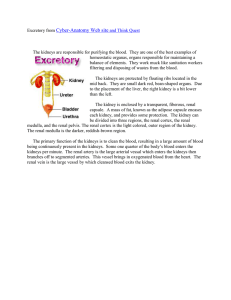
BJOG: an International Journal of Obstetrics and Gynaecology December 2002, Vol. 109, pp. 1388 –1393 Prenatal diagnosis of bilateral isolated fetal hyperechogenic kidneys. Is it possible to predict long term outcome? V. Tsatsarisa,b, M.F. Gagnadouxb,c, M.C. Aubryb,d, M.C. Gublerb,e, Y. Dumezb,d, M. Dommerguesb,d,* Objective To study perinatal and long term outcome following prenatal diagnosis of hyperechogenic kidneys. Design Prospective observational cohort study. Setting The Maternité Port-Royal Hôpital Cochin and at the Departments of Obstetrics and Paediatric Nephrology, Necker Enfants Malades in Paris, France. Population Forty-three fetuses with isolated bilateral hyperechogenic kidneys. Methods All patients referred with isolated bilateral hyperechogenic fetal kidneys were followed up prospectively up to 34 –132 months. The following prenatal items were analysed: fetal kidney size, amniotic fluid volume, gestational age at diagnosis, family history and renal ultrasound in parents. Postmortem examination was carried out in cases with perinatal death. Postnatal follow up of survivors included postnatal ultrasound, blood pressure, serum creatinine, proteinuria, need for restricted diet, weight and height and renal biopsy when available. Main outcome measures Aetiology of hyperechogenicity, perinatal mortality and renal function in survivors. Results The aetiology could be established by family history, postmortem or postnatal data, but not by prenatal ultrasound. There were 20 autosomal recessive, 8 autosomal dominant polycystic kidney diseases, 9 other renal disorders and 6 symptom-free survivors without aetiological diagnosis. There were 19 terminations of pregnancy, 5 neonatal deaths and 19 survivors, of whom 14 had normal renal function three had mild and two had end stage renal failure. None of those with severe oligohydramnios and fetal kidneys > 4 SD survived (n ¼ 14, 10 terminations and 4 neonatal deaths), whereas of the 17 with normal amniotic fluid volume and kidneys < 4 SD, 14 survived, of whom 9 were symptom-free. Conclusion Aetiology could not be established prenatally in the absence of familial data. Kidney size and amniotic fluid volume were the best prenatal predictors of outcome. INTRODUCTION Obstetricians are increasingly facing the challenge of counselling pregnant women following sonographic prenatal diagnosis of fetal abnormalities carrying an uncertain prognosis. Prenatal diagnosis of hyperechogenic kidneys a Department of Obstetrics, Maternité Port-Royal Hôpital Cochin, AP-HP, Paris, France b Université Paris V, Paris, France c Department of Paediatric Nephrology, Hôpital Necker Enfants Malades, AP-HP, Paris, France d Department of Obstetrics, Hôpital Necker Enfants Malades, AP-HP, Paris, France e INSERM U423, Hôpital Necker Enfants Malades, AP-HP, Paris, France * Correspondence: Dr M. Dommergues, Maternité Hôpital Necker, 149 Rue de Sèvres, 75015 Paris, France. D RCOG 2002 BJOG: an International Journal of Obstetrics and Gynaecology PII: S 1 4 7 0 - 0 3 2 8 ( 0 2 ) 0 2 9 5 5 - 5 is an example of this difficult situation, in which providing women with over pessimistic information leads to unnecessary termination of pregnancy, whereas reassuring patients without any restriction may be unfair. This underscores the need for basing prenatal counselling on prenatal cohorts with a long term postnatal follow up. There are few series of prenatal diagnosis with postnatal follow up1 – 5, and performing prenatal counselling based only on postnatal data is flawed by a number of biases. First, fetal sonography usually fails to provide an accurate aetiological diagnosis, and fetal hyperechogenic kidneys may result from a variety of aetiologies. Second, within each aetiological group, there is a wide range of outcomes. Postnatal series are likely to overlook the most severe cases, leading to perinatal death, as well as the mildest ones, which may remain undetectable clinically over a long period. So far, the outcome of fetal hyperechogenic kidneys can only be predicted accurately in the most severe cases, in which terminal renal failure is ascertained by severe oligohydramnios. In order to provide data on the long term outcome of fetal hyperechogenic kidneys, we conducted a prospective www.bjog-elsevier.com LONG TERM POSTNATAL FOLLOW-UP OF BILATERAL ISOLATED FETAL HYPERECHOGENIC KIDNEYS A 1389 B L L K K C K L Fig. 1. Legend: K ¼ kidney; L ¼ liver; A ¼ hyperechogenic kidney; B ¼ borderline kidney, yet considered as hyperechogenic; C ¼ non-hyperechogenic kidney. cohort study on 45 cases with prenatal diagnosis of hyperechogenic kidneys. METHODS Between 1985 and 1996, the diagnosis of isolated bilateral hyperechogenic fetal kidneys was made in 45 pregnant women referred to our department. Eleven patients had been screened for fetal kidneys abnormalities because of a family history of autosomal recessive (n ¼ 4) or dominant (n ¼ 7) polycystic kidney disease. In 34 cases, abnormal fetal kidneys were picked up by routine ultrasound. Additional anomalies were ruled out based on ultrasound and fetal karyotyping. Absence of associated anomalies was confirmed by postnatal or by postmortem examination. Cases with (i) urinary tract dilatation, (ii) macrocysts suggestive of multicystic kidneys or (iii) extra urinary abnormalities were not included. D RCOG 2002 Br J Obstet Gynaecol 109, pp. 1388 – 1393 Kidneys were considered as hyperechogenic when their echogenicity was greater than that of the liver (Fig. 1). The size of the kidneys was expressed as standard deviations above or below the mean derived from the growth charts of Le Guern et al.6. The amount of amniotic fluid was assessed in a semiquantitative fashion. Oligohydramnios was considered as severe when no amniotic pool greater than 2 cm could be identified by ultrasound. The diagnosis of moderate oligohydramnios was made on a subjective basis7. In the absence of a positive family history, parents were screened by ultrasound for renal cysts suggestive of autosomal dominant polycystic kidney disease (ADPKD). Prenatal management was based on the assessment of amniotic fluid volume. Termination of pregnancy was offered in cases with severe oligohydramnios. In cases with moderate oligohydramnios, the decision to continue the pregnancy or not was postponed and was eventually made based on prenatal sonographic follow up. In cases with 1390 V. TSATSARIS ET AL. Table 1. Autosomal recessive polycystic kidney disease. Case GA AF Perinatal outcome Indication for ultrasound Kidney’s height (SD) Follow up (months) Creatinine clearance Clinical symptoms 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 29 22 18 27 32 24 35 30 34 30 31 28 36 33 21 29 34 32 35 27 MOH N N MOH SOH SOH SOH SOH SOH SOH SOH MOH MOH SOH N MOH N N N N TOP TOP TOP TOP TOP TOP TOP TOP TOP TOP NND NND NND NND alive alive alive alive alive alive family history family history family history routine routine routine routine routine routine routine family history routine routine routine family history routine routine routine routine routine 3 2 3 3 7 3 4 4 8 6 4 9 9 7 3 3 3.5 – 5 1.8 132 132 84 84 120 120 49 121 96 55 159 106 hypertension, renal failure hypertension hypertension renal failure none none Postnatal ultrasound large HE kidneys and large HE kidneys and large HE kidneys and HE kidneys and cysts large HE kidneys and multiple microcysts cysts cysts cysts cysts TOP ¼ termination of pregnancy; AF ¼ amniotic fluid volume (MOH ¼ moderate oligohydramnios, PH ¼ polyhydramnios, SOH ¼ severe oligohydramnios, N ¼ normal amniotic fluid volume); NND ¼ neonatal death; HE kidneys ¼ hyperechogenic kidneys; GA ¼ gestational age at diagnosis. Creatinine clearance was calculated according to Schwartz formula (mL/min/1.73 m2). normal amniotic fluid volume, parents were encouraged to continue the pregnancy. However, following counselling by a fetal medicine specialist and a paediatric nephrologist, parental autonomy was respected as for continuing or terminating the pregnancy. Postmortem histological examination was performed in all cases of termination of pregnancy or of neonatal death. Among survivors, postnatal follow up was obtained based on reviewing medical records of children followed in our institution or interviewing the paediatrician in charge of children followed outside our hospital. The following items were recorded: (1) postnatal ultrasound, (2) blood pressure, (3) serum creatinine, (4) proteinuria, (5) need for restricted diet, (6) weight and height and (8) renal biopsy when available. Creatinine clearance was calculated according to Schwartz formula8. We did not screen for PKD1 or PKD2 gene mutations routinely because of technical limitations related to the genetic and allelic heterogeneity of ADPKD and to the complex structure of PKD genes. RESULTS Of 45 cases in which isolated hyperechogenic kidneys were diagnosed in utero, 43 had a complete follow up and form our database. There were 19 terminations of Table 2. Autosomal dominant polycystic kidney disease. Case GA AF Perinatal outcome Indication for ultrasound Kidney’s height (SD) Follow up (months) Creatinine clearance Clinical symptoms Postnatal ultrasound 21 22 23 24 25 26 27 28 21 24 23 33 23 36 28 24 MOH SOH SOH N N N MOH N TOP TOP TOP alive alive alive alive alive routine routine family history family history family history family history routine routine 8 9 7 2 2 5.5 1 2 58 88 130 36 34 NA NA 72 90 97 none none hypertension, renal failure none none NA NA large HE kidneys and cysts HE kidneys and cysts HE kidneys and cysts TOP ¼ termination of pregnancy; AF ¼ amniotic fluid volume (MOH ¼ moderate oligohydramnios, PH ¼ polyhydramnios, SOH ¼ severe oligohydramnios, N ¼ normal amniotic fluid volume); GA ¼ gestational age at diagnosis; NA ¼ not available. Creatinine clearance was calculated according to Schwartz formula (mL/min/1.73 m2). Cases 24 and 25 were two sisters born to a mother affected by ADPKD who elected not to have any imaging or biochemical screening performed in her children. In cases in which fetal renal hyperechogenicity was picked up by routine ultrasound, the diagnosis of ADPKD was made based on renal cysts in one of the parents or grandparents. D RCOG 2002 Br J Obstet Gynaecol 109, pp. 1388 – 1393 LONG TERM POSTNATAL FOLLOW-UP OF BILATERAL ISOLATED FETAL HYPERECHOGENIC KIDNEYS 1391 Table 3. Other renal abnormalities. Case GA AF Perinatal outcome Indication for ultrasound Kidney height SD Follow up (months) Creatinine clearance 29 30 31 32 33 34 35 36 34 23 21 22 31 23 20 30 SOH SOH N MOH SOH N SOH PH TOP TOP TOP TOP TOP TOP NND alive routine routine routine routine routine routine routine routine 2.5 1 5 4 6 1.5 1 1 60 74 37 22 N alive routine 3.5 61 11 Clinical symptoms/ postmortem diagnosis diffuse cortical cysts multicystic horseshoe kidney cystic dysplasia cystic dysplasia multicystic kidney nephrocalcinosis tubular dysgenesis MRF CTI, ESRF, hypertension, renal transplantation graft rejection Postnatal ultrasound small hyperechogenic kidneys with cysts cortical microcysts TOP ¼ termination of pregnancy; AF ¼ amniotic fluid volume (MOH ¼ moderate oligohydramnios, PH ¼ polyhydramnios, SOH ¼ severe oligohydramnios, N ¼ normal); CMD ¼ corticomedulary differentiation; GA ¼ gestational age at diagnosis; MRF ¼ moderate renal failure; NND ¼ neonatal death; ESRF ¼ end stage renal failure; CTI ¼ chronic tubulointerstitial nephropathy with cortical microcysts. Creatinine clearance was calculated according to Schwartz formula (mL/min/1.73 m2). pregnancy, 5 neonatal deaths and 19 survivors, who were followed for 34 –132 months (median: 84 months). Sonographic data such as kidney size, amniotic fluid volume or the degree of hyperechogenicity did not contribute to establishing the aetiology. This was achieved by postmortem results, postnatal follow up, and/or family history either known before pregnancy or uncovered following prenatal diagnosis. Twenty cases (46%) were diagnosed as autosomal recessive polycystic kidney disease (ARPKD) eight (19%) as ADPKD and nine (21%) as other renal disorders. In the remaining six cases (14%), it was not possible to establish the aetiology of fetal renal hyperechogenicity. Of the 34 cases in which hyperechogenic fetal kidneys were picked up by routine sonography in the absence of a known family history, there were 15 ARPKD (44%), 4 ADPKD (12%), 9 cases with other renal disorders (26%) and 6 idiopathic cases (18%). Of the 20 cases of ARPKD, 15 were picked up by routine sonographic screening, whereas in 5 cases prenatal sonography was performed because of a family history (Table 1). At the time of referral, oligohydramnios was severe in eight cases, moderate in five and with normal amniotic fluid volume in seven cases. There were 10 terminations of pregnancy, 4 neonatal deaths and 6 children survived. Of the survivors, two were symptom-free, three had hypertension with renal insufficiency in one of them and one had renal failure. The diagnosis of ADPKD was made in eight cases (Table 2). In four cases, prenatal sonography had been performed because of a family history. In the other four cases, hyperechogenic kidneys were picked up by routine sonographic screening and the diagnosis of ADPKD was ascertained because renal cysts were found in parents or grandparents. Oligohydramnios was severe in two cases, moderate in two, and with normal amniotic fluid volume in four cases. There were three terminations of pregnancy and no neonatal death. Four out of five survivors were symptom-free. One had moderate renal insufficiency with systemic hypertension. Nine infants were eventually considered to have another nephropathy (Table 3). The diagnosis was based on histological examination in eight cases and on postnatal Table 4. Cases with hyperechogenic kidneys without precise diagnosis: prenatal data and postnatal follow up. Case GA AF Perinatal outcome Indication for ultrasound Kidney height SD Follow up (months) Creatinine clearance Clinical symptoms Postnatal ultrasound 38 39 40 41 42 43 33 27 24 32 30 37 N N N N PH N alive alive alive alive alive alive routine routine routine routine routine routine 0 1 2 3.1 3 3.5 96 100 72 130 130 67 136 87 125 105 147 97 no diabetes no no no no normal* normal* normal* normal* abnormal** abnormal*** AF ¼ amniotic fluid volume (PH ¼ polyhydramnios, N ¼ normal), GA ¼ gestational age at diagnosis, NN ¼ neonatal. Creatinine clearance was calculated with Schwartz formula (mL/min/1.73 m2). * Transient hyperechogenic kidneys. Hyperechogenicity was confirmed in the neonatal period, but resolved at subsequent follow up. ** Two cysts measuring 10 mm in diameter in each kidney. *** Moderately hyperechogenic kidneys. D RCOG 2002 Br J Obstet Gynaecol 109, pp. 1388 – 1393 1392 V. TSATSARIS ET AL. Table 5. Sonographic features and outcome. Oligohydramnios* (n ¼ 22) Normal or increased amniotic volume (n ¼ 21) Kidney height 4 SD above the mean (n ¼ 17) Kidney height < 4 SD above the mean (n ¼ 25) Oligohydramnios and kidney height 4 SD above the mean (n ¼ 14) Normal or increased amniotic volume and kidney height < 4 SD above the mean (n ¼ 17) Termination of pregnancy Neonatal death Survivors Symptom-free survivors 15 4 11 8 10 3 5 0 4 1 4 0 2 17 2 16 0 14 1 11 1 10 0 9 * Moderate or severe at the time of prenatal diagnosis. ultrasonography in one. At the time of referral, oligohydramnios was severe in four cases, moderate in one, with normal amniotic fluid volume in three cases and with was polyhydramnios in one case. There were six terminations of pregnancy and one neonatal death. Of the two survivors, one developed end stage renal failure and underwent renal transplantation at the age of five. The other one had mild renal failure at six years, with small hyperechogenic kidneys (hypoplastic kidneys). In six children, it was not possible to obtain a precise diagnosis despite careful postnatal evaluation (Table 4). There was no case with oligohydramnios. In every case, neonatal ultrasonography confirmed renal hyperechogenicity, but in four children, renal sonography turned normal at subsequent follow up. Of the four children with transient hyperechogenicity, three remained symptom free and one had diabetes mellitus at the age of 11 months and minor learning disability at eight years. Both children with persistent unexplained renal hyperechogenicity remained symptom free. Overall, amniotic fluid volume and kidney size correlated with outcome (Table 5). There were no survivors among fetuses with kidneys larger than 4 SD above the mean for gestational age and oligohydramnios at the time of diagnosis. Most fetuses with normal amniotic fluid volume and kidneys smaller than 4 SD above the mean survived, the majority of which became symptom-free children. DISCUSSION Our results provide information on the spectrum of renal disorders associated with isolated fetal hyperechogenic kidneys. Prenatal diagnosis of hyperechogenic kidneys may be beneficial to infants, by allowing early recognition and treatment of a renal disease. However, prenatal identification of a fetal renal abnormality may be extremely stressful for the parents and can even be devastating when termination of pregnancy is sought because long term outcome appears uncertain. This prompted us to follow up prospectively all infants referred to our unit because of isolated fetal hyperechogenic kidneys. Increased echogenicity of the renal parenchyma is nonspecific and occurs as a response to different changes in renal tissue1. Interstitial infiltration, sclerosis and multiple microscopic cortical and medullary cysts may account for hyperechogenicity even in the absence of macrocysts1,9. ARPKD, ADPKD and dysplasia are the most common causes for fetal renal hyperechogenicity. However, it is not possible to ascertain the aetiology of fetal hyperechogenic kidneys by ultrasound alone10. The only prospective survey of hyperechogenic fetal kidneys published so far consisted of 19 cases, 14 of which had bilateral increased renal parenchymal echogenicity. Of the latter, there were four with ARPKD, three multicystic kidneys, two hydronephrosis, one renal dysplasia and four ‘false positive’1. In our experience, ARPKD was the leading, but not the sole cause of fetal hyperechogenicity. ADPKD was not uncommon. We were not able to discriminate ARPKD from ADPKD based on prenatal ultrasound. The incidence of ADPKD may have been under-estimated in our study, since the diagnosis can be overlooked in survivors without a family history. Cases with other renal disorders constitute a heterogeneous group. Most of the time, the diagnosis was based on histological findings following termination of pregnancy for severe oligohydramnios and abnormal kidneys. Our most striking finding is that a substantial number of children survived without symptoms and could not be allocated to a precise aetiological group. This reflects the recruitment bias inherent to prenatal screening, which uncovers morphological abnormalities that do not necessarily cause symptoms. It is possible that these children will never develop any disease, which could correspond to the postnatal entity referred to as ‘transient nephromegaly’11 or medullary hyperechogenicity12. Further follow up might also uncover a renal condition later in childhood or even in adulthood, such as ADPKD. At the other end of the spectrum of outcomes were fetuses with severe oligohydramnios, due to anuria and end stage renal failure. Short term outcome was then uniformly poor, regardless of the aetiology. However, these results are biased by the high rate of pregnancy terminations in cases with oligohydramnios. Nevertheless, the three pregnancies that were continued despite oligohydramnios resulted in neonatal death, supporting the concept that D RCOG 2002 Br J Obstet Gynaecol 109, pp. 1388 – 1393 LONG TERM POSTNATAL FOLLOW-UP OF BILATERAL ISOLATED FETAL HYPERECHOGENIC KIDNEYS severe oligohydramnios complicating a fetal nephropathy is an ominous finding. Severe oligohydramnios was documented both in ARPKD and ADPKD, confirming the variability of expression of these conditions13. Apart from these obviously severe cases, it is difficult to predict the long term postnatal outcome of fetuses with renal hyperechogenicity. However, this question is central for couples seeking advice following prenatal diagnosis. So far, prenatal studies focussed in predicting short term outcome2. Because series of renal diseases diagnosed in neonates could be biased towards the most severe cases, we choose to follow up a cohort of patients in whom diagnosis was made prenatally. A relatively long follow up was also required to obviate the most common limit of prenatal studies with a short term follow up, which is to overdiagnose cases as ‘idiopathic’ and to overlook morbidity in infancy. In our cohort, outcomes of children with documented ARPKD or ADPKD were consistent with what would be expected from paediatric series with neonatal diagnosis 5,14,15. However, the proportion of ‘idiopathic’ symptom-free survivors must be kept in mind while counselling parents after prenatal diagnosis of hyperechogenic kidneys. We are currently investigating the potential role of fetal urinalysis or fetal blood sampling to predict long term paediatric outcome or fetal nephropathies, but so far this question cannot be addressed based on currently available literature. In conclusion, our results suggest that prenatal counselling following the diagnosis of isolated bilateral hyperechogenic kidneys should emphasise that establishing the aetiology is difficult, except when renal cysts are found in one of the parents. While patients with very large kidneys and severe oligohydramnios are likely to have a poor outcome, the chances to survive without significant morbidity in infancy are high when amniotic fluid volume remains normal and when the kidneys are moderately enlarged. Acknowledgements The authors would like to thank all the doctors who provided them with postnatal follow up. D RCOG 2002 Br J Obstet Gynaecol 109, pp. 1388 – 1393 1393 References 1. Estroff JA, Mandell J, Benacerraf BR. Increased renal parenchymal echogenicity in the fetus: importance and clinical outcome. Radiology 1991;181:135 – 139. 2. Carr MC, Benacerraf BR, Estroff JA, Mandell J. Prenatally diagnosed bilateral hyperechoic kidneys with normal amniotic fluid: postnatal outcome. J Urol 1995;153:442 – 444. 3. Fick GM, Johnson AM, Strain JD, et al. Characteristics of very early onset autosomal dominant polycystic kidney disease. J Am Soc Nephrol 1993;3:1863 – 1870. 4. Romero R, Cullen M, Jeanty P, et al. The diagnosis of congenital renal anomalies with ultrasound: II. Infantile polycystic kidney disease. Am J Obstet Gynecol 1984;150:259 – 262. 5. Blickman JG, Bramson RT, Herrin JT. Autosomal recessive polycystic kidney disease: long-term sonographic findings in patients surviving the neonatal period. Am J Roentgenol 1995;164:1247 – 1250. 6. Le Guern H, Collet M, Jehannin B, Boog G. Le rein foetal, pathologie, sémiologie échographique et corrélations pré et post-natales. JEMU 1983;4:65 – 71. 7. Chamberlain PF, Manning FA, Morrison I, Harman CR, Lange IR. Ultrasound evaluation of amniotic fluid volume: I. The relationship of marginal and decreased amniotic fluid volumes to perinatal outcome. Am J Obstet Gynecol 1984;150:245 – 249. 8. Schwartz GL. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 1976; 58:259 – 263. 9. Guay-Woodford LM, Galliani CA, Musulman-Mroczek E, Spear GS, Guillot AP, Bernstein J. Diffuse renal cystic disease in children: morphologic and genetic correlations. Pediatr Nephrol 1998;12: 173 – 182. 10. Chitty LS, Clark T, Maxwell D. Perlman syndrome — a cause of enlarged, hyperechogenic kidneys. Prenat Diagn 1998;18:1163 – 1168. 11. Stapleton FB, Hilton S, Wilcox J, Leopold GR. Transient nephromegaly simulating infantile polycystic disease of the kidneys. Pediatrics 1981;67:554 – 559. 12. Howlett DC, Greenwood KL, Jarosz JM, MacDonald LM, Saunders AJ. The incidence of transient renal medullary hyperechogenicity in neonatal ultrasound examination. Br J Radiol 1997;70:140 – 143. 13. Lilford RJ, Irving HC, Allibone EB. A tale of two prior probabilities — avoiding the false positive antenatal diagnosis of autosomal recessive polycystic kidney disease. Br J Obstet Gynaecol 1992;99: 216 – 219. 14. Fick GM, Duley IT, Johnson AM, Strain JD, Manco-Johnson ML, Gabow PA. The spectrum of autosomal dominant polycystic kidney disease in children. J Am Soc Nephrol 1994;4:1654 – 1660. 15. Fick GM, Gabow PA. Natural history of autosomal dominant polycystic kidney disease. Annu Rev Med 1994;45:23 – 29. Accepted 4 September 2002