KUNDAVARAPU DINESH NAIDU (group 1) task 2 ASEPSIS
advertisement

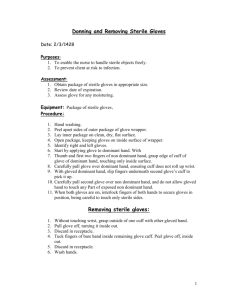
KUNDAVARAPU DINESH NAIDU ASCEPSIS GROUP-1 General Surgery Situational Tasks Topic No. 2 "Aseptic" Situation task No. 1 The patient after the appendectomy operation on day 4 felt discomfort in the postoperative wound area. Inflammation phenomena appeared in the wound. The surgeons who made the dressing removed the sutures, while receiving 10 ml of purulent detachable mixed blood. The patient is in a ward with 3 more people. Question: What needs to be done with this patient? Answer: Patient must be moved to an isolated area until the doctors find the microorganism is transferable to other patients through any medium and want to take certain antisepsis (like surgical vacuum drain) treatment immediately for the patient, so the patients health can be restored. Situation Task No. 2 During the operation, the surgeon found a small defect in the glove. When changing gloves, there were traces of blood on the finger. Question: What should be done in this case? Answer: The surgeon must immediately sterilize (with alcohol solution etc.) his hands to not to spread any infections to the patient itself or any other surgeon or nurses in the operation theater and he want to wear a new sterile gloves to perform the surgery. He must inform everyone in the operation theater that his glove has a defect. Situation Task No. 3 During the operation, an instrument contaminated with the patient's blood fell on the floor. Question: What should be done in this case? Who should perform these actions? Answer: flash sterilization and cidex are good options but sometimes we would need to have the instrument fully reprocessed. But it will be a safe option to keep a spare of the sterilized instruments because sometimes the operation must be completed immediately we can’t wait for the instrument to be sterilized and start the procedure this can lead to the patient’s death. The nurse should take care of the instrument that fell on the floor. Situation task No. 4 After disinfection and washing of tools, a reaction to hidden blood was carried out before sterilization. The result is positive. Question: what does this mean? What should be done in this case? Answer: - This means the blood is contaminated with microorganisms. A disinfectant cant clean spores present on the instruments so these spores can be developed int a specific microorganism. KUNDAVARAPU DINESH NAIDU ASCEPSIS GROUP-1 These instruments must be sterilized in a proper manner and make sure that the instruments are free of microorganisms before storing for next use Situation task No. 5 After autoclaving, the thermal band remained white in the bixe (sterilizing box) Question: what does this mean? What do I need to do with this content? Answer: - This means that the autoclave is not working properly, or the band is a defect one. But we need to re sterilize the instruments to prevent any unwanted infections in hospital. i.e. Double autoclave Situation task No. 6 The surgeon was regularly analyzed for oropharyngeal microflora. Result positive for S. Aureus Questions: Why is sowing on microflora? What should be done in this case? Answer: - Staphylococcus aureus is the most dangerous of all the many common staphylococcal bacteria. It often causes skin infections but can cause pneumonia, heart valve infections, and bone infections. This bacteria are the natural flora in pharynx and throat of the humans. But it will cause Diseases if the amount of the bacteria is more and if they entered into the blood stream. So, the Surgeon can be a major risk to be in an operation theatre as he can spread this bacteria as this can spread through the hands which can contaminate the surgical instruments and it can travel even through air. It is better that the doctor must avoid the surgeries and he must have proper treatment Situation task No. 7 Surgeons 2 days before the operation received wounds on the index finger of the right hand. There are inflammation phenomena Question: Can surgeons perform surgery in this situation? What does he need to do? Answers: - No, he can affect the patient as well as his wound will become large as the index finger is mainly used for preforming surgery. So, he must have specific treatment for the wound after the wound has been cured he can perform his surgeries normally. Situation task No. 8 In a microbiological study, E. Coli E. coli was seeded on the bed Question: what does this mean? What should we do? KUNDAVARAPU DINESH NAIDU ASCEPSIS GROUP-1 Answers: - This E. coli can be from his fecal discharge or from his wounds. It is better to change the clothes of the patient as well as bedsheets and pillow covers and sanitize the entire bed and the things near him. Situation Task No. 9 During the operation, the floor was contaminated with blood and pus. After the completion of the operation, a patient arrived who needs to be operated on urgently. Question: How to prepare the operating room for the next operation? Answer: -we must clear the pus and the blood with proper disinfectants and sterilize the entire room in a proper manner like by using the antiseptic liquids to clean the floors and removing the air from the room and filling with fresh air and sterilizing the contaminated instruments. Self-Training Questions: 1. operating field processing principles before an operation A. BASIC ASEPTIC PRINCIPLES All articles must be sterilized before use in procedure. If in doubt about sterility of item or person, it is not! All persons who touch sterile articles must be sterile. Non-sterile persons never reach across a sterile field. Draped tables are sterile only above the table level. Gown front is sterile only from waist to shoulder level. Moisture causes contamination. Before entering the operation room, one should: a) Change into clean scrubs (anaesthesiologists are allowed to wear their in hospital clothes). b) Remove all jewellery, watches and rings (risk of bacteria transfer is 10 times higher when nurse wears rings). c) Remove pager and cell phone. d) Put on surgical cap, mask, shoe covers (mask must be tied before entering the operation room; hair must be completely covered), waterproof apron (not necessary if waterproof gowns are used): protective clothing use reduces the risk KUNDAVARAPU DINESH NAIDU ASCEPSIS GROUP-1 of transmitting infection by 20-100 times! e) Surgeons and operation nurses should wash hands using international standard for hands processing (to be prepared for scrubbing in the operation room) and put on sterile gowns 1. A. rules for dressing sterile gloves Steps to put on sterile gloves Place the package of sterile gloves in a clean work area. Having the outside glove wrapper open before scrubbing allows the surgeon to lift the left glove with his/her right hand, holding the glove by the turned down cuff. This prevents touching of the outside surface of the glove. Without unfolding the cuff, place the left hand into the glove while the right hand carefully pulls the glove up, leaving the cuff turned down. The left gloved hand then reaches under the turned down cuff of the right glove and steadies it while inserting the right hand. Then, by reaching under the turned down cuff, the wearer can pull the glove up snugly and unfold the cuff up over each wrist and sleeve of the gown. . 2. A. rules for dressing a sterile gown a) When putting on the sterile gown, avoid touching the front surface of the gown and keep the gown from touching any object. b) Remove the gown from the autoclaved bundle, hold it at the neck, and allow it to unroll. With the back of the gown toward the wearer, carefully shake out and unfold it. c) While the assistant holds the collar at the left tie string with the right hand, the wearer inserts the left arm into the sleeve. d) Then while the assistant holds the collar at the right tie string with the left hand, the wearer inserts the right arm into the sleeve. e) While awaiting the assistant to tie and adjust the gown, the wearer keeps both arms extended upward.