal secretion of water and chloride and also inhibit absorption. They act on various substrates, including enteric nerves and on the epithelial cells themselves 1. Cell death is a direct result of parasite invasion, multiplication, and extrusion 2. Cell damage could occur through T cell-mediated inflammation, producing villus atrophy and crypt hyperplasia 3. Either model produces distortion of villus architecture and is accompanied by nutrient malabsorption and diarrhea Clinical manifestations in immunocompetent The incubation period - Two days - week. In immunocompetent patients, it is an acute, yet self-limiting diarrheal illness (1-2 week duration), and symptoms include : • Frequent, watery diarrhea • Nausea • Vomiting • Abdominal cramps • Low-grade fever Immunocompromised persons CD4 counts of <200 cell/cubic mm The illness is much more severe Debilitating, cholera-like diarrhea (up to 20 liters/day) • Severe abdominal cramps • Malaise • Low-grade fever • Weight loss • Anorexia Detection and Diagnosis • Stool Conc. Technique: Sheather’s sugar solution in Zn SO4 Saturated Nacl ): Formalin ether conc. Formalin ethyl acetate • By a biopsy of intestinal tissue . -"patchy" nature of parasitic infection • The modified acid-fast stain is traditionally used to detect –oocysts(4.2-5.4 um) have sporozoites (dd from Cyclospora-larger and unsporulated) Cryptosporidium • 4-5 mm oocysts • 4 sporozoites • no sporocysts Cyclospora • 8-10 mm oocyts • 2 sporocysts • 2 sporozoites each Isospora belli • 30 x 12 mm oocyts • 2 sporocysts • 4 sporozoites each OTHER DIAGNOSTIC METHODS • Anti-cryptosporidial IgM, IgG, and IgA can be detected by ELISA or by the antibody immunofluorescence assay (IFA), but neither of these assays can provide a direct diagnosis of cryptosporidiosis. • Recently, new genetic methods of detecting C. parvum have been developed, using PCR or other DNA-based detection methods. TREATMENT Since cryptosporidiosis is a self-limiting illness in immunocompetent individuals, general, supportive care is the only treatment for the illness. Oral or intravenous rehydration and replacement of electrolytes may be necessary for particularly voluminous, watery diarrhea. Antibiotics such as spiramycin and dicalzuril sodium have produced partial responses in patients. However, one particular antimicrobial agent, paromomycin, has shown promise Cyclospora cayetenisis • Cyclospora is associated with diarrhea. • 1990- virtually unknown before about • 1996 -Contaminated Guatemalan raspberry, cause of a United States outbreak of Cyclospora in. • “yuppie disease” . MORPHOLOGY • OOCYST DEFINATIVE HOST – REPTILES,BIRDS, HUMAN BEINGS • 8-10micro meter in diameter • Contains 2 sporocysts each containing 2 sporozoites • Sporozoite contain membrane bound nucleus and micronemes Gametogony Oocyst Sporozoites penetrate epithelium Producing merozoites Invade other epithelial cell Excystation In small intestine Unsporulated Oocyst Passed in feces 7-13 days mature oocyst(4sporozoites) Human Infection Through Water(oocyst) Modes of infection • Ingestion of contaminated food with sporulated oocyst. • Contaminated water • Contaminated raspberries. • Contaminated basil leaves. Clinical disease • Acute infective diarrhea • Incubation period: 2 to 11 days Immuno competant individual: 1)Rapid onset of watery diarrhea 7 to 8 stools per day 2)Nausea,anorexia,abdominal cramps 3)Low grade fever and malaise 4)Self limiting remission in 3-4 days followed by relapses from 4-7 weeks Immuno compromised individual 1)Diarrhea is prolonged 8-7 weeks and severe. 2)Biliary diseases have been reported lab diagnosis Light microscopy Auto florescence Concentration methods Normal light miscroscopy. Three mature, living oocysts sporozoites (sp) sporocystic residuum(sr) Stieda body (st). Bar = 10 µm. Direct wet preparation with no staining (x1650). • The outer wall is distinct and thick. • Each body contains several refractive granules. • 2 sporocysts in one oocyst Cyclospora cyst taking zeihl neelson staining AUTO FLUORESCENCE • Cyclospora organism flouresce when examined with an UV flourescent microscope. • This factor should be taken into consideration SEE WHETHER THE RASPBERRY ARE NOT CONTAMINATED BEFORE YOU EAT SEE THAT THE WATER IS NOT CONTAMINATED Isosopora belli • Apicomplexa • Coccidia • Monoxenous life cycle. • Coccida parasites are identified based on the structure of the oocyst. •Sporulated oocyst is the infective stage •Invades intestinal epithelial cells •Often asymptomatic •Symptoms mild gastro-intestinal distress to severe dysentery •Often self-limiting, but can become chronic •Symptoms more severe in AIDS patients • • • • HABITAT: Inside human beings. In form of trophozoites. Resides in epithelial cell of small Intestine Here schizogony and sporogony occurs Morphology • OOCYST 2 types: Immature oocyst Mature oocyst DEFINATIVE HOST – HUMAN BEINGS Immature oocyst: • Size- 15µm× 20µm • Shape – rugby ball • Develop inside epithelial cell of small intestine. • Central individual mass of protoplasm. • They are unsporulated. • They are shed in feces Immature oocyst Mature oocyst • • • Mature oocyst Size – 20µm × 10µm Shape- rugby shape It is elongated and narrow at one pole with neck like restricted area. 2 sporocyst with 4 sporozoites each Modes of infection • Reservoir host: NIL • Source : contaminated food and water. • Portal of entry: ingestion of oocyst Infection by Oocyst Gametogony, Fertilisation oocyst Merozoites Undergo Schizogony In epithelial cell Sporocyst Invade epithelium Of small intestine-trophozoite Trophozoite Undergo schizogony ISOSPORA BELLI LIFE CYCLE Clinical disease • Acute infective diarrhea • Incubation period: 2 to 11 days immunocompetant individual: 1) Rapid onset of watery diarrhea 7 to 8 stools per day 2) Nausea,anorexia,abdominal cramps 3) Low grade fever and malaise 4) Self limiting remission in 3-4 days followed by relapses from 4-7 weeks Immuno compromised individual 1)Diarrhea is prolonged 8-7 weeks and severe. 2)Biliary diseases have been reported LAB DIAGNOSIS DIRECT MICROSCOPY (FAECES) DUODENAL ASPIRATE BIOPSY Diagnosis-Mod acid fast staining Autofluorescence Biopsy of Intestinal mucosa PCR 20-33 um x 10-19 um PREVENTION Wash food such as green salads and fruits, especially if it is to be eaten uncooked. WASH YOUR HANDS BEFORE YOU EAT YOUR FOOD Eat meat only when it is cooked to "well done". For example, do not eat meat tartare or "rare" meat.