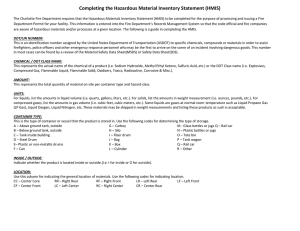
C ase 6 Health Management Information System for Integrated Delivery of Public Health Services in Tamil Nadu— A Success Story Dr S Vijayakumar The Health Management Information System (HMIS), Tamil Nadu, is the first centralised web-based HMIS solution in a state covering 276 secondary-care hospitals, 1,539 primary healthcare centres, to be expanded shortly to the 46 tertiary care institutions and 19 medical colleges. Each hospital in the state has an independent Health Management System (HMS), which is linked to the state-level HMIS. This makes real-time data available across 276 secondary care hospitals in 32 districts centrally. This data is used for planning healthcare, managing drug inventory, and planning health initiatives at the state level. There are no data entry operators employed in the whole project. The doctors themselves enter diagnosis, order lab tests, and give prescriptions online for all out-patients. The system stands apart in its comprehensiveness as it consolidates state-level data, links all health institutions, and makes it possible to track individual health indices anywhere in the state through a unique patient identification number. Introduction The government of Tamil Nadu has pioneered many new approaches to enhance effective access to quality health care at low financial cost. This article presents the experiences of Health Management Information System 113 the Tamil Nadu Health Systems Project, Department of Health and Family Welfare, in the installation and operation of health management information system in the state. The Situation Before Introduction of HMIS Prior to the introduction of Health Management Information System (HMIS) in the state, the information generation and communication remained, by and large, manual in nature. The problems were many. Following are some of the concerns/gaps in proper health administration prior to the introduction of HMIS: i. Inefficient delivery of health services: The delivery of health services in the hospital was not efficient. Patients’ health could not be tracked, they were sometimes prescribed medicines that were out of stock and there were gaps in the quality of service. ii. Lack of standardisation of health data: All hospital records were maintained manually, which was time consuming and a lot of time was spent in retrieving records. More funds were spent towards manual registers, which were difficult to maintain. Lack of standardisation, incomplete data, and poor understanding of formats were the major deterrents for healthcare practitioners. The data was provided for ad hoc requirements and as per needs of various monitoring agencies and varied. In-patients’ diagnosis was not being mapped to the International Classification of Diseases (ICD)-10 that is recommended and followed worldwide. iii. Costly maintenance of books: The government had been spending more funds in procurement/printing of manual registers and storage of large volumes of books/ registers/records. iv. Duplication of data entry, data retrieval, and reliable information: Same data was being entered at various levels—for example, patient details were entered at registration, nurses record, doctor record, etc. Reliability of the collated data could not be ensured and reconciliation was difficult. Eighteen directorates under health department required regular information. The number of copies of reports sent from the institutions to district and state-level authorities was high—for example, almost 18 copies of each report were made and some of these reports had to be consolidated at the district level for dispatch to state level for further consolidation. No records were maintained at hospitals for outpatients prior to HMIS implementation. v. No real-time data: For analysis of healthcare data, reliability of the data was questionable. The ready availability of data for consolidation and manual collation, etc., was prone to errors. Real-time data of transactions at the hospitals was unavailable at the institutional, district, or state level for decision making. There were no snapshot/dashboard views available to monitor the performance of the hospitals, prior to the introduction of this system. 114 Driving Process Change: Innovative e-Government Practices from India vi. Poor equipment maintenance and drug supply chain management: No consolidated equipment and drug inventory was available. Monitoring of equipment downtime, drug stocks auto indent, drug stock accountability, and monitoring for drug expiry dates were some of the other challenges the health system faced. It was felt at various levels that there was a need for comprehensive and IT-enabled information system to address these issues. The HMIS was therefore conceptualised to realise this long-felt need of putting in place a system that helps in promoting evidencebased management of healthcare. Given the above scenario and guided by the objective of improving the efficiency of the healthcare system in Tamil Nadu by leveraging technology, rationalisation of some processes, inputs, and reports has been affected. This has led to the removal of many manual processes including manual tokens for drugs, lab request slips, indent forms, etc., and automation of periodic reports on drug issues, indents, daily census, etc. This has resulted in substantial saving of time for the end-users. It has reduced data entry effort with direct export of required data to NRHM portal, and capture of patient data for NCD programme for easier tracking and follow-up of patients. Introduction of IT in Public Health Systems The expanding public health system makes administrative decisions complex. The manually maintained communication systems pose many challenges to the administration of health initiatives in the state. The international funding is increasingly used by the health department for various projects that need an efficient information system. For many years, the need was felt for a comprehensive information system that could address the information needs of policy makers at all levels at a cheaper cost. HMS at all the 276 Hospitals in 32 Districts Hospital Management Systems (HMS) was deployed across the 276 secondary care hospitals to streamline their functioning by automating processes and aiding proper management of data. The services covered for hospitals as part of the HMS comprise 10 modules including Registration (outpatient, inpatient, casualty), Lab services, Pharmacy, Stores, Wards, Blood Bank, Linen management, Diet, Biomedical Waste Management, Equipment Inventory and Clinical Module covering patient Outpatient (OP) record, In-patient (IP) record, Nurses notes, Operation notes, discharge summary, Ante Natal Records (ANC) record, Natal & Post Natal record, Family welfare services, and Referral services. Health Management Information System 115 State-Level Health Management Information System HMIS is implemented with the objective to serve multiple users with a wide array of purposes that can be summarised as the generation of information to enable decision-makers at all levels of the health system to identify problems and needs, make evidence-based decisions on health policy and allocate/utilise scarce resources optimally. HMIS covers not only the clinical part of health systems but also reporting on other aspects such as administrative, personnel, ancillary services, and programme management for a hospital. The clinical records that are captured under the HMS are automatically incorporated into the HMIS Figure 1: Tamilnadu Health Systems system, thereby avoiding the need to re-report the Project clinical data. Further, HMIS aims to (i) promote the migration from paper-based to an electronic health record information structure that would enable the health care providers and beneficiaries easy access to information and health care respectively; (ii) ensure that integration of institutional and personal health information and medical records are managed effectively so as to ensure access to good health care; (iii) deliver measurable cost and quality results from improved information management in health care; and (iv) convert granular data to information for decision making. The HMIS addresses the information needs at individual as well as health facility levels. In the individual level data, the HMS captures the patient’s profile, healthcare needs, and treatment, which serve as the basis for clinical decision making. Computerised health care records provide the basis for continuum of care. This ensures minimisation of manual data recording and easy retrieval of patient data. In the health facility level data, it facilitates the capture of data at the point of care. The HMIS is providing critical health data across the health chain for quick and timely intervention by health directorates. The HMIS captures data from both aggregated facility-level records and administrative sources such as drug procurement records, enables healthcare managers to determine resource needs, guides purchasing and distribution/deployment for drugs, equipment and supplies, manpower, etc. 116 Driving Process Change: Innovative e-Government Practices from India This has enabled institutions as well as the health administration to improve supply chain management of essential drugs, build a robust equipment management system to manage and monitor functioning of critical equipment and reduce down time through systematic tracking. The following services are covered as part of HMIS: i. Online registration of outpatients and inpatients ii. All out-patient services including doctors’ consultation, lab and pharmacy services. Doctors’ services for outpatients including clinical findings, diagnosis, prescriptions and lab requests entered online (real time) iii. In-patient services including diet, linen management and discharge summary iv. Blood bank and bio-medical waste management v. Drug inventory vi. Equipment management system vii. Human resources management viii. Health data reporting HMIS: Planning and Implementation Strategies The HMIS was planned to be introduced in a phased manner and initiated by a pilot project that was implemented in five secondary care hospitals during October 2008. After the successful implementation of the pilot, the next phase of implementation was carried out in five districts covering 38 hospitals from March 2009. Subsequently, in Phase II, the HMIS component was implemented across all primary care and secondary care institutions covering 276 hospitals and 1,600 Primary Health Centres (PHCs). Figure 2: Registration of outpatients, Padmanabhapuram. Health Management Information System 117 Figure 3: Doctor consultation, Padmanabhapuram. The HMS component covers all the 276 hospitals across all the districts in the state. The HMIS is an online reporting system that comprises four modules, namely, Clinical, Ancillary, National Programme Information, and Administrative Information System. i. The clinical module comprises OP, IP census and details of maternal, child health, immunisation details, family welfare services and disease-wise data of treatment and cases, etc. ii. The programme information module covers the national-and state-level programmes like Blindness Control, Malaria, TB, Infectious diseases, School Health, etc. iii. The ancillary module includes reporting forms for blood bank services, laboratory services, stores/inventory details for drugs and other consumables, diet details, and biomedical waste management. iv. The administrative information system module contains finance-related forms for budget, etc., and infrastructure related forms, including buildings, equipment, vehicles, etc. This module also comprises establishment related forms for capture and reporting details of all the health department personnel including transfers, training, leave, etc. The strategies adopted to bring about the transformation and smooth transition from manual maintenance of records/register to a simple and efficient IT-enabled module are listed below: i. The project was conceptualised as a centralised web-based software solution to minimise technology support and maintenance dependencies. ii. The end-users across various institutions and offices were involved in finalising the software requirement specifications, so that the entire application was customised to suit the needs of 18 departments in the health sector. This helped to a greater 118 Driving Process Change: Innovative e-Government Practices from India Figure 4: Pharmacy–issue of medicines, Padmanabhapuram. iii. iv. v. vi. vii. viii. ix x xi xii xiii. extent in fulfilling the expectations of all stakeholders—a kind of motivation for them to support its substance. Use of open source software stack as it had a lower cost. At the same time, proper support was ensured to overcome issues of using open source software. Extremely simple, user-friendly screens designed and optimised for performance by application provider to ensure end user ease of use. Adequate training for the end-users at the institutional level, to ensure their full participation and to increase their comfort level. The line department officers visited each of the hospitals during the induction training programme that was conducted over 3–4 weeks at each hospital. Handholding during the initial roll out was helpful in addressing the resistance to change from traditional practice. Use the connectivity offered by Tamil Nadu State Wide Area Network (TNSWAN) for a secure bandwidth for data transfer. Provision of redundant connectivity using VPN over Broadband. Co-location of the central servers at the State Data Centre to utilise the existing investments by the state’s IT department Issuance of necessary Government Orders (GO’s) to facilitate mandating the use of online system as well as removal of manual systems Around 5,000 hospital staff members have been trained and are using the online system, which includes hospital staff from PHCs. Appointment of trained skilled IT team to coordinate and troubleshoot problems in IT infrastructure—one person in each district Establishment of a central helpdesk to coordinate and follow up with vendors for IT infrastructure installation, management and trouble shooting Health Management Information System 119 xiv. Continuous monitoring by the top management and periodic reviews of the performance of the hospitals on HMS at the Directorate-level ensured that the implementation was a success. The other process initiatives include: i. Stakeholder meetings Periodic reviews Follow-up on action points ii. Help desk set up Central helpdesk Protocol established iii. IT coordinator placed in each district Coordinate all infrastructure issues related activities Application support and training to end users as needed iv. Basic computer skills training through TNeGA v. Motivation to end users—written appreciation for good usage of online support—by Project Director; Director of Medical Services vi. Hospital/District level process Daily online usage monitoring e-nodal team set up at each hospital HMIS part of quality circle meeting agenda for review Process Change Guided by the objective of improving efficiencies at the global level and leveraging the prolific presence of technology, rationalisation of some processes, inputs, and reports have been done. This has led to removal of many manual processes including manual tokens for drugs, lab request slips, indent forms, etc., and automation of periodic reports on drug issues, indents, daily census, etc., resulting in substantial savings of time for the end users. Grassroot level study of information requirements and processes has facilitated the design of uniform and standardised input formats and processes. Common uniform system of reporting will ease data comparison and performance monitoring across institutions. Proactive Health programmes can now be tailored to meet local challenges. Role of Top Management in Planning and Implementation of HMIS The role of top management has been critical to the success of HMIS implementation. Certain responsibilities included: 120 Driving Process Change: Innovative e-Government Practices from India i. Set project expectations: In the planning stage, the Government of Tamil Nadu and the team of HMIS carried out an analysis of the project and developed a strategic plan to accelerate implementation by ensuring participatory consultation with key management teams. ii. Set the cultural tone for systemic change for the project: For instance, for project-related activity, e-mail communication was made mandatory and paper communication was banned. A helpline was set up to help and ensure seamless usage of IT. At the behest of the Director of Medical and Rural Health Services facilitated by TNHSP, the state government has supported this project by way of issuing government orders (GO) for doing away with manual registers and making full use of HMIS application. This has been an important policy decision and a significant step in change management. The GO also advised the audit department on the auditing process. iii. Lead the vendor management process: An accelerated vendor selection process was developed that followed the state’s transparency guidelines. During the roll out of the project, the nominee played a very important role as a catalyst in bringing multiple vendors and other stakeholders together for periodic review of the progress in implementation of the HMIS to address bottlenecks across the table. The sheer size and spread of the infrastructure was daunting, given the stringent timelines involving procurement, installation, commission of over 15,000 desktops, connectivity, power back-up through UPS, 500 printers and installation of LAN at each hospital as well as the setting up of the server at the data centre that called for strong programme implementation and monitoring capabilities. This was ably demonstrated by constant reviews and quick decisions to address bottlenecks. There was continuous motivation of the health administrators for change management on the one hand and addressing vendor-specific issues during the reviews on the other. HMIS involved multiple vendors in the combined periodic reviews that helped in addressing gaps and in speeding up the processes. iv. Lead communication efforts (with physicians and nurses): The project actively engaged with physicians and other clinicians to design and implement HMIS. The author ensured in his capacity as Special Secretary, Health the involvement and support of the top management from the 18 health directorates, which was critical in the successful acceptance and deployment of the IT application. v. Human capital development (critical for change management): It was felt that physician leadership is a critical success factor for health information technology initiatives. Dialogue was also initiated with reputed academic Institutions (Tata Institute of Social Science (TISS)/National Institute of Engineering (NIE)) to assess further training needs of the health professionals. The author has been able to design the training programmes for public health professionals to provide them opportunities for higher level of learning and motivation. He also ensured that basic computer training was given to all the hospital staff with the help of Tamil Health Management Information System 121 Nadu e-Governance Agency (TNeGA). The doctors themselves use the system to enter diagnosis, order lab tests and give prescriptions online for all outpatients. No data entry operators were deployed and the end-users were empowered for on-line usage. As a result, manual records are not maintained any longer. Around 8,000 hospital staff members have been trained and are using the on-line system. Apart from the health professionals, a pool of IT-skilled professionals was created to assist and handle IT-related issues both at the hospitals and at the HQs for server management. All these initiatives were carefully streamlined into the mainstream health administration to ensure continuity of support. vi. Create HMIS implementation plans and training modules: The project published guidelines covering many facets of HMIS/HMS practices. Many of the guidelines are aligned with the national priorities of building the capacity of information management and sharing at various levels. For example, the HMIS Manual/practice guideline ‘Core Data Sets for the Physician Practice Electronic Health Record’ clearly indicates the nominee’s commitment in understanding the importance of core data sets and insisted discipline across all levels in adhering to the manuals. These guidelines provided domain-specific best-practice principles for health care professionals to succeed in the transition to an electronic healthcare environment. vii. Adoption of health information standards for inter-operability of health information: The author promoted the introduction and use of standards (such as ICD-10, standardised drug/lab codes) and this transition brings tremendous benefits in patient management in the long run. Salient Features of HMIS The salient features of HMIS have been listed below: i. Transparency and stakeholder participation: The implementation of HMIS involved multiple stakeholders including IT infrastructure vendors. Vendors provided hardware, infrastructure, furniture, training, civil work, networking, connectivity, data centre hosting, etc. The other health department stakeholders include the Director of Medical and Rural Health Services, Director of Public Health, Tamil Nadu Medical Services Corporation, ELCOT, etc. In order to effectively implement the project, it was critical that the different stakeholders be actively involved in the processes during the implementation phase. During progress review, the issues were immediately addressed across the table as all the stakeholders involved in the implementation of HMIS were part of the reviews. The end users across various institutions and offices were called upon for finalising the software requirement specifications, so that the entire application was customised to suit the needs of each and every department. Extremely simple, user-friendly screens were designed by application provider to ensure end-user’s 122 Driving Process Change: Innovative e-Government Practices from India ease and optimised performance. The customisation was made based on the requirements of the end-user; for example, the medical officer at the hospital could customise drug combinations for general illness so that during consultation, he/she could prescribe the drug with one click. Stakeholder participation in all stages of the project was the major reason for the least resistance in the IT implementation in the project. Involvement and participation of all stakeholders including the end users is ample proof of the openness and transparency prevailing in the implementation of the IT-enabled healthcare administration. ii. Innovative and replicable: The HMIS is based on unique identifiers for each hospital, patient, and institutional user. This provides for patient referral across the health chain. HMIS is an idea that has been designed to improve the process and services in the health system by using information technology. The project uses a centralised server model instead of a client server model, which enables inter-hospital retrieval of patient data. This web-enabled system, built on open source software, captures real time clinical data of patients from 276 hospitals across all districts of Tamil Nadu. While TCS provides the software solution support, the connectivity is provided by Electronics Corporation of Tamil Nadu using a 2 mbps dedicated leased line at every hospital. Thereby, this system was successfully deployed across all hospitals, independent of the volume of patients handled by them. The simplicity of the interface enables the use of the application directly by the end-users. The centralised web-based solution developed using open source technologies addresses issues like costs associated with vendor lock-in for proprietary databases, etc. The end-user systems work on Linux Operating system that has also proved to be cost-effective, keeping them free from virus as well as savings on cost of procurement of antivirus software as is required for other OS till date. The use of open source software has led to significant reduction in cost of procurement even of Server Hardware as many standard proprietary databases are highly resource hungry and will disproportionately increase the cost of ownership by increasing the hardware requirements and license fee for each installation including high maintenance costs. The design caters for possible pain-points that could arise at operational level due to factors like remote location of the hospital, lack of trained manpower at hospital, operational exigencies, etc. The solution is driven by low cost of support, ease of deployment, training, etc. HMIS data entry formats are fully standardised and provide for uniformity in reporting and data consolidation. Data input and collection in forms includes the data requirements for National Rural Health Mission (NRHM) and other reporting needs at state and central level. Integration and inclusion of programme initiatives like NRHM and NCD as part of the application design has brought in several benefits. It has also provided the health administration with required reporting facility. Health Management Information System 123 Results The following is the outcome expected from and delivered by the initiative: i. Evidence-based planning, financing, research, and policy formulation is ensured. ii. Workflow at all 276 secondary care hospitals has been standardised and streamlined. iii. The demographic details and clinical records of 1,48,51,390 patients are available in the database and can be retrieved on demand across all government hospitals in the state. Real-time records are available from all secondary care hospitals. iv. 62 per cent of the patients bring back the Patient Identification Number (PIN) to the hospital during subsequent visits. They have realised that they need to bring only the PIN and need not carry all previous records with them. v. Doctors in all the hospitals have been trained and are comfortable with the online system for documenting clinical findings and prescriptions. vi. Management of drug inventory and equipment inventory has improved. Moreover, a large section of the manpower used in the process of data compilation and reporting is now available for other essential medical services. vii. Unique PIN. viii. Unique institution codes across all government hospitals and offices. ix. Unique employee numbers/user names and passwords – for access to system. x. Standardisation through reuse of drug codes (from central procurement agency) and treasury codes for finance-related information. xi. Uniform reporting platform across all state government health facilities with standardised reporting formats across all institutions for better data consolidation, comparison, and analysis. xii. Facility to link patient’s record with UID, once it is made operational by Government of India. xiii. Auto integration with national-level data pool. xiv. Lab test results are being given to the patient with test report reference values. xv. The final diagnosis is linked to International Classification of Disease Code-10. The system can be easily replicated in any other state as most of the reporting indicators are compliant with the Government of India (GoI) reporting formats. Processes and Effectiveness of Outcomes The solution has been designed in such a way that the system automatically incorporates data at the institutional level with clinical data from HMS and auto populates the HMIS reporting fields, thereby minimising considerable amount of effort in terms of reporting and consolidation. HMIS is a solution that encompasses technology, procedures and people with a focus on providing timely and accurate information to manage at the operational level and aid 124 Driving Process Change: Innovative e-Government Practices from India decision making at the policy level. This solution aims to increase process and quality outcomes and decrease inefficiencies and costs. This would help control administration costs and maximise efficiencies of available resources. The huge cost involved in the procurement of records and registers are now being curtailed and a more cost-effective system is put in place. This project was cost effective when compared to other similar projects of this size and scale. This was possible because of various reasons—use of open source software, rationalisation of hardware/equipments, no additional manpower for data entry, capacity creation within the hospital, increased productivity and centralised system curtailing costs of maintenance at the hospital level. Review of hospital performance has become easier as the CMO can view staff performance and distribution of patients among the medical officers, pharmacist, lab technician, and nurses. Institutions’ performance review and monitoring are possible as it has been built as a part of HMIS that can give a snapshot view of the capacity of the hospital and utilisation of services. Out-patient (OP) and In-patient (IP) statistics, rationalisation of manpower, etc., is possible with HMIS. The system is open and is capable of being linked with larger systems when there is such a need. All these characters make these initiatives capable of creating transformational effect in the health sector and the initiatives have the potential to be sustainable, scalable and replicable. Impact of HMIS HMIS has brought about a significant reduction in the time taken for delivery of services and the time spent by a patient in the hospital. The patients who are already registered do not have to wait in long queues every time they visit the hospital as was the practice before the introduction of HMS. The patients can now go directly to the respective OP department to meet the doctor. The doctor is able to retrieve the patient’s records using the unique patient number and enter the details. Doctors can view all previous history of the patient including treatment, medication and investigations done. Table 1: Impact of HMIS Indicator Before HMIS After HMIS Citizens Waiting time in the queue Every visit at the OP registration Spends about 15 minutes counter approximately 30 minutes during the first visit, on subsequent visits does not have to go to the OP registration counter (Contd.) Health Management Information System 125 (Contd.) Collection of lab results Where the patients were asked to The patient can collect the come back to meet the doctor for results the next day itself. follow up visits after 3 days, the patient had to come back to the lab to collect the results the next day and on the third day for the follow up visit Medical Officers Time spent on writing Separate tokens written for drugs, Pre-designed packages for prescriptions and lab orders lab orders and treatment prescription and lab requests help doctor complete it with few clicks Review of patient history Patients had to bring their old during the visit records during the visit for the doctor to review. No documents at the hospital regarding treatment given to the outpatients at the hospital level Consolidation of diagnosis All records available on the computer—doctors can view entire patient record— better patient management. Patients need to bring the PIN number only. No data available on OP treatment Diagnosis and prescription pattern pattern available Nurse Day-end statistics consolidation of 1 hour for injections for OP alone Drug indenting for IP cases 5 minutes 20–30 minutes 5 minutes 3 hours 10 minutes 15 minutes 5 minutes 2 hours every day 5 minutes every day 2 days 15 minutes 4–5 hours 15 minutes Census report 1 day 10 minutes Stock report for stores 2 days 30 minutes Diagnosis-wise report 3 hours 5 minutes Drug inventory Diet/linen indenting Pharmacist Consolidation of stock issue report day-end Indenting drugs and reporting at the end of the month Stock check for expiry Report preparation 126 Driving Process Change: Innovative e-Government Practices from India The HMIS has brought about significant impact in the delivery of health services to the citizens. The doctors find the system very useful for patient care. The availability of data helps them in observing trends. The doctors, for example, get online alerts for drugs that are not available in the hospital pharmacy, or if the patient is currently on medication prescribed by any other doctor in the system and in general, keeping track of the patient history. The nursing staff finds the system useful for preparing reports, inventory management, diet orders, etc. The patients can now visit any secondary care hospital in the state with the Patient Identification Number (PIN) and his/her case records can be accessed by the treating physician. i. Real time data is available for closer monitoring and decision making on staff deployment, utilisation of resources, etc. This can be used to understand the trends and patterns accurately. ii. The time spent on consolidating the monthly reports has come down drastically. The consolidated reports are available readily. With HMIS, each administrative unit can view the reports online; this has helped do away with the system where monthly consolidated reports were required to be sent to several agencies. iii. Reporting compliance by institutions is easier. Defaulters are closely tracked and held accountable during review meetings. iv. Validation of data elements at the time of data entry has significantly improved the accuracy of data reported. Missing data elements and report tracking is also made easier through online system. v. Institutional Performance Report and identified periodic reporting forms currently at 100 per cent compliance due to close monitoring and follow up by the health administrators. vi. Periodic and monthly reports that are to be sent to NRHM are directly exported from HMIS online; there is no consolidation or data entry. vii. Manpower rationalisation based on performance, utilisation, etc., is possible. For instance, work load of the medical officers can be calculated. Figure 5: Total Registration of patients 2010–2012. Health Management Information System 127 One of the important measurable outcomes of HMIS is based on the observation that around 60 per cent of the registered patients bring back the PIN (Patient Identification Number) during their subsequent visits, which shows high patient compliance with this system. The HMIS has significantly contributed to the simplification of processes that were hitherto very cumbersome and time consuming. The discharge summary is autopopulated and ready at the time of discharge. Most importantly, a printed discharge summary (that is readable!) is ready at the time of discharge of the patient. The patient does not have not to wait or come back to collect the discharge summary. Another example of improved efficiency and process simplification is that in-patients’ diet can be ordered over the system by the ward in-charge for all inpatients based on their dietary requirement. Before introduction of this system, the diet staff had to go to each ward and collect the diet request forms. HMIS has done away with manual system of drug indenting. The staff nurse in-charge of the ward places the orders over the system. State Health Data Resource Centre (SHDRC) The SHDRC is planned as a comprehensive repository of health information across all directorates and departments integrated in a single platform. IT enablement of hospitals in Tamil Nadu’s districts creates an accurate real time database that can be used as a basis of timely information for drawing up health-related policies and budgets by the state bureau. The data gives insights such as the main ailments in the state, most common drugs prescribed, lab usage pattern, district-wise health indicators, etc. This initiative strives to strengthen the patient and hospital databases such that they ably support the strategic management of health system of the state. Easy access to epidemiological data about individual patients enables proactive and efficient management of communicable and non-communicable diseases. This is very effective and result-oriented during the eventuality of an epidemic. Early intervention and swift response by the health directorates, guided by accurate information would aid in handling emergencies and such other situations. Towards Sustainability The HMIS has demonstrated the integration of departments in providing cost-effective and sustainable IT solution to public health services. To ensure sustainability, policy-level steps were initiated through the health department. The budget (recurring expenditure) needed to run this project is factored in during the annual budgeting of the respective directorates. The state IT department maintains the hardware/software through its Annual Technical Support plan. A major portion of the cost for network connectivity is assured as the project depends on the state IT infrastructure and TNSWAN for hosting and connectivity. The central servers are co-located at the State Data Centre (managed 128 Driving Process Change: Innovative e-Government Practices from India by the IT Department). This ensures sustainability of HMIS at least cost. This also serves as a model for other departments of the state government to make better use of existing IT infrastructure of the government. Figure 6: Pictorial representation of the HMS and HMIS.