Blood Composition, Function & Anemia: A Comprehensive Overview
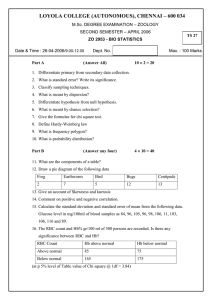
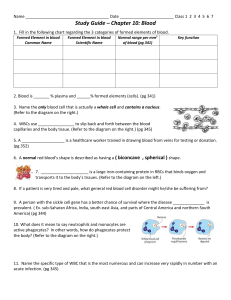
advertisement

Blood Mrs Sikazwe What is blood? • Blood is a connective tissue in fluid form. • Life - carries O2 from lungs to tissue and CO2 from tissue to the lungs. • Growth - carries nutritive substances from GIT and hormones from endocrine gland to all the tissues. • Health - protects the body against the diseases and gets rid of the waste products and unwanted substances by transporting them to the excretory organs like kidneys. Properties of blood •Colour: Blood is red in colour. •Volume: Average volume of blood in a normal adult is 5 L. •Reaction and pH: Blood is slightly alkaline and its pH in normal conditions is 7.4. •Viscosity: Blood is five times more viscous than water. •It is mainly due to red blood cells and plasma proteins. Blood cells • Red blood cells/erythrocytes, White blood cells/leukocytes and Platelets/ thrombocytes. Haematocrit Value/ packed cell volume (PCV). • Plasma forms 55% and RBCs form 45% of the total blood. Plasma and serum PLASMA • Plasma is a straw-coloured clear liquid part of blood. • contains 91% to 92% of water and 8% to 9% of solids. • The solids are the organic and the inorganic substances SERUM • Has no fibrinogen, i.e. serum contains all the other constituents of plasma except fibrinogen. Function of plasma • Coagulation of blood through fibrinogen • Gamma globulins act as antibodies (immune substances) immunoglobulins • Albumin, alpha globulin and beta globulin are responsible for the transport of hormones, enzymes, taking part in transportation • Maintain osmotic pressure as plasma proteins are too large to pass through the capillary membrane and remain in the blood where they exert colloidal osmotic (oncotic) pressure. • It regulates acid base balance in the blood. Bone marrow • In the adult, RBCs, many WBCs, and platelets are formed in the bone marrow. • In the foetus, blood cells are also formed in the liver and spleen • Active cellular marrow- red marrow • Inactive marrow infiltrated with fat - yellow marrow Life – as a function of blood Red blood cells • RBC count ranges between 4 and 5.5 million/mm3 of blood. • Diameter : 7.2 μ (6.9 to 7.4 μ). • Normally, the RBCs are disk shaped and biconcave (dumbbell shaped). • Central portion is thinner and periphery is thicker. FUNCTIONS Transport of Oxygen from the Lungs to the Tissues • Haemoglobin in RBC combines with oxygen to form oxyhaemoglobin. Transport of Carbon Dioxide from the Tissues to the Lungs • Haemoglobin combines carbon dioxide and carbhemoglobin. with form Buffering Action in Blood •Hb regulates H+ concentration and plays a role in the maintenance of acid base balance In Blood Group Determination •RBCs carry the blood group antigens like A antigen, B antigen and Rh factor. •This helps in determination of blood group and enables to prevent reactions due to incompatible blood transfusion Haemoglobin in RBC • Hb is an iron containing colouring matter of RBCs • Average Hb content in blood is 14 to 16 g per 100 mL • Erythroblasts manufacture a pyrrole ring • 4 combine to form protoprophyrin or porphyrin • The porphyrins are connected by methane CH4 •Iron is added to the structure in the centre • It attaches to the N part of each pyrrole ring • This structure is called a heme •The cell synthesizes a peptide chain • May be alpha, beta, gamma or delta • These are known as globins • This attachment of a peptide chain to iron of a heme makes a haemoglobin monomer Function of Haemoglobin •Transportation of O2 from the lungs to the tissues by forming oxyhaemoglobin •O2 binds with Hb by attaching to Fe2+ of the heme and this is enhanced by increase in temperature, RBC concentration, 2,3, DPG decrease • 2,3 DPG and H+ compete with O2 for the binding site and therefore decrease Hb affinity for O2 •O2 is released in tissue due to pressure differences •CO2 is transported from the tissues to the lungs by formation of carbaminohaemoglobin • Increase in CO2 in tissue allows it to diffuse to plasma and RBC • Dissolved CO2 from the cell enters capillaries • It may be transported like this to the lungs or bind to Hb to form carbaminohaemoglobin • It acts as a buffer in maintaining blood pH • It does so by binding and releasing H+ when need arises • An RBC has carbonic anhydrase present that allows for the production of H+ • The H+ binds to another component of Hb reducing the affinity of O2 by Hb • It can be released when H+ is in low concentration Destruction of RBC • When RBCs are destroyed, haemoglobin is degraded into heme and globin • Globin returns to the body’s metabolic pool where its amino acids are utilised • The porphyrin ring of heme is degraded by heme oxidase to yield biliverdin • Biliverdin is further reduced to form bilirubin by biliverdin reductase RBC Indices Mrs. Sikazwe Anaemia • Has many causes - a sign of disease . • Associated with reduction in circulating Hb because of reduced numbers of erythrocytes or less Hb per erythrocyte . • The physiologic result of low circulating Hb is the reduced capacity for blood to carry oxygen • Iron deficiency anaemia • excessive loss of iron . • Women are at risk. ---- For menstrual blood and growing foetus. • Megaloblastic anaemia • Less intake of vitamin B 12 and folic acid. • Red bone marrow produces abnormal RBC. • RBC too large and low in number • Cannot proliferate rapidly • They have fragile membrane and easily rapture • Pernicious anaemia • Inability of stomach to absorb vitamin B 12 in small intestine. • Haemorrhagic anaemia • Excessive loss of RBC through bleeding, stomach ulcers, menstruation • Aplastic anaemia • destruction of red bone marrow . • Haemolytic anaemia- Fragile RBC which easily rupture • Could be normal, but have a shorter life span • Hereditary spherocytosis • RBC are small and round • Cant withstand the compression pressure • Sickle cell • Abnormal shape with faulty beta chains • HbS when exposed to low O2 precipitates forming crystals that damage the cell membrane Determination of RBC Indices • Hb content – normal male 14 to 18g/dl of blood and female12 – 16g/dl of blood • Parked Cell Volume (haematocrit) • Red cell count – (method noted) • From these 3, indices can be calculated; • Mean corpuscular volume (MCV) • Volume/size of average RBC • Mean corpuscular haemoglobin (MCH) • Weight of Hb in the average RBC • Mean corpuscular haemoglobin concentration (MCHC) • Hb concentration or colour of average RBC Mean corpuscular volume • MCV in femtolitre (fl); 1fl = 10-15 litre • MCV (fl) = haematocrit (per cent) x 10/RBC count (millions per mm3) • If haematocrit is 45% and RBC count is 5 million/mm3 of blood gives • 45 x 10/5 = 90fl • Normal value 78-96fl • Increase in value means cells are too large • Decrease means too small (decreased Hb synthesis, iron deficiency) Mean corpuscular haemoglobin (MCH) •How much the average weight of Hb in a RBC – pictograms (1 pg = 10-12g) • MCH (pg) = Hb (g/dl) x 10/RBC count in millions/mm3 • If Hb content is 14g/dl and RBC count is 5 million/mm3 • MCH = 14 x 10/5 = 28pg •Normal value 27 – 33pg • Subnormal values occur in iron deficiency Mean corpuscular haemoglobin concentration (MCHC) • Average Hb concentration per unit volume of parked red cells g/dl or % • MCHC % = (Hb (g/100ml)/PCV/100ml) x 100 • If Hb content is 15g/dl and PCV is 45% • MCHC = 15/45 x 100 = 33.3% • Normal value 30 to 37g/dl or % • Above 40% indicates errors in the instrument • Increased values denote dehydration of red cells • Subnormal indicate abnormal Hb formation- iron deficiency Colour index (CI) • The ratio of Hb% to RBC% • Decreases with decrease in Hb and increases if RBC % is low • Indicates the Hb content in RBC • CI = Hb%/RBC% • 100% of Hb = 14.8 g/100ml • 100% of RBC = 5 million/mm3 • Normal value – 0.85-1.10 • CI less than 0.85 indicates hypochromic anaemia Cell type Low High Neutrophils Physiological Chronic exposure to severe cold Physiological Emotional stress, food intake, exercise, pregnancy Pathological Starvation, typhoid, aplastic anemia, parasitic infection like malaria, viral infections like measles, influenza, viral hepatitis Pathological Acute pyogenic infection, noninfective inflammation , acute hemorrage, trauma, leukemia Eosinophils Cushings diseases, aplastic anemia, stress Allergic condition; bronchial asthma, food allergy, hay fever; Parasitic infestations – hookworm, filariasis; skin disease Basophils Septicemia or aplastic anemia Chronic myeloid leukemia, polycythemia Lymphocytes Bone marrow failure, immune deficiency, Hodgkins disease TB, whooping cough, syphilis, viral infections Monocytes Bone marrow failure, aplastic anemia, septicemia Protozoan disease- malaria, kala azar, Hodgkinn’s disease Blood type Mrs Sikazwe Determination of blood group • Landsteiner laws: • If a particular agglutinogen (antigen) is present in the RBCs, corresponding agglutinin (antibody) must be absent in the serum. • If a particular agglutinogen is absent in the RBCs, the corresponding agglutinin must be present in the serum. • Two agglutinogens/antigens have been noted on the surface of RBCs – A and B • Therefore, if a person has A antigen, he may not require the A antibodies in his serum/plasma and they will bind (agglutination) • This is true for B Structure of antigens on RBCs • The A and B antigens are complex oligosaccharides – H component • H component of the antigen is usually present in individuals of all blood types and has fucose transferase that codes for terminal fuscose • A antigen expresses a terminal Nacetylgalactosamine on the H antigen • B antigen expresses a terminal galactose. • Individuals who are type AB have both transferases. • Individuals who are type O have neither, so the H antigen persists. Inheriting ABO blood types • Each parent donates one of their 2 AB genes to their child • Parent with O type only passes an O gene to her offspring • Parent with AB passes either A or B gene to offspring • If the above were a couple, children would have the following types • The A can be homozygous (AA) or heterozygous (AO) and the B phenotype can be homozygous (BB) or heterozygous (BO) • Note that O is the recessive gene in this case Agglutination • If a particular agglutinogen is absent in the RBCs, the corresponding agglutinin must be present in the serum • If you take a prepared serum with a known agglutinin, you can determine which type of agglutinogen is present by noticing binding/clumping/agglutination • If Serum had B antibodies/agglutinins (Anti B); they will only react in the presence of a B agglutinogen/antigen • Therefore if clumping is observed, then the person must be a type B or type AB • To note if they are type AB, clumping will also be observed when serum with antibody A is mixed with the blood • Since O has not antigens that can clump, they are noted to stay unreactive with all types of serum Matching • Blood matching (typing) is a laboratory test done to determine the blood group of a person • For blood matching, RBC of the individual (recipient) and test serum are used. • Matching = Recipient’s RBC + Test serum. • Cross-matching is done to find out whether the person’s body will accept the donor’s blood or not. • Cross-matching is done by mixing the serum of the recipient and the RBCs of donor. • Cross-matching = Recipient’s serum + Donor’s RBC Transfusions •When the recipient's plasma has agglutinins against the donor's red cells, the cells agglutinate and haemolyse. •Persons with type AB blood are "universal recipients" • They have no circulating agglutinins/antibodies •Type O individuals are "universal donors" because they lack A and B antigens • Can be given to anyone without producing a transfusion reaction due to ABO incompatibility. Rhesus • Rh factor is an antigen present in RBC. • There are many Rh antigens but only the D antigen is more antigenic in human. • The persons having D antigen are called ‘Rh positive’ and those without D antigen are called ‘Rh negative’. • The antigen D does not have corresponding natural antibody (anti-D). • However, if Rh positive blood is transfused to a Rh negative person anti-D is developed in that person. • Rhesus factor is an inherited dominant factor. • It may be homozygous Rhesus positive with DD or heterozygous Rhesus positive with Dd • Rhesus negative occurs only with complete absence of D (i.e. with homozygous dd). Rh and transfusion • When a Rh negative person receives Rh positive blood for the first time, he is not affected much, since the reactions do not occur immediately. • But, the Rh antibodies develop within one month. • The transfused RBCs, which are still present in the recipient’s blood, are agglutinated. • These agglutinated cells are lysed by macrophages. • A delayed transfusion reaction occurs. • But, it is usually mild and does not affect the recipient. • However, antibodies developed in the recipient remain in the body forever. • When this person receives Rh positive blood for the second time, the donor RBCs are agglutinated and severe transfusion reactions occur immediately. Haemolytic disease • Disease in foetus and new-born, characterized by abnormal haemolysis of RBCs. • It is due to Rh incompatibility • Leads to erythroblastosis fetalis which is is a disorder in foetus characterized by the presence of erythroblasts in blood. • When a mother is Rh negative and foetus is Rh positive (the Rh factor being inherited from the father), sensitization will occur; • Noted during delivery of the child • Rh antigen from foetal blood may leak into mother’s blood because of placental detachment. •Within a month after delivery, the mother develops Rh antibody in her blood. •When the mother conceives for the second time and if the foetus happens to be Rh positive again; •The Rh antibody from mother’s blood crosses placental barrier and enters the foetal blood. •Rh antigen cannot cross the placental barrier, whereas Rh antibody can cross it.