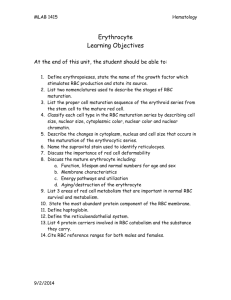
Red blood cells transport O2 to other cells and don’t use any O2 themselves for cellular metabolism, pick up O2 is to deliver to tissues, RBC do pick up a little bit of CO2 65% of Hb that is made while there is still a nucleus in place 35% of Hb is being made in the RBC without a nucleus (younger newer cells don’t have as much Hb as the mature RBC) Hb concentration per unit volume of whole blood12-16g per deciliter is normal at sea level 2x10^11 new and 2x10^11 are exciting due to old age this is to maintain steady state (majority of RBC are being reutilized/recycled) RBC are bag of Hb Few enzymes for glycolysis Using glucose for energy only through glycolysis in the production of lactate acid, this is why RBC are not using O2 for energy Has ability to go through space a min diameter of 3.5um (half the RBC size) Has to be able to deform if the fluidity of RBC is correct FE in Hb in reduce state ferrous form +2 so O2 can attach Ferric +3 cannot pick up O2 Has little repair mechanism but yet can last 120 days RBC Membrane LIPIDS Lipids are important Phospholipids = phosphor side (water loving) lipid side (long change of carbon no reason to interact with water) Cholesterol to adjust the spacing RBC very critical in being able to last 120 days Protein on outer surface that act as receptors, when the ligand hooks up to the receptor it will change the cell membrane that allows a change in the cytoplasm. Peripheral proteins-cytoskeletal support: Spectrin, Actin, Ankyrin, Band 4.2, Band 4.1 (inner part of membrane) allows for the deformability, the structural to be altered without being damaged. If a patient doesn’t have the ability to deform their RBC then it can’t make it through small spaces and get stuck, so beyond where the RBC is stuck is not going to get delivered O2 and cause CELL DEATH If there is a problem of the outer part of the membrane (ends up being bigger) spikes outside the membrane Wont last 120 days If problem with inner membrane than you get a stomatocyte (lost biconcave disk) won’t last 120 days Structural Integrity (must have proteins to allow for deformity to occur) Stay fluid/ability to deform RBC become elongated so the fluidity of Hb can squeeze through as the RBC is deforming (this is why RBC cannot be completely filled with Hb) RBC has more surface area 1. Critical thing is the RBC membrane 2. Cell surface area to volume (less material inside compared to surface volume 3. Cytoplasmic viscosity (has to be fluid) Hb is the major protein in RBC that Hb has to be fluid, so if anything changes in the protein component of Hb, so if certain amino acids change Hb may not be stable Hb could precipitate in the cell (and eventually make it to the cell membrane and when it goes through the spleen, the spleen will get rid of it creating less membrane aka shorten the life span of RBC), it could change the viscosity inside the cell (meaning it doesn’t matter how pliable that membrane is, it’s not going to make it through) Energy mechanism Once the nucleus comes out of RBC and finished with ribosomes, it goes away, no mitochondria (where does RBC get energy from? Glucose in plasma being able to go into the cell and strictly the breakdown of glucose for energy) If there is excess glucose in plasma it will get into the RBC and attach to Hb and stay attach as long as that RBC is alive, a person who is diabetic A1c will still show high levels of glucose in blood ATP is going to be used mostly in the formation in keeping that RBC membrane in proper form other energy need doesn’t have to keep that Hb (FE) in the reduce state and subject to oxidated stress all over and yet the FE remains in +2 state Thinking about Anemia Is there something wrong with the membrane? Is there something wrong with Hb in the RBC, is it not made right? Did we lose surface area of the RBC, did we lose some of it in the spleen (but that doesn’t mean we haven’t lost any Hb)? Needed for Erythropoiesis (Problem with these will cause an ANEMIA) • Metals = Fe, Mn, Cobalt • Vitamins =B12, Folate (important), C, E, B6 • Amino Acids = for Hb formation • Hormones Erythropoietin/EPO comes from kidneys goes to bone marrow and tells it we need RBC to be made. Is not an lineage cytokine it is a hormone (doesn’t work at stem cell level does not drive stem cell to become RBC) it will speed up maturation once the cell has been committed and can help put Hb faster to get them out of bone marrow early. Stimulated proliferation Stimulated RNA synthesis Release RBC earlier If a patient is having a problem with the kidneys, they will have a problem with EPO production and will be anemic Androgens can stimulate EPO being release Males have higher Hb than females Thyroxine is involved in overall cellular metabolism If patient is hypothyroid (not having as much cellular metabolism, there’s not demand for O2 there won’t be a need for making RBC) • Growth Factors/Cytokines (Bone marrow stroma that help with maturation of stem cells to erythroid side to make RBC) Hb molecule is made up of 4 protein chains it has 4 Fes attach and has to be exposed to O2 to be able to attach to O2 1,3 BPG help with 3D of Hb allows for rearrangement of itself and either allow O2 to attach or prevent O2 from coming off until its need. You want Hb in form that can have the attachment of O2 in the lung and you want that Hb to take it to the tissues and deliver O2 If there is a problem with the membrane it will change the osmotic gradient in those cells, (if there is DECREASED ATP production those cells are going to become fragile) you don’t have membrane to maintain its shape and deform. NOT MADE BY MITOCHONDRIA! It is done by Glycolytic pathway Cations RBC vs PLASMA Na (Sodium) plasma, Ca (Calcium) higher concentration in plasma K (potassium) RBC, Ca little in RBC, Mg (Magnesium) much more in RBC If there is any changes in ATP formation, if the patient is having problems with a particular enzyme in the pathway of glycolysis they will end up having an anemia amongst other things. Hexose Monophosphate Shunt (HMP) A shunt off of glycolysis (glycolytic pathway), your reducing glutathione which is going to help keep the FE IN A REDUCE STATE to transport oxygen, it’s a way to pick anything that will oxidize that FE and take care of it so that the Fe can be in the reduced state, If there is a problem with HMP in particular G6PD it will cause an anemia Fetus (ONTOGENY of hemoglobin) The Hb in RBC is different than MOM Hb because in order to get O2 its going to have a stronger affinity for O2 than moms Hbs, the fetus will want to take it from mom blood to be able to utilize it for energy once it gets a certain size Embryonic Hb is not the same structure as Adult Hb The protein chains are different the FE isn’t different The structure allows for the Hb to have a higher O2 affinity Adult Hb do include fetal Hb, there is a switching (proteins on the DNA RNA to algin amino acids there has to be switching at DNA of chain to make it more of O2 affinity than adult Hb NO KNOWN REASON WHAT CAUSES THE SWTICHING, we know its by gestational age, if the baby is a premature (born early) they will have much more fetal Hb than adult and they will have it longer because they came out early. It’s a time frame situation. THE SWITCH ISNT COMPLETE In adult Hb if one of the chains can’t be made right because there has been an amino acid substitution, if there a way to switch back to fetal Hb? As an adult do we have both fetal and adult Hb? HEMOGLOBIN Non protein component = Heme Protein = Globin Protein chains Alpha chain is going to be very critical because that is making up all of the adult Hb Zeta after embryonic stops as alpha chain takes over Genes are located on CHROMOSOME 11 and 16 Chromosome 16 zeta chain =embryonic equivalent of alpha chain Alpha chain has 2 different locations (loci) for making alpha chain, tightly conserved (ALPHA CHAIN LESS EXPRESSED) Chromosome 11 (alpha will hook up to one of these to form Hb) Epsilon = embryonic Gamma 2 different species of gamma chain Delta and Beta (MORE EXPRESSED) 4 polypeptide chains that make up Hb 4 subunits each part, has protein chain (involves DNA RNA, lining of amino acids and non-protein = heme (formed all amongst the mitochondria of the developing RBC, 1st step of heme synthesis that regulates the whole process) Alpha gene is duplicated Hb have to have EQUAL AMOUNT of alpha and beta to form Hb molecule If there is anything wrong at the DNA level it will potentially affect transcription, or it could be transcribed but the cleaning up of it will be a problem which will affect translation. Globin synthesis (protein chains are being made at the ribosome) at the same time heme is being made in and out of the mitochondria it has to be able to hook up heme gets inserted into poly peptide chains and with FE in them ready to accessible of oxygen 4 o2 per heme molecule 3 types that can transport oxygen 98-99% of adult Hb is 2 alpha and 2 beta HbA 2 alpha 2 beta and each chain have Heme component non protein component Alpha 1 Beta 1 together and Alpha 2 and Beta 2 together HbF 2 alpha chains 2 gamma chains <1% of the adult Hb but there is still some there Hb 2 2 alpha chains and 2 delta chains 2% Last step of heme formation is the addition of Fe into that molecule The rate limiting step for Hb synthesis is the 1st step in heme formation is the regulatory step in Hb formation that is what is going to be telling DNA what amino acids have to be lined up The Hb part is DNA RNA RIBOSOMES lining up amino acid Heme synthesis is a series of steps 1. Condensation of glycine and CoA ( rate limiting step) BOTH THE PROTEIN AND THE HEME IS CONTROLED BY THIS STEP if this isn’t happening DNA will not code for the protein if the synthesis continues in the cytoplasm the final step is the corporation of iron in non-protein component, heme leaves mitochondria and combines with globin chains LAST STAGE IS INCORPORTAION OF IRON If there is a problem along this way of making heme, there will be a backup of intermediaries or in the case of not enough iron it will SLOW IT DOWN if there is no Iron to incorporate, IRON DEFICIENCY ANEMIA THERES NO EXCESS CHAINS IN RBC BECAUSE 1ST STEP HAS BEEN SLOWED DOWN AND THE PROTEIN PART IS ALSO SLOWED DOWN BECAUSE OF THAT BEING THE RATE LIMITING STEP, there’s nothing extra if there is no Iron PROFORREA? Central cavity allows for the dispersment