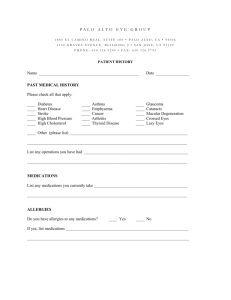
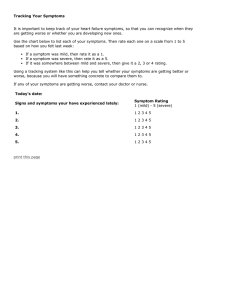
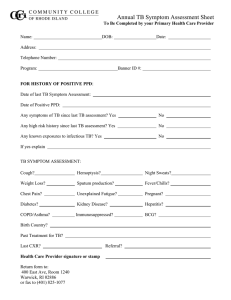
History Taking Jason Waechter 2008 Cardiovascular History The primary symptoms that must be asked about for a CV history include: • • • • • • • • • Chest pain Palpitations Dyspnea (shortness of breath) Syncope and pre-syncope Edema Cyanosis Claudication Fitness capacity Risk factors o For atherosclerosis (4 major ones) o For valve disease (i.e. hx. of rheumatic fever) And of course … • Past medical history (and surgeries) • Family history • Medications • Allergies • ROS (review of systems) For each symptom, apply an organized approach such as is demonstrated in the “generic history taking” approach and flush out as many details as you can for each symptom that is present. For clinical work and OSCE (something-something-clinical exams), you will have to be very good at taking histories and performing physicals. To learn all the different histories and physicals can be an overwhelming task. I am certain that all the information in this handout can be found in any textbook that focuses on physical exams and history taking. I have tried to summarize what I think are the most important and useful points. Because there are many different ways to organize your history and physical, please remember that the method described here is only one of these ways, and it might not suite your particular style. Visit teachingmedicine.com for more learning resources. Generic History Taking There are many different symptoms that you will have to take a history for. There are also many different “systems” (CVS, GI, neuro) that you will have to take histories for. To remember how to take a history for all symptoms and systems is challenging. However, there are commonalities which exist that might make the skill of history taking easier. Not only do you have to obtain information from the patient (or the patient’s family) but you also have to be able to present this information in an organized manner to be able to effectively communicate to other health care members. This “scaffold” summary is only one method for summarizing and organizing this information. Identification (ID): age, gender, occupation, genetic/national background. Chief complaint (CC): what is the main reason the patient is to see you. History of presenting illness (HPI): The following steps must be performed for each and every symptom that you elicit. This is the most difficult part, but can be organized, to a degree: • • • • • • what is going on: patient’s own description of symptom(s) (if symptom is pain, can ask about quality) timing: when did is start is this the first time or has it happened before how fast was the onset (slowly, over days/weeks/months or quickly minutes/seconds/instantly) does time of day influence the symptom (morning, afternoon, evening, night) is the symptom constant (always present) or intermittent severity: how bad is the problem (maybe use a scale from 1-10) impact on the patient’s life, as a result of the problem: • ADL’s (activities of daily living: eating, sleeping, cleaning, dressing) • working, sports, special activities progression: since it has started, is it getting better, worse or staying the same influencing factors: does anything make it better or less severe does anything make it worse associated factors: has you noticed anything else associated with this problem • regional things: anatomically related • systemic things: fever, fatigue, bad sleep, weight loss, medication start • “outside” things: new job, recent vacation, painted my house, new hobby Visit teachingmedicine.com for more learning resources. • • risk factors: has the patient had exposure to risk factors for the symptom • usually, this question requires knowledge regarding risk factors treatment: what tests has the patient had so far • blood tests, imaging studies, specialists visited what treatment has the patient pursued so far • conservative: lifestyle, diet • pharmaceutical: drugs • invasive: procedures, surgery Medications • is the patient on any medications now, or recently stopped any medications Allergies • does the patient have any allergies • does the patient have any drug allergies or bad side effects Past Medical History (PMH) • what medical problems has the patient had in the past important current problems (possibly related or unrelated) should be included early in HPI (diabetes, renal failure, rheumatoid arthritis etc) • what surgeries has the patient had Family History (this is easy to perform, and also easy to forget) • does anyone else in the family have this problem or a related problem • do any diseases run in the family ROS (Review of Systems): • ask general screening questions about all the other systems (CVS, Resp, Neuro etc) Usually, obtaining a history will be a combination of the patient’s agenda of how they want to tell the story and the doctor’s agenda of how they want to ask the questions. It would be very rare for a history to be able to follow such a clearly organized pattern as described above. However, if the doctor is aware of the main questions that should be asked, then hopefully, these questions will, at some point in time, be asked. This list is only a guide and many other questions can be asked. Visit teachingmedicine.com for more learning resources. To illustrate that this format could be used for any symptom, I will demonstrate an example with a completely stupid symptom. This way, it will be easier to apply the scaffold to other, more realistic symptoms, such as pain, diarrhea, difficulty chewing, weakness, rash etc. The example will be a patient complaining of a blue nose. ID/CC: A 33 year old Greek welder presents with a complaint of a blue nose. HPI: Mr. Panagopoulos states his nose turned blue 4 days ago. He has never had this problem before and was completely healthy before it began. The problem was associated with being hit in the face while playing paint ball. The blue coloration developed over a period of 6-12 hours and has not improved over the 4 days since it began and maybe it is getting a little worse. There is no change in the blue color associated with time of day and the coloration has been present the entire time. Nothing seems to make the coloration better or worse that the patient can think of. He says that the color of his nose embarrasses him and he refuses to go to work. The patient thinks that the color of his nose is quite severe. However, he has no problems sleeping, eating or doing chores around the house. The patient reports that his nose is painful, swollen and stuffed up. He also says that he has a runny nose at times since this began. He denies other symptoms regarding any other part of his body and he has had no other changes in his life that are associated with this problem. <I do not know any special risk factors for a blue nose, so these questions are not asked> He has not pursued any treatment so far and has not seen any other doctors for this problem. PMI: The patient has no significant past medical problems Allergies: No drug allergies. No other allergies Medications: None Family History: Both parents are alive. Father had a heart attack 3 years ago. Mother is healthy. Siblings are healthy. Grandparents all passed away, 1 from cancer, 1 from old age and 2 from unknown causes. There is no family history of persons having a blue nose. After you finish writing the history in the chart, next write the physical, investigations, impression and plan. Some people use “SOAP”: subjective, objective, assessment, plan. Hx Px Investigations Imp. Plan or Subjective Objective Assessment Plan Visit teachingmedicine.com for more learning resources.