Panagglutination Case Report: Alloantibodies & Blood Transfusion
advertisement
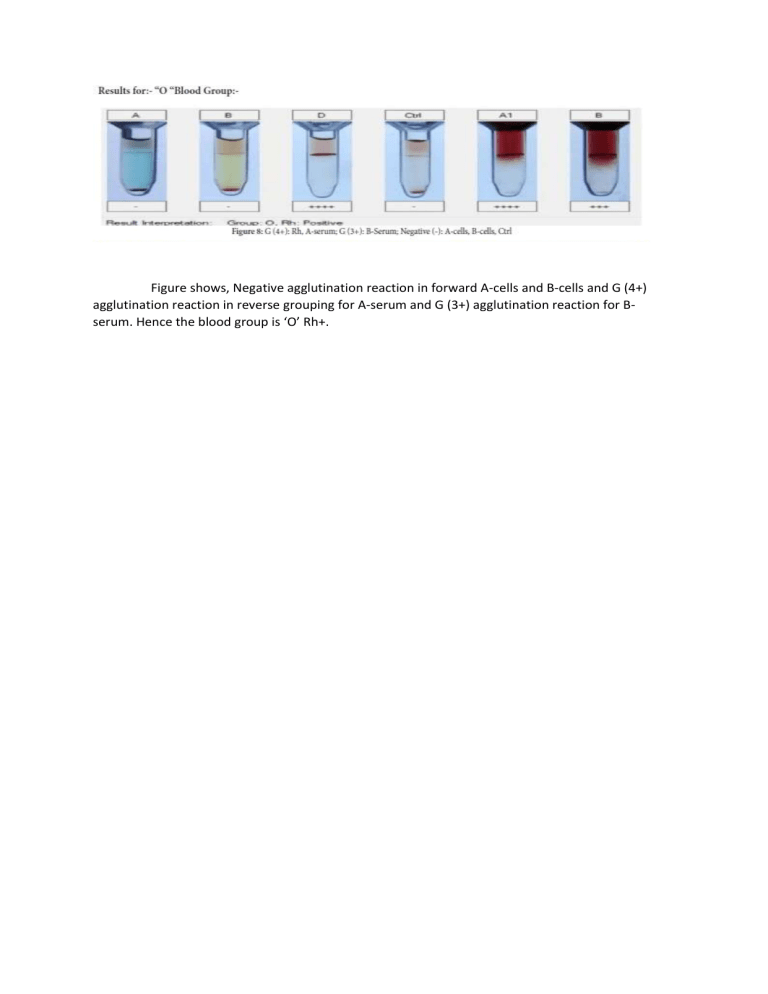
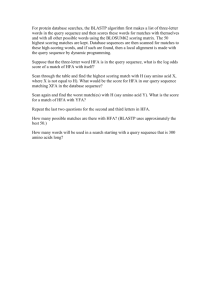
Figure shows, Negative agglutination reaction in forward A-cells and B-cells and G (4+) agglutination reaction in reverse grouping for A-serum and G (3+) agglutination reaction for Bserum. Hence the blood group is ‘O’ Rh+. Case Report of a Panagglutination due to alloantibodies Annapurna Ramesh, Deepak Bhandari, Ankit Mathur TTK Rotary Regional Transfusion Centre, Bangalore, India Background: Red cell serology is a complex area though appears as simple technology. Panagglutinating sera are rare (0.089%) occurrence. Panagglutination is a patient sera agglutinates with all red blood cells (RBCs) tested in first approach. Also agglutinates all RBCs screening and identification of panel cells. A Panagglutinating serum is challenging dilemmas of the antibody identification and to manage the patient transfusion wise, even in advanced countries. In this situation, systematic workup is necessary to reduce the risk of error and optimize the sample use as many tests need to be done and repetitions of few tests are necessary. Panagglutinating sera to high frequency antigen e.g. Cartwright, Colton, Diego, Vel, Scianna etc is (0.002%), and due to auto antibody is (0.087%) Case Report: We investigated serum of a female patient 31years of age for Panagglutination, posted for Spinal cord neurosurgery. We received her sample on 14 April 2011 for grouping and two units PRBC reservation. She gave H/O G3, P1, A2, without previous H/O blood transfusions, H/ O treated tuberculosis 2 years ago. https://www.ajts.org/article.asp?issn=09736247;year=2012;volume=6;issue=1;spage=59;epage=129;aulast= We sent the sample for Ab identification to TTK Regional Centre and found 2 + agglutination in all 11 Ab identification panel red cells; auto control was negative for agglutination (Bioview), DCT Negative, tube technique did not pick up the alloantibody. DCT Negative, auto control negative, Hb-11.6gm %, normal blood smear ruled out auto antibody and alloantibody was causing Panagglutination. Alloantibody to high-frequency antigen (HFA) - Ab corresponding to HFA usually best reacts by IAT, uniform grading seen in panel cells and IAT tests with red cells. Multiple antibodies to recognizing antigens (other than HFA) - differential Grading seen is due to variable intensity and distribution of multiple antigens in panel cells. Clinically insignificant High-titer, low-avidity (HTLA) antibodies usually agglutinate with W+ to 1+ grading in IAT. Uniform 2+ agglutination in IAT suggested alloantibody to a HFA. Chances of HTLA antibodies cannot be ruled out and further investigations such as extended cell panel testing, genotyping and in vitro test for predicting the outcome of transfusing incompatible blood are desirable. Clinical Management: Informed all details to clinicians. Blood was neither reserved nor utilized. Post operative period was uneventful. Oral haemetenics prescribed. Conclusion: In this case, panagglutination was due to HFA alloantibodies (? HTLA) acquired as a result of pregnancy. Patients lacking high-frequency antigen with HFA alloantibodies are rare. Due to rarity of blood donors lacking corresponding HFA, it is most difficult to arrange HFA negative blood. Also in vitro pre-transfusion tests for predicting the outcome of transfusing incompatible blood are invaluable in these rare cases.