Therapeutic Modalities

Therapeutic Modalities
Sports Medicine
●
●
●
●
●
●
●
Terminology review
Acute-the result of a specific impact or traumatic event that occurs in one specific area of the body, such as a muscle, bone, or joint
Chronic-the result of prolonged, repetitive motion that is particularly common in endurance sports such as swimming, running and cycling
○ Also known as overuse!
Hard tissue-injury to the bones
Soft tissue-injury to the ligaments, tendons, or muscles.
Direct-injury sustained by an external force
○ Ex: hit by a ball, bat, person.
Indirect-caused by an internal force within the body
○ Sprains and strains are always classified as indirect injuries as an external force does not cause tears in ligaments or muscles.
New terms:
○
○
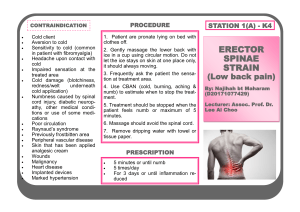
Indications-a reason to use a certain treatment
Contraindications-a condition or factor that serves as a reason to withhold a certain medical
Inflammation
• Pain
• Swelling
• Redness
• Heat
• Loss of function
Modalities
• Modalities are physical agents that produce a specific therapeutic response.
• Include: heat (superficial and deep heat), cold, sound, electricity, mechanical forces and light.
• Used to control the inflammation process
(not stop it)
• You should understand what the modality will do to the body prior to use
Gate Theory for pain control
• If you stood up and hit you head what would you immediately do?
• Each nerve can either sense “touch” or
“pain”
• When you stimulate the touch part of the nerve…you close the pain channel
• When you rub your head you feel the rubbing instead of the pain
Purpose
● Muscle Spasm/Pain Cycle ~ injury causes muscle spasms that cause pain that causes muscle spasms
○ Leads to decreased mobility
● Therapeutic Modalities used to stop cycle
● Misapplication can make injury worse
Pain Spasm Cycle
• Bodies natural reaction to an injury is to cause the surrounding structures in spasm o Natural splinting of the body
• Spasm most powerful for of contraction (100%)
• Problem o o o
Injury causes spasm
Spasms hurt
Pain causes spasm o Spasms hurt
• Through use of modalities you can either stop the pain or the spasm
Choosing a Modality
● Is modality safe for this type of injury?
● Will modality contribute significantly to rehab process and complete recovery?
● Is person applying modality trained to use it?
Heating and Cooling Means
●
●
●
Conduction~ heat transfer by direct contact with another medium. (hot or ice packs)
Convection~ heat transfer by indirectly through secondary conductive medium. (air or liquid)
Radiation~ heat transfer by or from its source to surrounding environment in form of waves or rays. (ultraviolet light)
Heating and Cooling Means
●
●
Conversion~ heat transfer that takes place through other forms of energy, such as sound, electricity or chemicals.
(Ultrasound, diathermy)
Evaporation~ heat transfer takes place when a liquid coverts into a gas.
(perspiration)
When to use Ice or Heat
• Ice o First 24-72 hours post injury almost always use cryotherapy to control the inflammation process
• Heat o o o
Before rehabilitation exercises
▪ Especially ROM exercises
Before exercise
Later stages of injury treatment
Heat Therapy
• Moist Hot Pack (160 degrees for 20 minutes)
• Warm Whirlpool (100-110 degrees for 20 minutes) o Over 120 is scalding
Effects of Heat Therapy
• Immediate Vasodilatation o Increase blood flow
• Increases tissue Elasticity o Increase ROM
• Counterirritant for pain o Decrease Pain
Cryotherapy
• Application of any cold therapy
• Ice bag (20 minute treatment time)
• Ice massage (15-20 minute treatment time)
• Cold Whirlpool (50-55 degrees for 20 minutes
• ***Water based cryotherapy cannot cause cold injuries (frostbite)
• ***People may be allergic to or have adverse reactions to cold
Effects of Cryotherapy
• Immediate Vasoconstriction o Decreases blood flow o Decreases swelling
• Decreases tissue elasticity o Decreases ROM = protect the injury
• Counterirritant o Decrease pain
• ***ice does not “numb” the area
Cryotherapy
● Treatments using Cold
● Decreases tissue temperature
● Skin Color change from white to red
● Decrease in total blood flow
● Decrease in nerve conduction
Cryotherapy Treatment Length
● Average 15-20 minutes, once an hour
● Three phases of sensation:
○ Cold sensation lasting 0-3 minutes
○ Mild burning and aching lasting 2-7 minutes
○ Relative numbness lasting 5-12 minutes
Guidelines for Cryotherapy
●
●
●
●
●
Use of a barrier, except in ice massage
Never on anesthetize skin
Never on open wounds
Never on someone with desensitized skin
Monitor for signs of Raynaud’s Phenomenon , condition in which the arteries and arterioles of an extremity constrict extensively. Causes extensive arterial blood flow.
Cold Packs
Indications:
○
○
○
○
○
○
○
Acute trauma
Acute Pain
Heat Illness
Muscle Fatigue
Spasms
Post-op Pain
Acute Edema
Contraindications:
○
○
○
○
○
○
Circulatory insufficiency
Cardiac Problems
Open wounds
Anesthetic skin
Hypersensitivity to cold
Raynaud’s Disease
Clinical Application of Ice Pack
● Directly to injured area
● Frequency should be 20 minutes for every waking hour in acute injuries
● No longer than 20 minutes (veins begin to vasodialate to warm body)
● Used primarily for the first 48-72 hours of an injury
Typical Response to Ice Pack
● Cold → Burning → Aching → Numbness
○ Numbness takes from 3-7 minutes
● Treatment usually satisfactory when skin turns pink or red
Ice Massage
●
○
○
○
○
○
○
Indications:
Acute Trauma
Acute Pain
Muscle pain/spasm
Post-op pain
Heat Illness
Acute tendonitis
●
○
○
○
○
○
○
Contraindications
Circulatory insufficiency
Cardiac Problems
Open wounds
Anesthetic skin
Hypersensitivity to cold
Raynaud’s Disease
Clinical Application/ Responses
● Ice should have round edges
● Continuous movement of ice to prevent tissue freezing
● 5-10 minutes, 4-6 times a day
● Cold → Burning → Aching → Numbness
○ Numbness takes from 3-7 minutes
Cold Whirlpool/Ice Immersion
Indications:
○
○
○
○
○
○
Acute Trauma
Acute Pain
Muscle pain/spasm
Post-op pain
Heat Illness
Acute tendonitis
Contraindications
○
○
○
○
○
○
Circulatory insufficiency
Cardiac Problems
Open wounds
Anesthetic skin
Hypersensitivity to cold
Raynaud’s Disease
Clinical Application
● Frequency of treatment is 20 minutes
● Cool = 67º - 80º F . . Use for spasticity
● Cold = 55º - 67º F . . Use for inflammation and acute injury
● Very Cold = 33º - 55º F . . Use for acute injury and pain relief
● Encourage athlete to work on ROM while in the whirlpool or cold bath
Typical Reactions
● Athlete will usually be uncomfortable and not want to do treatment
● Cold → Burning → Aching → Numbness
○ If water is constantly moving, athlete may never achieve complete numbness
Contrast Bath
● Theory is that the cold vasoconstricts the veins and the heat vasodialates the veins creating a pumping motion to push edema out of the area
● Indications and Contraindications same as those for Thermotherapy and Cryotherapy
Clinical Application
●
●
●
●
●
○
If swelling is anticipated end in cold
Work to ending in hot
Hot water should be 95º-110º, and cold water should be 55º-65º
Encourage athlete to work on increasing
ROM
Use a 2:3 ratio of cold to hot or hot to cold
Treatment should last between 20 and 30 minutes
Thermotherapy
● Treatments using heat
● Increase the temperature of the body region to cause vasodilation
○ Increases blood flow to area
● Decreases pain and muscle spasms
● Increasing flexibility to tissues
● Comforting for most patients
Guidelines for Thermotherapy
● Never apply to an area of decreased sensation
● Never apply directly after injury
● Never apply to eyes or genitalia
● Never apply to a pregnant belly
● Never apply over an open wound
● Do not apply on pts with hx of diabetes
Moist Heat Packs
●
○
○
○
○
○
Indications
Chronic
Pain/Tendonitis
Lg jt. Contractures
Muscle Spasm
Chronic edema
Pre-heating to electrical stim tx
●
○
○
○
○
○
○
Contraindications
Existing fever
Cardiac irregularities
Decreased skin sensation
Infections
Active Bleeding
Acute inflammatory conditions
Clinical Application
● Pack should be applied with several layers of towels or hot pack cover
● Hydrocollator water temp = 170 degrees
● Treatment time varies as indicated
● Never lie or sit on hot pack due to increase in burns
Typical Reactions to Hot Pack
● Feel comfortable warmth
● Sensation of area relaxing
● No sensation of burning should be felt
Paraffin Bath
●
○
○
○
○
○
Indications
Chronic Pain
Muscle Spasms
Chronic Edema
Chronic arthritis
Soften calloused hands
●
○
○
○
○
○
○
Contraindications
Existing fever
Infections
Hypertension
Acute inflammatory injuries
Wet hands/fingers
Open wounds
Clinical Application and Response
●
●
‘Glove hands’ with wax, frequent dip
Follow individual manufacturer directions
●
●
●
●
Feel comfortable warmth
Feel sensation of relaxation
No sensation of burning
Feeling of slight oil on hands after removal of wax
Ultrasound
● High frequency sound wave converted to heat
● Can reach depths of 3-5 cm
● Coupling mediums used to help sound waves penetrate the skin
● Sound head moved in slow, circular pattern with contact at all times
Ultrasound
●
Two Types of Ultrasound
○
○
○
○
○
Thermal Effects
↑ collagen elasticity
↓ Joint stiffness
↓ Pain and spasm
↑ Blood Flow
Effects can last up to 1 hour after 5 minute tx.
●
○
○
○
○
○
Mechanical Effects
↑ Nerve conduction
Cell permeability altered from pressure changes
Mineral deposits dissolved
Micromassage
Protein synthesis promoted
Ultrasound
● Depths of Ultrasound
○ 1Mhz Frequency: depth of penetration = up to 5 cm
○ 3Mhz Frequency: depth of penetration = 1-2 cm
Ultrasound
Ultrasound Rate of Heating per Minute
Intensity
(W/cm²)
0.5
1
1.5
2
1 Mhz
.04º C
.2º C
.3º C
.4º C
3 Mhz
.3º C
.6º C
.9º C
1.4º C
Ultrasound~ Suggested Uses
● 1Mhz for deep tissue
● 3Mhz for shallow tissue
● Treatment time should be 5-10 minutes depending on area being treated
● Ultrasound treatments not performed more than one time per day
Phonophoresis
● Combination of ultrasound and medication driven into the skin through sound waves
● Usually anti-inflammatory medication
● Time and technique same as regular ultrasound
Electric Modalities
● Use of electricity to influence healing by stimulating the body tissues
Guidelines for Electrical Modalities
● Follow all MD guidelines
● Explain procedure to the patient
● Expose and clean area to be treated
● Place electrodes in appropriate place
● Use equipment as prescribed
● Never use on an open wound
Electrical Stimulation
● Effects:
○ Management of pain through gate control theory
○ Increase in deep blood flow and lymphatic drainage
○ Slight increase in circulation
○ Muscle relaxation
Electrical Stimulation
●
○
○
○
○
○
○
Indications:
Pain
Edema
Spasm
Hematoma
Trigger Point
Early muscle reeducation
●
○
○
○
○
○
○
Contraindications:
Metabolic diseases
Children
Pacemaker
Tumor
Fever
Irritated skin
Clinical Application
●
●
●
●
Follow MD recommendations for dosage
Treatment time should be 15-20 minutes
Each person has different levels that they can tolerate, use the athlete as the guide
Athlete should feel a comfortable ‘moving’ tingling zone in the area around the treatment pads
Iontophoresis
●
●
●
●
Use of ions to penetrate medicine into the injured area
1 cm penetration of medicinal ions
○
○
○
Numbing effect
Advantageous over Injectable:
No chance of infection
No tissue trauma
Medication is only thing going through skin
Iontophoresis
●
○
○
○
○
○
○
Indications:
Trigger points
Tendonitis
Superficial inflammatory conditions
Plantar Warts
Myositis
Bursitis
●
○
○
○
○
○
Contraindications:
Superficial metal implants
Pacemaker
Allergy to drug being used
Acute injury
Anesthetic skin
Clinical Application
● Must have a prescription for use of medicine
● Follow MD guidelines for dosage
● Must use appropriate medicines
● Athlete should feel some pain relief
● Athlete should not feel ‘hot pin’ sensation
Diathermy
● High frequency electrical current to heat the body’s tissue
● Bigger machines, not popular
Diathermy
●
○
○
○
Indications:
Chronic sprains/strains
Limited ROM
Sub-acute inflammations
●
○
○
○
○
○
○
Contraindications:
Acute inflammatory injuries
Hemorrhages
Casts
Metal implants
Screws
Pregnant women
Clinical Application
● Sound heads placed around the area being treated
● Remove all metal from area
● Cover the area with 2 layers of towels
● Should feel like a ‘ray of sunshine’ on the skin
● Heats tissues to 104-112ºF at about 2 inches from skin’s surface