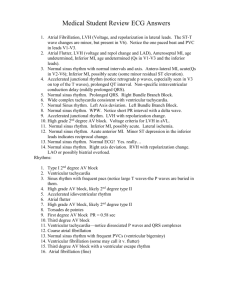
APPROACH TO ACLS RHYTHMS Dr. Jill Irene Capistrano-Sun Dr. Miriam Roxas Timonera Advanced Cardiac Life Support • Basic Life Support (BLS) • Efficient use of Skills and equipment in maintaining circulation and ventilation • ECG monitoring and Arrythmia recognition • Intravenous access and drug administration • Emergency therapies for respiratory, cardiac and post-cardiac arrest • Acute coronary syndrome and stroke management Advanced Cardiac Life Support BLS Equipment and Techniques Ethical considerations First Aid ACLS ACS and stroke management ECG and Arrythmia recognition IV Drug administration Emergency Therapies Background: CARDIAC SYSTOLE & DIASTOLE 1-Atrial diastole 4-ventricular systole 2-Atrial systole Atria relax and fill with blood Ventricles contract And force blood Out of heart 3-Ventricular diastole Atria contract and force blood into ventricles Ventricles relax and fill with blood Anatomy and Physiology Of cardiac conduction LA RA LV RV Anatomy and Physiology Of cardiac conduction Sinoatrial Node (SA Node) 60-100 bpm Bundle of His (40-60 bpm) Atrioventricular Node (AV Node) 40-60 bpm Bundle branches Purkinje fibers (20-40 bpm) Review Impulse Formation In SA Node Atrial Depolarization Delay At AV Node Conduction Through Bundle Branches Conduction Through Purkinje Fibers Ventricular Depolarization Plateau Phase of Repolarization Final Rapid Repolarization Basic ECG information .08 – 0.10 sec 0.12 – 0.20 sec 0.40 – 0.43 sec Basic ECG information 1.Rate 2.Intervals 3.Rhythm 1. Rate Different ways to calculate a rate: a) Locate a QRS that is close to a big line and count to next big line: 300, 150, 100, 75, 60, 50 1 small box = .04 sec 1 small square = 5 small boxes or 0.2 sec 60 sec/ 0.2 sec = 300 /min 1 big line: 60 sec/ 0.2 sec = 300/min 2 big lines: 60 sec/ 0.4 sec = 150/min 3 big lines: 60 sec/0.6 sec = 100/min 4 big lines: 60 sec/0.8 sec = 75/min Computation of Rate 1,500 = rate # of small squares 3 big boxes = 15 small squares 1500 / 15 small squares = 100/min 5 big boxes = 25 small squares 1500 / 25 small squares = 60/min How many QRS in 3 big boxes ? 1500 / 15 small squares = 100/min How many QRS in 5 big boxes ? 1500 / 25 small squares = 60/min 1. Rate Different ways to calculate a rate: a) Locate a QRS that is close to a big line and count to next big line: 300, 150, 100, 75, 60, 50 How many QRS in 5 big boxes ? How many QRS in 3 big boxes ? How many QRS complexes in this 6 second strip? 11 X 10 = 110 /min Rate using 6 second strip b) take a 6 second strip, count number of QRS complexes and multiply by 10 1 2 3 4 5 6 7 8 9 10 11 How many QRS complexes in this 6 second strip? 1 minute = 60 seconds = 60 secs/ 6 secs = 10 11 X 10 = 110 /min 2. Intervals We assess intervals to see where the impulse is coming from (pacemaker beat) Remember: PR interval: normal is 0.12 - 0.2 QRS interval: normal is less than or equal to 0.12 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia Atrial fibrillation Atrial flutter Supraventricular tachycardia First degree AV block Second degree AV block Third degree AV block Escape Rhythms: Junctional Rhythm Idioventricular Rhythm Ventricular fibrillation Ventricular tachycardia Asystole Causes of Cardiac Arrhythmias • Disturbances in automaticity • Disturbances in conduction • Combinations of altered automaticity and conduction Firing TACHYARRHYTHMIAS Firing Automaticity of SA Node Abnormal Automaticity and Triggered Activity Re-entry Physiologic Altered Impulse Formation Altered Impulse Conduction Pathologic Conduction Blocks Automaticity of SA Node Firing BRADYARRHYTHMIAS Firing Mechanism of Arrhythmia Development BRADYARRHYTHMIAS ABNORMALITY MECHANISM EXAMPLES Altered Impulse Formation automaticity Phase 4 depolarization (e.g.cholinergic stimulation) Sinus Bradycardia Altered Impulse Conduction Conduction blocks Ischemic, anatomic or drug-induced impaired conduction 1st , 2nd, 3rd degree AV Block Mechanism of Arrhythmia Development TACHYARRHYTHMIAS ALTERED IMPULSE FORMATION •Enhanced automaticity •Increased phase 4 depolarization •Sinus node (e.g., sympathetic stimulation) •Acquired phase 4 depolarization •Ectopic focus •Triggered activity •Prolonged action potential •Early afterdepolarization (tissue damage or drug-induced) •Intracellular calcium overload •Delayed afterdepolarization (e.g., digitalis toxicity) ALTERED IMPULSE CONDUCTION •Reentry •Unidirectional block + slowed retrograde conduction •Sinus tachycardia •Ectopic atrial tachycardia •Torsade de pointes •PAC,PVC, digitalisinduced SVT •Paroxysmal SVT, atrial flutter/fibrillation, Vent. tachycardia/fibrillation 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia (Normal) Sinus Rhythm • 60-100 bpm • P preceding each QRS • Normal intervals ..\..\Basic Rhythm Edited\1.avi Other Sinus Rhythms • Sinus bradycardia ..\..\Basic Rhythm Edited\29.avi – a sinus rhythm with a rate <60 bpm Other Sinus Rhythms • Sinus tachycardia ..\..\Basic Rhythm Edited\28.avi – a sinus rhythm with a rate >100 bpm 2. Rhythm What’s the rhythm? A) Normal Sinus Rhythm B) Sinus bradycardia C) Sinus tachycardia 2. Rhythm What’s the rhythm? A) Normal Sinus Rhythm B) Sinus bradycardia C) Sinus tachycardia What’s the HR? 5 x 10 = 50/min 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia Atrial fibrillation Atrial flutter Supraventricular tachycardia SUPRAVENTRICULAR TACHYCARDIA Narrow complex tachycardia SUPRAVENTRICULAR TACHYCARDIA • • • • • • Atrial Fibrillation Atrial Flutter Paroxysmal SVT (PSVT) Non paroxysmal atrial tachycardia Multifocal atrial tachycardia (MAT) Junctional tachycardia Supraventricular Arrhythmias • IRREGULAR RHYTHM • • • • Atrial fibrillation Atrial flutter with varying AV conduction Wandering atrial pacemaker Multifocal atrial tachycardia • REGULAR RHYTHM • • • • • • Sinus Tachycardia Atrial tachycardia Junctional/atrioventricular rhythm Atrial flutter with fixed AV conduction AV nodal reentrant tachycardia AV reentrant tachycardia Atrial Arrhythmias • ATRIAL FIBRILLATION (A-fib) – irregular rate – no discernable P waves – increased risk of strokes due to clots that might form due to fibrillation (patients are usually on anticoagulation therapy) Atrial Fibrillation • Results from multiple areas of re-entry with in the atria from multiple ectopic foci • Atrial Rate = 400 - 700/min • irregularly irregular; fibrillation waves • no organized atrial activity; no P waves Atrial fibrillation ..\..\Basic Rhythm Edited\5.avi Atrial Arrhythmias • Atrial flutter – saw tooth in appearance – irregular rate Atrial Flutter • Atrial rate 220-350/min • ventricular rhythm may be regular • P waves: flutter waves resemble SAWTOOTH or PICKET FENCE Atrial flutter ..\..\Basic Rhythm Edited\3.avi Atrial Fibrillation/Atrial Flutter Treatment: if unstable: cardiovert if stable : digoxin verapamil diltiazem -blockers Paroxysmal Supraventricular Tachycardia • Basic considerations – – – – – circus movement or reciprocating tachycardias utilize the mechanism of reentry Sudden onset Stops abruptly Usually a narrow QRS complex tachycardia • Exceptions: – Pre-existing conduction – Aberrant ventricular conduction – Pre-excitation SUPRAVENTRICULAR TACHYCARDIA • Characterized by tachycardia with a narrow QRS complex • sudden onset and termination • 150-250 beats/min (180 to 200 bpm in adults) • regular rhythm • QRS complex is normal in contour and duration • No P waves • P waves are generally buried in the QRS complex • Often, P wave is seen just prior to or just after the end of the QRS and causes a subtle alteration in the QRS complex that results in a pseudo-S or pseudo-r PSVT • Regular narrow-complex • Tachycardia without discernible P waves (?) • Sudden onset or cessation SUPRAVENTRICULAR TACHYCARDIA SUPRAVENTRICULAR TACHYCARDIA ..\..\Basic Rhythm Edited\2.avi 2. Rhythm ..\..\Basic Rhythm Edited\4.avi What’s the rhythm? What’s the HR? A) Atrial fibrillation B) Atrial flutter C) Supraventricular tachycardia D) Sinus tachycardia 13 x 10 = 130/min 2. Rhythm What’s the rhythm? A) Atrial fibrillation B) Atrial flutter C) Supraventricular tachycardia D) Sinus tachycardia What’s the HR? 7 x 10 = 70/min 2. Rhythm What’s the rhythm? A) Atrial fibrillation B) Atrial flutter C) Supraventricular tachycardia D) Sinus tachycardia What’s the HR? 9 x 10 = 90/min 2. Rhythm What’s the rhythm? A) Atrial fibrillation B) Atrial flutter C) Supraventricular tachycardia D) Sinus tachycardia ..\..\Basic Rhythm Edited\4.avi What’s the HR? 16 x 10 = 160/min 2. Rhythm A B C D 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia Atrial fibrillation Atrial flutter Supraventricular tachycardia First degree AV block Second degree AV block Third degree AV block BRADYCARDIAS: ATRIOVENTRICULAR BLOCKS Anatomical Sites of Heart Block First Degree AV Block • delay in passage of impulse from atria to ventricles • normal QRS; regular rhythm • PR interval prolonged >0.20 sec. Blocks ..\..\Basic Rhythm Edited\18.avi • 1st degree AV block – a PR interval that exceeds 0.20 sec 1st degree AV block ( PR = 0.28 sec) Blocks ..\..\Basic Rhythm Edited\19.avi • 2nd degree AV block (Mobitz) – a) type I (Wenckebach) • longer and longer PR intervals until a QRS is dropped Blocks ..\..\Basic Rhythm Edited\20.avi • 2nd degree AV block (Mobitz) – a) type I (Wenckebach) • longer and longer PR intervals until a QRS is dropped Second Degree AV Block • MOBITZ Type I (wenckebach) progressive prolongation of PR interval until an impulse is blocked Blocks ..\..\Basic Rhythm Edited\20.avi • 2ND DEGREE AV BLOCK (MOBITZ II) b) type II • P waves are regular, PR duration is constant and then suddenly a QRS is dropped Type II 2nd Degree AV Block • No lengthening of PR interval before a dropped beat HIGH GRADE AV BLOCK 3rd degree AV block ..\..\Basic Rhythm Edited\21.avi • P waves with a regular P to P interval • QRS complexes with a regular R to R interval • The PR interval will appear variable because there is no relationship between the P waves and the QRS Complexes Third Degree AV Block • Complete absence of conduction between atria and ventricles • atrial rate is always equal to or more than ventricular rate • QRS may be narrow or wide depending on level of block 3rd Degree AV Block • level of AV Node 3rd Degree AV Block • At ventricular level Paced Rhythm 2. Rhythm What’s the rhythm? A) First degree AV block B) Second degree AV block C) Third degree AV block 2. Rhythm What’s the rhythm? A) First degree AV block B) Second degree AV block C) Third degree AV block A. Mobitz I (Wenckebach) B. Mobitz II 2. Rhythm Mobitz I or Wenchebach Non conducted p Mobitz II 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia Atrial fibrillation Atrial flutter Supraventricular tachycardia First degree AV block Second degree AV block Third degree AV block Escape Rhythms: Junctional Rhythm Idioventricular Rhythm Junctional Complexes • conducting tissue near AV node has taken over the pacemaker of the heart • rate 40-60 • usually with retrograde P waves Junctional Rhythm Junctional Rhythm •Impulses from the AV node •P wave inverted or buried w/in QRS or follows the QRS •Rate slow •QRS narrow ..\..\Basic Rhythm Edited\6.avi •Impulses from the AV node •P wave inverted or buried w/in QRS or follows the QRS •Rate slow •QRS narrow Idioventricular Rhythm Impulse ventricular in origin Absence of (N), upright P wave associated with QRS complexes QRS > 0.10 sec T wave opposite in direction to QRS Rate < 40 / min Rate < 48 / min ACLS PHILHEART CENTER Accelerated Idioventricular Rhythm Impulse ventricular in origin Absence of (N), upright P wave associated with QRS complexes QRS > 0.10 sec T wave opposite in direction to QRS Rate = 40-120 / min Rate = 40-120 / min ACLS PHILHEART CENTER Accelerated Junctional Rhythm •Impulses from the AV node •P wave inverted or buried w/in QRS or follows the QRS •Rate 60-100 bpm •QRS narrow Idioventricular Rhythm ..\..\Basic Rhythm Edited\7.avi Idioventricular Rhythm •Impulse ventricular in origin •Absence of (N), upright P wave associated with QRS complexes •QRS > 0.10 sec •T wave opposite in direction to QRS •Rate < 40 / min Rate < 40 / min Accelerated Idioventricular Rhythm •Impulse ventricular in origin •Absence of (N), upright P wave associated with QRS complexes •QRS > 0.10 sec •T wave opposite in direction to QRS •Rate = 40-100 / min 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia Atrial fibrillation Atrial flutter Supraventricular tachycardia First degree AV block Second degree AV block Third degree AV block Escape Rhythms: Junctional Rhythm Idioventricular Rhythm Ventricular fibrillation Ventricular tachycardia VENTRICULAR TACHYCARDIA Wide complex tachycardia Premature Ventricular Contraction • • • • • • • Prematurely occurring complex. Wide, bizarre looking QRS complex. Usually no preceding P wave. T wave opposite in deflection to the QRS complex. Complete compensatory pause following every premature beat. ACLS PHILHEART CENTER Premature Ventricular Contraction in Couplets Two Premature ventricular contractions occurring consecutively ACLS PHILHEART CENTER Premature Ventricular Contraction in Bigeminy Alternating normal sinus beat and a PVC ACLS PHILHEART CENTER Premature Ventricular Contraction in Trigeminy PVC’s regularly occurring every third beat ACLS PHILHEART CENTER Multifocal Premature Ventricular Contraction PVC’s coming from different foci in the ventricle PVC’s assuming different polarities in a single lead PVC’s of different morphology and coupling interval ACLS PHILHEART CENTER Premature Ventricular Contraction R on T Phenomenon R or Q of the PVC occurring at the T wave of the preceding sinus beat Most dangerous PVC ACLS PHILHEART CENTER Ventricular tachycardia (V-tach) • impulse originates in the ventricle • always has a wide QRS complex ACLS PHILHEART CENTER Ventricular Tachycardia •At least 3 consecutive PVC’s •Rapid, bizarre, wide QRS complexes (> 0.10 sec) •No P wave (ventricular impulse origin) Rate > 100 / min ACLS PHILHEART CENTER ACLS PHILHEART CENTER Ventricular Tachycardia ACLS PHILHEART CENTER Ventricular Tachycardia • Nonsustained • Sustained • Monomorphic • Polymorphic • Torsades pointes • ..\..\Basic Rhythm Edited\9.avi Accelerated Idioventricular Rhythm With 2 foci of ventricular activity ACLS PHILHEART CENTER Pre excitation : WOLFF PARKINSON WHITE Rhythm is sinus except during pre excited tachycardia Short PR interval QRS distorted by delta wave ACLS PHILHEART CENTER Pre excited tachycardia ACLS PHILHEART CENTER Torsades de Pointes • A form of polymorphic VT • Electrical tracing appears to be twisted into a helix • This form of ventricular tachycardia degenerates relatively often into ventricular fibrillation ACLS PHILHEART CENTER Torsades de Pointes ACLS PHILHEART CENTER Ventricular Tachycardia Treatment: lidocaine procainamide amiodarone sotalol if unstable: electrical cardioversion or defibrillation for torsades de pointes: Magnesium Sulfate overdrive pacing ACLS PHILHEART CENTER Ventricular Fibrillation Associated with coarse or fine chaotic undulations of the ECG baseline No P wave No true QRS complexes Indeterminate rate Coarse Fibrillation Fine Fibrillation Ventricular fibrillation – complete breakdown of all rhythm Ventricular Fibrillation • single most important rhythm for an ACLS provider to recognize • no organized ventricular depolarization • no EFFECTIVE cardiac output • may be coarse or fine Coarse Ventricular Fibrillation Fine Ventricular Fibrillation Ventricular Fibrillation Ventricular Fibrillation Management Only DEFIBRILLATION provides definitive therapy 2. Rhythm What’s the rhythm? A) Ventricular fibrillation B) Ventricular tachycardia A) Monomorphic B) Polymorphic C) Torsade de Pointes 2. Rhythm Most commonly encountered rhythms: Normal Sinus Rhythm Sinus bradycardia Sinus tachycardia Atrial fibrillation Atrial flutter Supraventricular tachycardia First degree AV block Second degree AV block Third degree AV block Escape Rhythms: Junctional Rhythm Idioventricular Rhythm Ventricular fibrillation Ventricular tachycardia Asystole Ventricular Asystole • total absence of ventricular electrical activity • FLAT LINE PPROTOCOL : • check 2 leads on the monitor perpendicular to each other to make sure patient is in asystole • Check all connections of patient to monitor • Adjust gain/sensitivity Asystole • Pulseless ..\..\Basic Rhythm Edited\15.avi ASYSTOLE • absence of ventricular electrical activity • sometimes p waves or ventricular escape beats (agonal beats) may occur ASYSTOLE Treatment: epinephrine atropine search for reversible cause CPR 2. Rhythm What’s the rhythm A) Ventricular fibrillation B) Asystole Ventricular fibrillation changing to Asystole